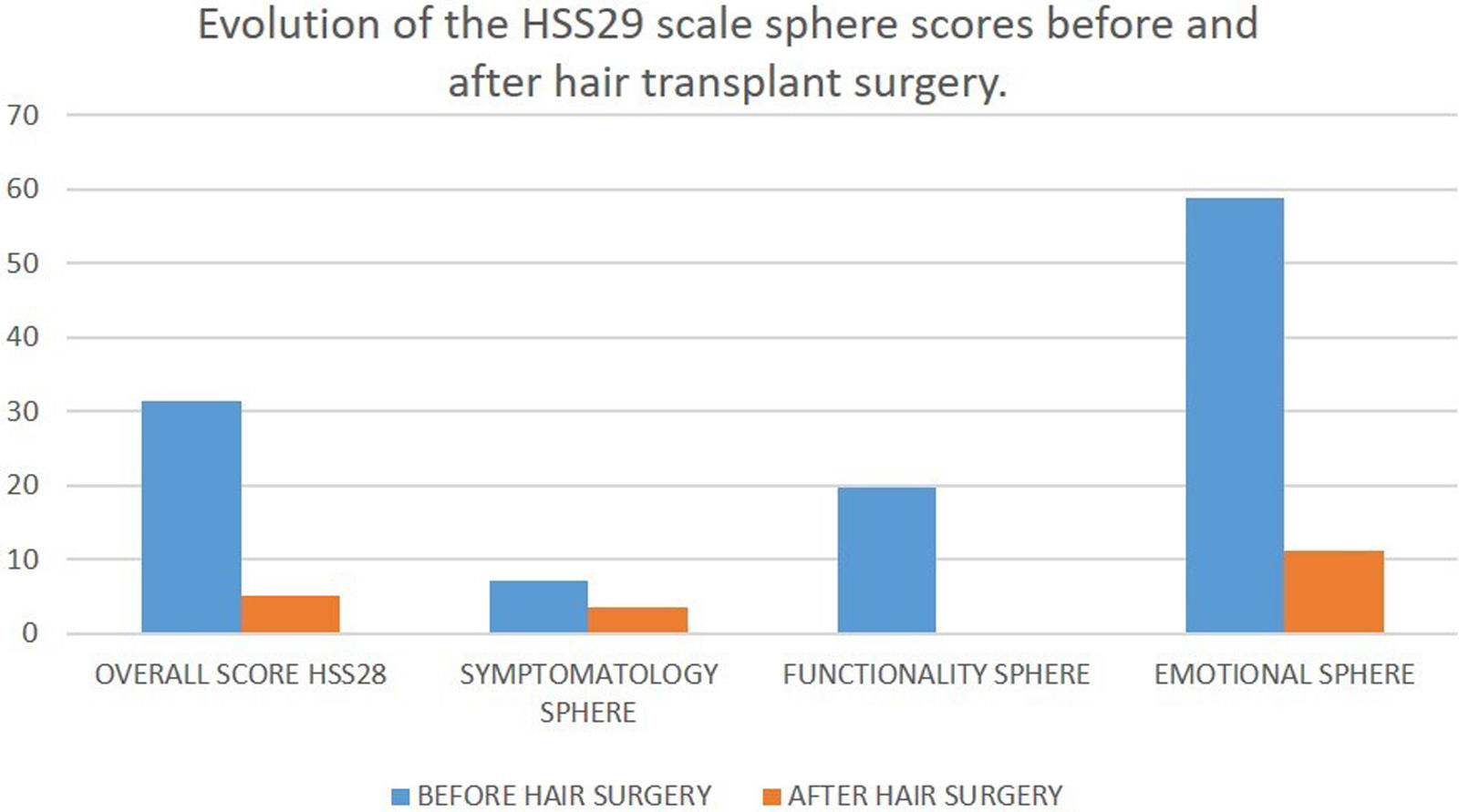
Androgenetic alopecia is the most common cause of non-scarring alopecia in women.1 Treatment options approved are limited to topical minoxidil.1 Hair transplantation is a minimally invasive surgery, consisting of the transfer of non-miniaturized follicular units from the donor area to the alopecic site, preserving their original calibre based on the “donor dominance” theory.2 A total of 95% of hair surgical procedures are performed in male AGA patients; however, women with alopecia may experience greater societal pressure compared with men.3 Recently, the HAIR SPECIFIC INDEX 29 (HSS29) scale has been validated in Spanish to quantify the repercussion of AGA on quality of life across 3 different spheres (symptomatology, functionality and emotions).4 The HSS29 scale includes a 29-item questionnaire whose response score go from 1 up to 5 and are, later, transformed into a linear scale from 0 up to 100.5,6 We conducted a related-group analytical retrospective observational cohort study to evaluate the degree of psychological impacts in women with AGA before and after hair transplantation, and included a total of 17 women (mean age, 54.6 years) with clinical and trichoscopic diagnosis of AGA who underwent surgery from December 2019 through April 2022 using the follicular unit excision (FUE) technique. All patients had been on medical therapy for, at least, 6 months. The Spanish-validated HSS29 questionnaire was administered to all patients before and, at least, 6 months after surgery (median, months; IQR, 6–12). In addition, they were asked 3 questions on the degree of satisfaction with the surgery (scores from 1 to 10) and were instructed to rate the degree of perceived improvement in their alopecia (−2, noticeable worsening; −1, slight worsening; 0, no change; +1, slight improvement; +2, noticeable improvement). The mean number of follicular units transplanted was 1900, with a shaved window in the donor site and no shaving in the recipient site. The statistical analysis was conducted using IBM SPSS version 26.00. All quantitative variables were estimated using measures of central location (median) and dispersion (interquartile range, IQR). Normality of data was assessed using the Shapiro–Wilk test. The non-parametric Wilcoxon signed-rank test was used for the symptom and functional spheres, while the Student's t-test was used for the emotion sphere (normally distributed data). All HSS29 values are shown in Table 1 and were considered statistically significant at p<0, 05. Of note the large decrease in some of the scoring spheres, with significant statistical values in the emotional sphere, which dropped from a median of 58.75 points (IQR, 27.5–76.25) prior to the intervention down to 11.25 points (IQR, 5–28.75) after the intervention, and in the functional sphere, which dropped from a median of 19.79 points (IQR, 6.25–38.55) down to 0 points (IQR, 0.2–2.09). Both decreases show the relevant improvement in our patients’ emotional situation and everyday activities after hair surgery and are reflected in the overall decrease of the HSS29 scale score from a median of 31.47 points (IQR, 12.07–40.06) down to 5.17 points (IQR, 3.02–12.93) with p<0.001 (Fig. 1). The overall satisfaction score with the surgery had a median of 9 points (IQR, 7.5–10). The questions “Would you perform the surgery again?” and “Would you recommend the surgery to another woman?” obtained a median score of 10 (IQR, 8–10 and 8.5–10, respectively). The degree of improvement was scored as marked improvement (+2) in 10 cases, slight improvement (+1) in 5, and no changes (0) in 1. One patient did not respond to the post-transplant survey. The main limitation of this study is the size of the sample. AGA implies functional limitations and a great emotional impact in affected women. The overall HSS29 score obtained prior to the surgery was ranked as moderately affected and severely affected in the emotional sphere. Questions, such as question #8 (“I tend to stay at home because of my alopecia”) or question #24 (“My alopecia affects my desire to be with people”) bring us closer to the reality of these patients. The significant changes achieved in the questionnaires after hair transplantation, a minimally invasive surgery with exceptional complications, and the degree of improvement perceived by the treated patients should lead us to evaluate this treatment option in a greater number of patients. Hair transplantation is an effective treatment for female AGA (Fig. 2). We expect to see a wider use of this surgical procedure in women in the coming years.
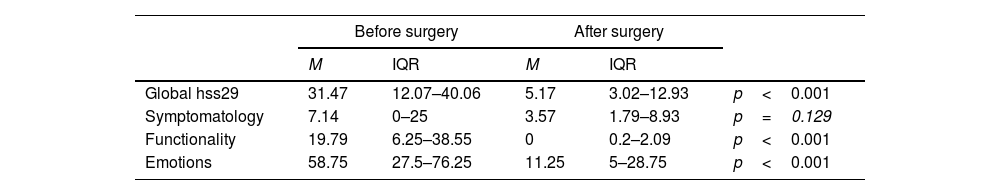
HSS29 scale scores before and after hair transplant expressed as median and interquartile range (IQR).
| Before surgery | After surgery | ||||
|---|---|---|---|---|---|
| M | IQR | M | IQR | ||
| Global hss29 | 31.47 | 12.07–40.06 | 5.17 | 3.02–12.93 | p<0.001 |
| Symptomatology | 7.14 | 0–25 | 3.57 | 1.79–8.93 | p=0.129 |
| Functionality | 19.79 | 6.25–38.55 | 0 | 0.2–2.09 | p<0.001 |
| Emotions | 58.75 | 27.5–76.25 | 11.25 | 5–28.75 | p<0.001 |
Of note the statistical significant decrease in the overall score of the questionnaire and functionality and emotions spheres. Hair transplant is associated with an improvement in the quality of life of female patients with androgenetic alopecia.
HSS29: Hair Specific Index 29; IQR: interquartile range; M: median.
Progression of the HSS29 scale sphere scores (before and after), at least, 6 months following the hair transplant (median, 9 months). Data presented are expressed as the medians in the global score and each of the spheres of the HSSS29 scale. Except for the symptomatology sphere, the lower scores reported were statistically significant (p<0.01). The symptomatology sphere is not very relevant in androgenetic alopecia, because it is not a condition usually associated with pruritus or trichodynia. However, after hair surgery, these symptoms were gone, which confirms the absence of adverse local effects associated with the intervention.