Burn scars cause high morbidity in the form of contractures, body disfigurement, and itching, as well as a high emotional impact that adversely affects patient quality of life. Laser therapy has proven effective in this setting. It is superior to topical treatments and can be used in conjunction with surgery, helping to reduce morbidity. The use of lasers in hospital dermatology departments, however, is still limited. Carbon dioxide laser is the most widely used device for reducing scar thickness, improving textural abnormalities, and treating associated contractures, which may restore the mobility of these patients when it is altered. Pulsed dye laser treatments are particularly useful for reducing erythema in recent burn scars and preventing subsequent hypertrophy. Pigment laser treatments with short pulse durations (nanoseconds or picoseconds) can improve hyperpigmentation. In this article, we review the evidence for the use of laser therapy for burn scars and propose a treatment algorithm.
Las cicatrices por quemadura suponen una elevada morbilidad en forma de contracturas, desfiguración corporal y prurito, así como un elevado impacto emocional que disminuye la calidad de vida de estos pacientes. Los dispositivos láser se han mostrado eficaces para su tratamiento, por encima de los tratamientos tópicos y complementarios a la cirugía, sin generar tanta morbilidad. Sin embargo, su uso en los departamentos de dermatología hospitalarios todavía está poco extendido. El láser más utilizado es el láser CO2 para tratar el grosor de la cicatriz, alteraciones texturales, y la posible contractura asociada, restaurando la movilidad de estos pacientes cuando se encuentra alterada. El láser de colorante pulsado es especialmente útil ante las cicatrices de quemaduras recientes con componente eritematoso y para prevenir el desarrollo de cicatrices hipertróficas posteriores. La hiperpigmentación puede mejorar con láseres de pigmento en modalidades de pulso corto (nano- y picosegundos). Revisamos la evidencia de estos dispositivos para el tratamiento de las cicatrices por quemaduras y aportamos una propuesta de algoritmo terapéutico.
Laser devices have proven very useful for the treatment of scars.1 Lasers have been widely studied in specific types of scar, such as those resulting from acne, surgery, and injury, as well as keloids.1,2 However, laser treatment for the sequelae of burns has received less attention, and the option is not available in most hospitals.
In 2017, the worldwide prevalence of burn injuries exceeded 1000 per 100000 inhabitants. Most burns affected <20% of the body surface and mainly involved the skin, thus highlighting the role of the dermatologist.3
Complications resulting from burn scars can have a considerable effect on patient quality of life.4 Contractures and disfigurement have a huge impact on function, reduce mobility, and cause pain and itching. Moreover, the strong emotional component associated with this type of lesion can be stigmatizing, especially in lesions affecting the face and neck, and lead to anxiety, depression, and low self-esteem.5
A variety of conservative treatments have traditionally been administered to manage burn scars, including silicone gel, corticosteroid injections, pressure therapy, and therapeutic massages.6 These approaches must often be combined with surgery, which can range from resection of the scar with closure of the wound to transverse incision, Z-plasty, flaps, and skin grafting.7
LasersIn recent years, lasers have proven effective in the treatment of burn injuries. They are minimally invasive, carry a low risk of adverse effects, and are associated with rapid recovery. Therefore, they are included in some treatment protocols alongside modestly successful conservative approaches and surgical interventions, which may be very effective but are associated with high morbidity.8 While lasers do not necessarily replace surgery, they can reduce the area to be treated, thus leading to fewer postsurgical complications.9
Lasers are classified according to their mechanism of action as ablative/nonablative and fractional/nonfractional.10 The main devices used in the treatment of burn scars are summarized in Table 1.
Main Scar Abnormalities and Lasers Available for Treatment.
| Abnormality | Laser |
|---|---|
| Erythema | 585- and 595-nm PDL, 500- to 1200-nm IPL, 1064-nm Nd:YAG (ms), 532-nm KTP (ms) |
| Thickness | AFL10600-nm carbon dioxide2940-nm Er:YAGNAFL1540- and 1550-nm Er:glass |
| Flexibility | 10600-nm carbon dioxide |
| Pigmentation | AFL, NAFL, QS 755-nm alexandrite, QS 1064-nm Nd:YAG, QS 694-nm ruby, QS 532-nm KTP |
Abbreviations: AFL, ablative fractional laser; IPL, intense pulsed light; KTP, potassium-titanyl-phosphate; LADD, laser-assisted drug delivery; ms, milliseconds (long pulse); NAFL, nonablative fractional lasers; Nd:YAG, neomydium: yttrium-aluminum-garnet; PDL, pulsed dye laser; QS, Q-switched (nanoseconds/picoseconds, short pulse).
This article covers the parameters most commonly applied for the treatment of burn scars and could prove useful for guidance only. Importantly, these parameters differ widely owing to the heterogeneous nature of the scars themselves and the wide variety of devices available (Table 2).
Main Lasers for the Treatment of Burn Scars: Grade of Recommendation and Level of Evidence.
| Laser | Grade of recommendation | Level of evidence |
|---|---|---|
| 10600-nm carbon dioxide | A | I |
| 585- and 595-nm PDL | B | I |
| 1540- and 1550-nm Er:glass | B | II |
| 755-nm alexandrite | C | III |
Abbreviations: Er, erbium; PDL, pulsed dye laser.
Burn scars generally result in abnormal healing of the skin in more than 70% of cases owing to abnormalities in thickness, texture, erythema, and pigmentation.11 Such is the case of burns affecting the deep layers of the dermis, for example, second- or third-degree burns, which may require laser treatment. Superficial burns that do not reach the reticular dermis rarely lead to abnormal scarring and do not generally cause complications.12
In terms of thickness, the scars can be classified as keloids, hypertrophic and atrophic scars; in terms of pigmentation, they can be classified as hypopigmented and hyperpigmented regarding adjacent healthy skin. Furthermore, erythema is common, especially in active and recent scars.11
The severity of the scar should be assessed before initiating and monitoring therapy. The most common approach is the Vancouver Scar Scale,13 which evaluates vascularization, thickness, flexibility, and pigmentation. However, the Patient and Observer Scar Assessment Scale (POSAS) is considered the most complete, since it also includes subjective symptoms, such as pain and itching.14 Appropiate evaluation allows selecting the most suitable laser for treatment. Moreover, in order to choose the right type of device and parameters, we must take into account both the characteristics of the patient (e.g., skin phototype, comorbidities) and the location of the scar (e.g., head, neck, limb).
Vascular LasersPulsed dye lasers (PDLs) are nonablative vascular lasers with wavelengths of 585 and 595nm.15 Using selective photothermolysis, they cause coagulation and necrosis of the blood vessels, with oxyhemoglobin as the target molecule (chromophore).16 PDLs are considered the laser of choice for treating the vascular component of burn scars and carry a low risk of adverse effects.
Multiple studies have shown PDLs to be effective for the treatment of scar erythema, which is caused by excess neovascularization during the scarring process.17 It has also proven effective for the treatment of hypertrophic scars through destruction of collagen secondary to tissue hypoxia caused by coagulation of the vessels.18 Allison et al.19 also recorded an improvement in itching after treating the vascular component. While not fully defined, this mechanism is thought to be associated with a change in cytokines, neuropeptides, and histamine resulting from hypoxia and local heat after laser treatment.
Fluence is generally low, 4–8J/cm2, with a beam diameter (spot size) of 7–10mm and short pulse duration (0.5–2ms).8 The endpoint, or immediate desired effect, is mild purpura, since overtreatment can lead to pigmentation abnormalities. Patients with skin phototypes I-III are the best candidates for PDL because they have less melanin, which competes with hemoglobin for the absorption of energy. Treatment is usually administered in sessions separated by a 6- to 8-week interval until the desired therapeutic effect is achieved. A mean of 4 sessions is normal.15
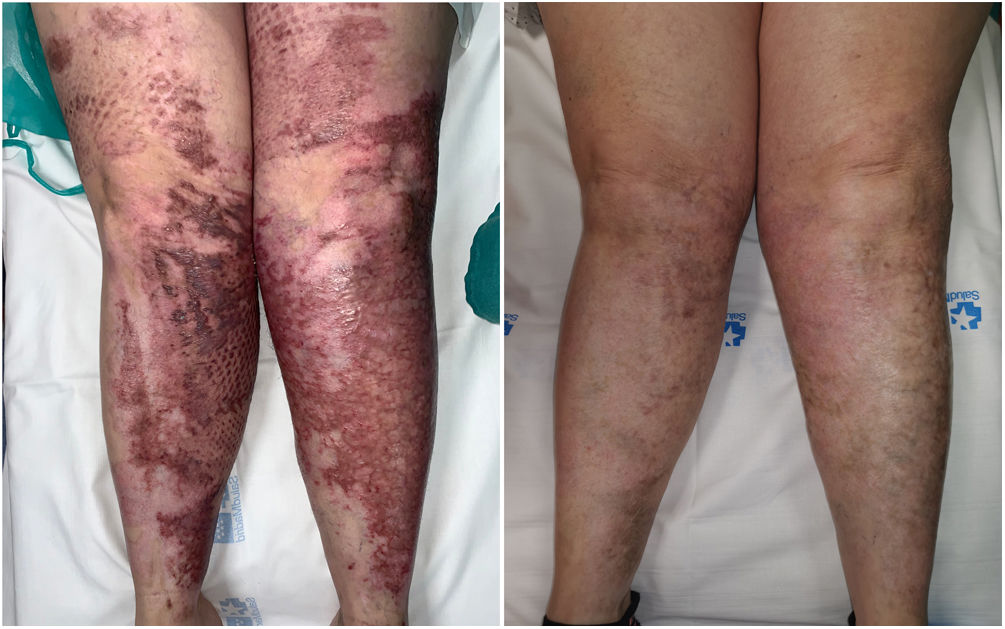
The fact that the laser penetrates approximately 1.2mm into the skin means that its use in thick hypertrophic scars is limited. Therefore, it is frequently combined with ablative fractional lasers (AFLs) in thick scars to generate a potentially synergic effect.15 We have found that pediatric patients generally have poor tolerance to AFL treatment and that PDL in monotherapy has very good results, especially in the early phases of scarring (Fig. 1).
In a clinical trial, Al-Mohamady et al.20 demonstrated that the long-pulse, low-fluence 1064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser was effective for the treatment of hypertrophic scars, observing no significant differences with respect to PDL.
Finally, intense pulsed light lasers emit a broad-spectrum polychromatic light beam (500–1200nm) that can be delimited using filters and act on various types of chromophores by means of selective photothermolysis.21 These devices can also prove useful for the treatment of the vascular component, pigmentation, and hypertrophy in various types of scar, such as burn scars, and can be a good alternative. However, evidence for their use in the treatment of burn scars is limited.22
Ablative Fractional LasersAFLs are the cornerstone of burn scar treatment. The most common are the 10600-nm carbon dioxide laser and the 2940-nm erbium-doped yttrium aluminum garnet (Er:YAG) laser, which use water as a chromophore. They act by generating columns of thermal damage in the epidermis and dermis. These columns favor collagen remodeling, thus improving the thickness, flexibility, and color of the scars. They vary in depth from 0.2 to 4mm. Furthermore, the healthy tissue between the columns serves as a reservoir for rapid posttreatment recovery.23
Carbon dioxide lasers have less affinity for water than Er:YAG lasers and generate more thermal coagulation in peripheral tissue. Given that this mechanism facilitates collagen repair, the carbon dioxide laser is considered the more effective and is more widely used. In addition, carbon dioxide lasers deposit energy at a greater depth, up to 4mm, and their role in vessel coagulation prevents some bleeding during treatment.8
Recent meta-analyses show that the use of fractional carbon dioxide lasers significantly improves the thickness, flexibility, vascularization, and pigmentation of burn scars, and even associated pain and itching.24,25
Depending on the characteristics of the scar, the laser can be applied superficially to smoothen the skin and deep to reduce tension and favor remodeling of abnormal collagen. It can even be used in combination26 (Fig. 2).
The parameters applied in AFLs vary considerably and are adjusted to the characteristics of the scar and the patient's skin phototype. For example, more hypertrophic scars tend to be treated at higher energy levels in order to act at greater depths, albeit with lower densities to compensate for excessive thermal damage. The most common parameters used are intermediate-high powers (15–30W) and low densities (5%–15%). Darker skin phototypes require more conservative approaches in order to prevent hyperpigmentation. Treatment is usually administered in a mean of 3–5 sessions over 4–12 weeks.27
The carbon dioxide laser has been used in its continuous nonfractional mode (traditional mode) to reduce tension and increase mobility in hypertrophic scars associated with contractures, mainly around joints. This procedure consists of incisions made perpendicular to the most prominent part of the contracture or in the form of the Mercedes Benz car logo in cases of extensive scarring, leaving the wound to heal by secondary intention.28
AFLs can also be used in atrophic scars resulting from reduced dermal collagen in order to stimulate new collagen production.29
Treatment with AFLs is generally well tolerated, with few adverse effects, which, when they do occur, are usually mild. Reported complications, in order of frequency, include hypopigmentation, pain and inflammation, prolonged erythema, vesicles, paradoxical growth of scar tissue, and infections.27
Nonablative Fractional LasersNonablative fractional lasers (NAFLs) cause heat damage in the dermis in the form of columns of coagulation without ablation, leaving the epidermis intact.10 This mechanism makes it possible to reduce surface damage and the degree of heat applied to the skin; therefore, recovery time is shorter.26 The most commonly used type is the 1540-nm or 1550-nm Er:glass laser.
NAFLs heat the skin to a lower temperature (50–70°C) and reach lower depths (approximately 1.8mm) than AFLs.8 Despite the paucity of studies comparing the 2 lasers for treatment of scars, NAFLs cause less thermal damage and are therefore less effective and require more sessions.26,30
In a clinical trial, Taudorf et al.31 found an improvement in the thickness, flexibility, and roughness of burn scars, as well as normalization of collagen in histology, albeit at the expense of reduced effectiveness in hypertrophic scars.
Pigment LasersThe main pigment lasers are the 694-nm ruby laser, the 755-nm alexandrite laser, and the 1064-nm and 523-nm potassium-titanyl-phosphate (KTP) lasers in Q-switched mode (nanoseconds or picoseconds).32 Although these are widely used to treat dyschromia in several types of scar,33 we found no studies specifically assessing their use in burn scars. Management of pigment abnormalities is generally complex, and recurrences are frequent.
Ablative lasers that use water as a chromophore (e.g., carbon dioxide lasers) are commonly applied to treat textural abnormalities, although they can also be used to nonselectively eliminate hyperpigmentation through vaporization of melanin in the epidermis. Lasers that use melanin as a chromophore, however, are more specific, since they selectively destroy melanosomes in keratinocytes and melanocytes, thus limiting collateral thermal damage in peripheral tissue.32 Furthermore, topical depigmenting treatments combined with rigorous photoprotection are essential for management of postinflammatory hyperpigmentation.32
In our experience, pigment lasers such as the short-pulsed 755-nm alexandrite laser provide good results (Fig. 3). We propose low fluence values (1–3J/cm2) to improve tolerance at pulses measured in nanoseconds or picoseconds with a spot size of 3–5mm.
Finally, AFLs and NAFLs have led to some improvement in hypopigmentation, possibly owing to migration of normal melanocytes from peripheral tissue.34
Combination Laser TherapyGiven that burn scars are frequently characterized by abnormalities in thickness, texture, erythema, and pigmentation, combining several lasers makes for more complete and specific therapy. Clinical trials have shown more favorable outcomes with the combination of treatments, especially PDL and carbon dioxide laser.35,36
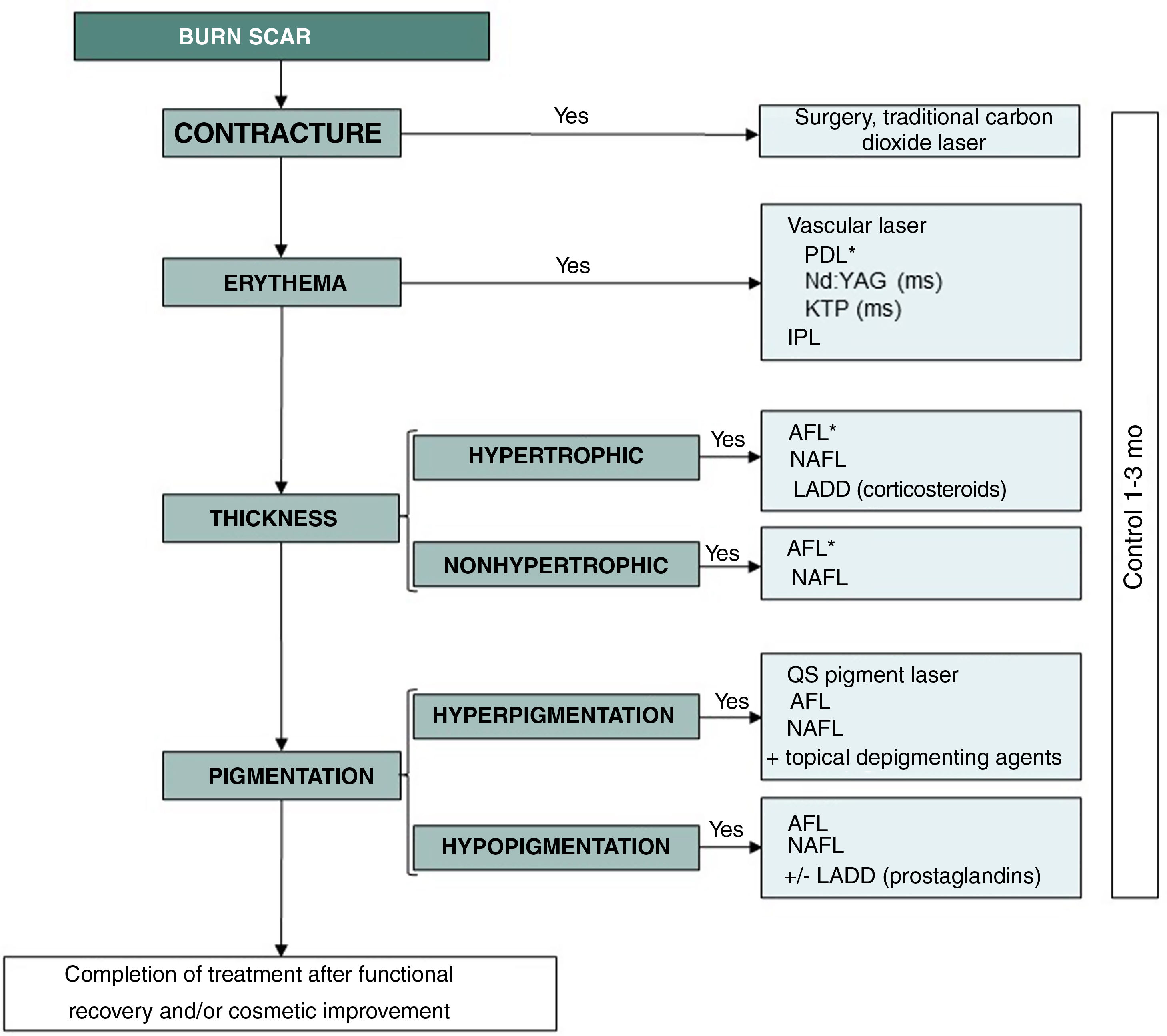
Anderson et al.8 propose a therapy plan including initial application of PDL for treatment of erythema and inflammation, followed by combination with AFL to improve thickness and texture. In our experience, scars with abnormal pigmentation or hypertrichosis can also be treated by combining lasers whose chromophore is melanin, such as the 755-nm alexandrite laser and the 1064-nm Nd:YAG laser. We propose a therapeutic algorithm for the management of burn scars based on a review of the literature and our professional experience (Fig. 4).
Algorithm for the treatment of burn scars. *Laser of choice. IPL indicates intense pulse light; PDL, pulsed dye laser; Nd:YAG, neodymium-doped yttrium aluminum garnet; KTP, potassium-titanyl-phosphate; AFL, ablative fractional laser; NAFL, nonablative fractional laser; QS, Q-switched (nanoseconds or picoseconds); LADD, laser-assisted drug delivery.
Applying adjuvant treatment to laser treatment can generate a synergistic effect in the management of burn scars. An improvement in hypertrophic scars has been observed when PDL is combined with intralesional corticosteroids, mainly triamcinolone, and 5-fluorouracil.37
Laser-assisted delivery of corticosteroids is an increasingly used and promising modality. This approach is based mainly on fractional Er:YAG laser and carbon dioxide laser. The underlying mechanism involves delivery of the drug via the columns generated in the epidermis, thus increasing its ability to act.38 The main advantage of this modality is that the topical treatment delivered is better tolerated than intralesional corticosteroids. The drug usually administered is triamcinolone at 10–40mg/mL. This modality generally requires low laser densities (<5%) and energies that vary depending on the thickness of the scar.39,40
Administration of prostaglandins such as latanoprost and bimatoprost after fractional laser treatment recently led to significant improvements in hypopigmentation. This phenomenon is probably due to the increased transfer of melanosomes in melanocytes to basal keratinocytes. Adjuvant topical retinoids, which have traditionally been used to treat postinflammatory hyperpigmentation, have also been used to restore pigment through modulation of tyrosinase activity.41
Platelet-rich plasma,42 autologous fat grafting,43 and radiofrequency36 may also prove useful.
When to TreatOnce the burn injury has completely healed, early intervention on the scar makes it possible to alleviate symptoms, prevent contractures, and improve the recovery process.8 While the ideal time to start treatment of burn scars has not been defined, PDL, AFL, and NAFL applied to surgical scars on the day the sutures are removed have proven safe and effective.44,45
Erythematous and hypertrophic scars are common, especially during the first year of healing. Therefore, early treatment with vascular lasers plays a major role and can even prevent complications.46 In some patients, especially those with low skin phototypes (I–II), erythema can become chronic. PDL has also proven successful in the treatment of lesions that have progressed over several years.47
ConclusionsBurn scars are generally associated with considerable morbidity. Lasers, especially PDLs and carbon dioxide lasers, have proven effective for improving erythema, hypertrophy, pigmentation, flexibility, and itching, with a low risk of adverse effects and rapid recovery time. We believe that implementing laser treatment in the management of these lesions would go a long way to improving patients’ quality of life.
FundingThe authors declare that no funding was received for the present article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.