The use of drugs to sustain sexual activity for prolonged extended periods of time is known as chemsex. It is more common among men who have sex with men. Sex sessions (SS), known as “chills” or “parties,” can last from a few hours to several days. The most widely used drugs are gamma-hydroxybutyric acid (GHB), mephedrone, crystal methamphetamine (tina), and cocaine. The IV administration of drugs during SS is known as slamsex, slam, or slamming.1–3
Mephedrone, also known as “cactus food,” “bath salts,” “meow,” or “CatMef,” is a synthetic drug derived from cathinones.4 It is one of the most popular alternatives to other psychostimulants such as cocaine or 3,4-methylenedioxymethamphetamine (MDMA, ecstasy) and is among the most widely used during chemsex.1,2 It can be administered orally, intranasally, or intravenously. When administered intravenously, peak effects occur within 5–10min and can go on for 15–30min. Due to the short duration of effects and rapid tolerance buildup, successive doses are consumed compulsively. Up to 10 injections per day can be administered during an SS.2,4
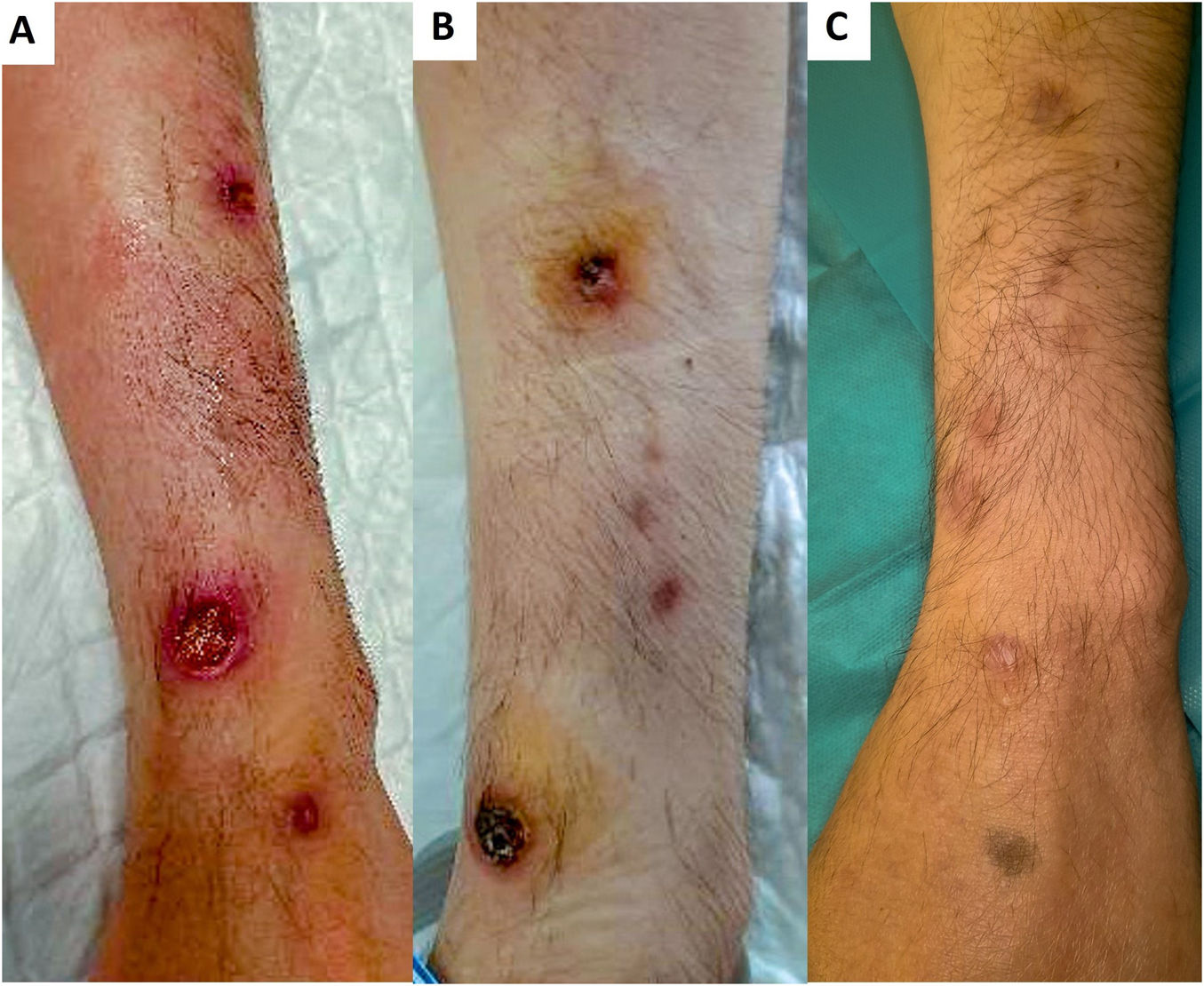
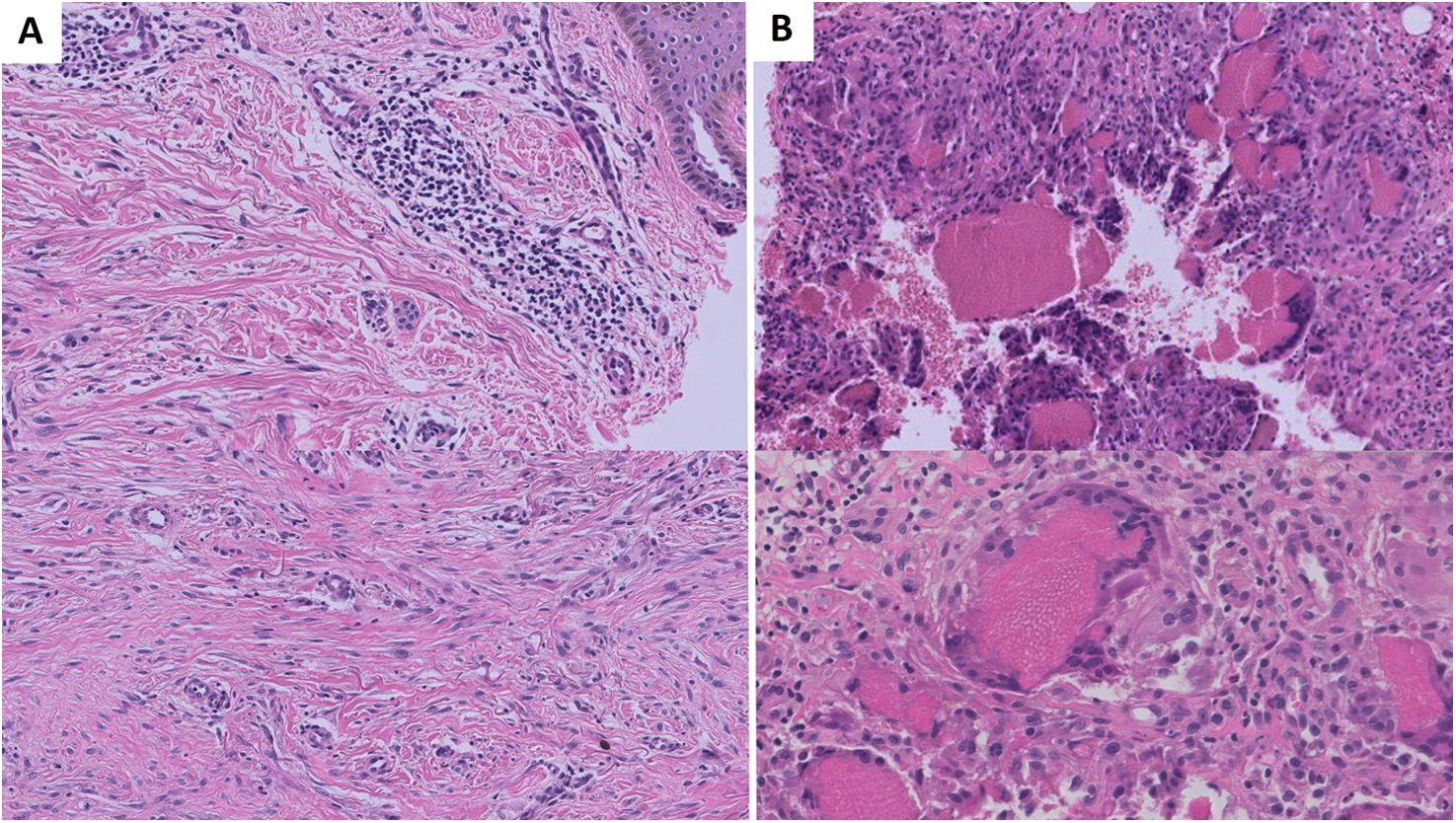
Case #1: A 30-year-old male with a history of HIV, past HBV infection, and secondary syphilis, with a practice of sex with men and slamsex with IV GHB and mephedrone, presented with a 1-month history of painful lesions on the left forearm, which appeared after mephedrone injection. He presented with 2.1cm and 1.5cm rounded ulcers with erythematous–violaceous borders that developed a black crust, along with smaller violaceous macules<5mm on both forearms. He received topical treatment with betamethasone/gentamicin cream (0.5mg/g and 1mg/g), with complete healing in 2–3 weeks, leaving residual depressed scars (Fig. 1). Histology showed superficial scarring fibrosis and a foreign body giant cell reaction at the dermis-subcutaneous junction. No signs of vasculitis or intravascular thrombi were reported (Fig. 2). Techniques for microorganisms and direct immunofluorescence all tested negative.
Cases #2 and #3: A couple of 2 men, aged 39 and 40, with a history of HIV infection and slamsex practice presented to the ER with ulcers similar to those described in Case #1, located on the upper and lower extremities after mephedrone administration in an SS. Antibiotic therapy was indicated due to suspected abscesses. Follow-up was not possible due to loss to follow-up.
Patients denied the use of other drugs and did not know whether the drug may have been adulterated. The first patient participated in multi-day SS with several injections per day. Patients 2 and 3 participated in 24-h SS and injected themselves 5–6times/day. The lesions appeared within the first week at the injection sites. They identified improper administration by the absence of immediate effects.
Cutaneous complications due to mephedrone injection are rarely documented. In 2018, Frances et al. described a case of necrosis on the tip of the thumb following the accidental intra-arterial injection of mephedrone.5 Recently, a patient with retiform purpura and a second patient with chronic, punched-out ulcers on both forearms as mephedrone injection-related complications have been described.6
Differential diagnosis includes complications described with other drugs. Cocaine-levamisole use can cause destructive lesions of the facial midline, autoimmune complications such as leukocytoclastic vasculitis, thrombotic vasculopathy with retiform purpura (bilateral lesions on lower limbs, trunk, auricular pavilions, and acral areas), or neutrophilic dermatoses (multiple pyoderma gangrenosum-like lesions).7,8 Infectious and non-infectious complications occur at injection sites, such as elbow creases, forearms, and legs. Infectious complications are a common finding in IV drug users, with 60% having a past medical history of infections, such as abscesses at puncture sites, cellulitis, or thrombophlebitis.8,9 Ecthyma gangrenosum is another condition to consider in necrotic ulcers.10 Chronic ulcers and sclerosis also develop at the injection sites. These lesions could be due to a dermal reaction to the drug or adulterants.8,9 The mechanism behind necrosis is unclear and may be multifactorial, due to vasospasm, drug embolism, thrombotic vasculopathy, or vasculitis.5,8,9 In our patients, thrombotic vasculopathy findings may not have been observed in subcutaneous tissue due to the shallow depth of the biopsy.
We present 3 new cases of cutaneous complications following mephedrone injection. These complications are likely underdiagnosed due to physicians’ lack of awareness of these practices and patients’ omission of information due to the associated stigma. Dermatologists must stay updated on these practices and the emergence of new drugs to recognize these complications.
FundingNone declared.
Conflicts of interestNone declared.