We read the quite enlightening article ‘MPOX (formerly monkeypox): review of the most relevant clinical, epidemiological, diagnostic and therapeutic aspects for the dermatologist’ by Catala et al. with great interest.1 The global outbreak of monkeypox has led to more than 15,000 cases being reported in non-endemic countries. This article is an addendum to the article published by the authors to differentiate similar looking lesions described in monkeypox, chickenpox, and COVID 19 for which literature is scarce. The World Health Organization (WHO) has recommended the use of the term ‘MPOX’—as opposed to monkeypox—to avoid the stigma associated with the term. It has also been reported in the United States in patients traveling from the endemic central and West Africa. In the absence of a history of travel to endemic countries, cases are being frequently seen in men who have sex with men (MSM).2
Monkeypox is a double stranded DNA virus of the poxviridae family. Respiratory droplets, fomites and direct contact are the main routes of transmission. The definition of a monkeypox case has been defined by the U.S. Centers for Disease Control and Prevention (CDC) (Table 1). The incubation period lasts between 5 and 21 days. Cases of monkeypox usually present as fever, rash and lymphadenopathy. Monkeypox rash is a monomorphic painful vesiculopustular lesion with early central umbilication and a prominent white rim surrounded by an erythematous halo over the face, extremities, trunk, genitals, palms and soles. It is imperative to differentiate the current Monkeypox outbreak from the pandemic of coronavirus disease 2019 (COVID-19).
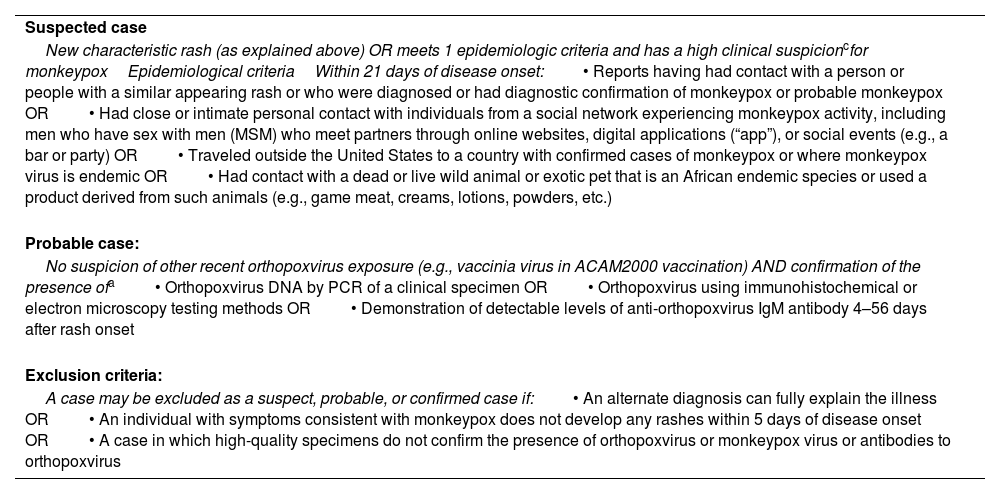
| Suspected case |
| New characteristic rash (as explained above) OR meets 1 epidemiologic criteria and has a high clinical suspicioncfor monkeypoxEpidemiological criteriaWithin 21 days of disease onset:• Reports having had contact with a person or people with a similar appearing rash or who were diagnosed or had diagnostic confirmation of monkeypox or probable monkeypox OR• Had close or intimate personal contact with individuals from a social network experiencing monkeypox activity, including men who have sex with men (MSM) who meet partners through online websites, digital applications (“app”), or social events (e.g., a bar or party) OR• Traveled outside the United States to a country with confirmed cases of monkeypox or where monkeypox virus is endemic OR• Had contact with a dead or live wild animal or exotic pet that is an African endemic species or used a product derived from such animals (e.g., game meat, creams, lotions, powders, etc.) |
| Probable case: |
| No suspicion of other recent orthopoxvirus exposure (e.g., vaccinia virus in ACAM2000 vaccination) AND confirmation of the presence ofa• Orthopoxvirus DNA by PCR of a clinical specimen OR• Orthopoxvirus using immunohistochemical or electron microscopy testing methods OR• Demonstration of detectable levels of anti-orthopoxvirus IgM antibody 4–56 days after rash onset |
| Exclusion criteria: |
| A case may be excluded as a suspect, probable, or confirmed case if:• An alternate diagnosis can fully explain the illness OR• An individual with symptoms consistent with monkeypox does not develop any rashes within 5 days of disease onset OR• A case in which high-quality specimens do not confirm the presence of orthopoxvirus or monkeypox virus or antibodies to orthopoxvirus |
Antibody and antigen detection methods are not confirmatory since orthopox viruses show serological cross-125 reactivity.
Monkeypox endemic countries: Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Ghana (identified in animals only), Côte d’Ivoire, Liberia, Nigeria, the Republic of the Congo, and Sierra Leone. Benin and South Sudan have documented importations in the past. Countries currently reporting cases of the West African clade are Cameroon and Nigeria.
The prevalence of papulovesicular rash in COVID-19 is 3.7% up to 15%.3 Two morphological patterns have emerged in COVID-19 vesicular exanthem: localized and a more common, widespread polymorphic pattern consisting of small papules, vesicles and pustules. Vesicular rash appears 3 days after the onset of systemic symptoms and disappears 8 days later, which suggests an earlier resolution than monkeypox rash.4 Moreover, vesicular exanthem in COVID-19 is characterized by small size, a frequently compromised trunk, and mild or absent pruritus while the monkeypox exanthem is characterized by painful, monomorphic, large size lesions, frequently involving the face, extremities, genitals, palms and soles. Several studies have confirmed the transmission of severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) through semen whereas no outbreaks of monkeypox in men who have sex with men (MSM) have ever been reported. However, the semen or vaginal fluid route of transmission is yet to be elucidated.5
Chickenpox rash tends to develop more rapidly than monkeypox and each lesion is less severe, less painful or not painful at all, and commonly associated with pruritus and evolving pleomorphically in a centripetal pattern compared with monkeypox rash, which exhibits monomorphic painful lesions evolving in a centrifugal pattern. Bilateral presentation in monkeypox is different from that of herpes zoster.
Diagnostic confirmation of monkeypox requires a positive lesion-based monkeypox-specific polymerase chain reaction assay. Broncho-pneumonia, encephalitis, ocular infections and sepsis are the most common complications of monkeypox disease, which has a self-limiting course within a matter of 2–4 weeks. Oral antivirals developed for smallpox such as brincidofovir and tecovirimat are available to treat monkeypox especially in immunocompromised patients. Smallpox vaccines have shown a 85% efficacy rate to prevent monkeypox.6 Similar vaccines may be used for post-exposure prophylaxis (PEP) if administered within a 96-h timeframe after exposure.
The dissemination of monkeypox in non-endemic countries means changes have occurred in the typical pattern of this disease, as well as a changing epidemiology. Of note the recent monkeypox outbreaks described in the context of the current COVID-19 pandemic, as well as the need to clinically recognize the disease early in a resource-poor settings. Further studies are required to understand whether the current monkeypox outbreak is an independent phenomenon or has been exacerbated by the COVID-19 pandemic.
Funding sourceNone.
Authors’ contributionsY.S. Pathania – Prepared and finalized the manuscript.
Conflict of interestNone.
Data availability statementNo new data were generated or analyzed in support of this research.