Cocaine and some of its main adulterants, such as levamisole, can cause multiple cutaneous and mucosal manifestations, including ischemic complications, neutrophilic dermatoses, midline destructive lesions, and vasculitis associated with antineutrophil cytoplasmic antibodies (ANCAs). Striking systemic symptoms are generally not seen. In all these conditions, positive test results may be observed for antinuclear antibodies, antiphospholipid antibodies, and various ANCAs, sometimes with characteristic staining patterns. Histology typically shows vascular changes, such as leukocytoclastic vasculitis, necrotizing vasculitis, and thrombi. We review the clinical, serologic, and histologic features of cutaneous and mucosal conditions associated with the use of cocaine and also look at pathophysiologic mechanisms, differential diagnoses, and treatments.
El consumo de cocaína, junto con algunos de sus adulterantes más frecuentes como el levamisol, puede provocar múltiples procesos cutáneos y mucosos, ya sean de índole isquémico, dermatosis neutrofílicas, lesiones destructivas de la línea media y vasculitis asociadas a ANCA, entre otros. Generalmente no se asocia clínica sistémica llamativa. Todos estos cuadros pueden presentar anticuerpos antinucleares, antifosfolípido y contra distintos antígenos de los neutrófilos, en ocasiones con un patrón característico. El estudio histológico suele mostrar cambios vasculares, como vasculitis leucocitoclástica, necrosis de la pared y trombos. En este artículo revisamos las características clínicas, serológicas e histológicas de estas entidades, junto con los mecanismos fisiopatológicos implicados, el diagnóstico diferencial y su tratamiento.
Cocaine is an alkaloid obtained from the leaves of the Erythroxylum coca plant. It is a central nervous system stimulant and a powerful vasoconstrictor and local anesthetic. According to a survey conducted in Spain in 2020, 2.5% of people aged 15 to 64 years consumed cocaine.1 The number of publications on mucocutaneous conditions associated with cocaine use has multiplied significantly since 2010.
Cocaine leaves mixed with ash or lime were chewed by the Incas for their moderate stimulant effects to reduce hunger and thirst and relieve fatigue, pain, and the effects of high-altitude and low-oxygen environments. Leaves have a low concentration of cocaine and are not addictive. Much more potent and highly addictive derivatives of cocaine produced at different processing stages appeared later, and include cocaine base paste, cocaine hydrochloride, and freebase cocaine, also known as crack. Cocaine hydrochloride is administered directly, either intranasally or intravenously (mixed with water), while cocaine base paste and freebase cocaine are smoked.2
Levamisole is an antiparasitic veterinary medication with immunomodulatory properties that was formerly used to treat autoimmune diseases and cancer in humans. It was withdrawn from the market due to adverse effects such as agranulocytosis, hepatotoxicity, and vasculitis. It is widely used as an adulterant in cocaine. It has been estimated that 80% of cocaine in the United States is adulterated with levamisole.3–5
We conducted a narrative review to analyze the pathophysiology, clinical manifestations, diagnosis, differential diagnosis, and treatment of different conditions associated with cocaine and its main adulterants. We conducted a literature search in PubMed and ScienceDirect using the terms skin, cutaneous, cocaine, and levamisole. We targeted publications in Spanish and English and focused on articles published since 2000 and reviews. We then searched the same platforms for articles on the conditions discussed in this review.
Pathophysiologic MechanismsVasoconstriction and NecrosisCocaine stimulates the sympathetic nervous system, leading to vasoconstriction and increased heart rate. It also acts on blood vessels by stimulating the release of endothelin 1, a powerful vasoconstrictor, and inhibiting the production of nitric oxide, the main vasodilator produced by endothelial cells. It causes direct endothelial damage, enhances platelet aggregation, and induces a prothrombotic state.6
The above effects decrease vascular blood flow, generating both systemic ischemia (notably myocardial infarction and cerebral ischemia)and local ischemia. Local ischemia leads to necrosis of the intranasal mucosa and can even affect deep osteocartilaginous structures and cause anatomic cocaine-induced midline destructive lesions (CIMDLs).
Nonischemic mechanisms have also been purported to have a role in CIMDLs. Examples are direct trauma caused by cocaine crystals impacting the mucosa at high speed,7 antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis,8 and inflammation induced by Staphylococcus aureus superantigens,9 which colonize the mucosa of most patients with CIMDLs. None of these mechanisms, however, have been demonstrated. Trimarchi et al.10 identified the expression of genes related to apoptosis, autophagy, tissue regeneration, cell proliferation, collagen integrity, and DNA damage response in nasal epithelial cells exposed to cocaine, indicating another potentially significant pathway in the pathogenesis of CIMDLs.
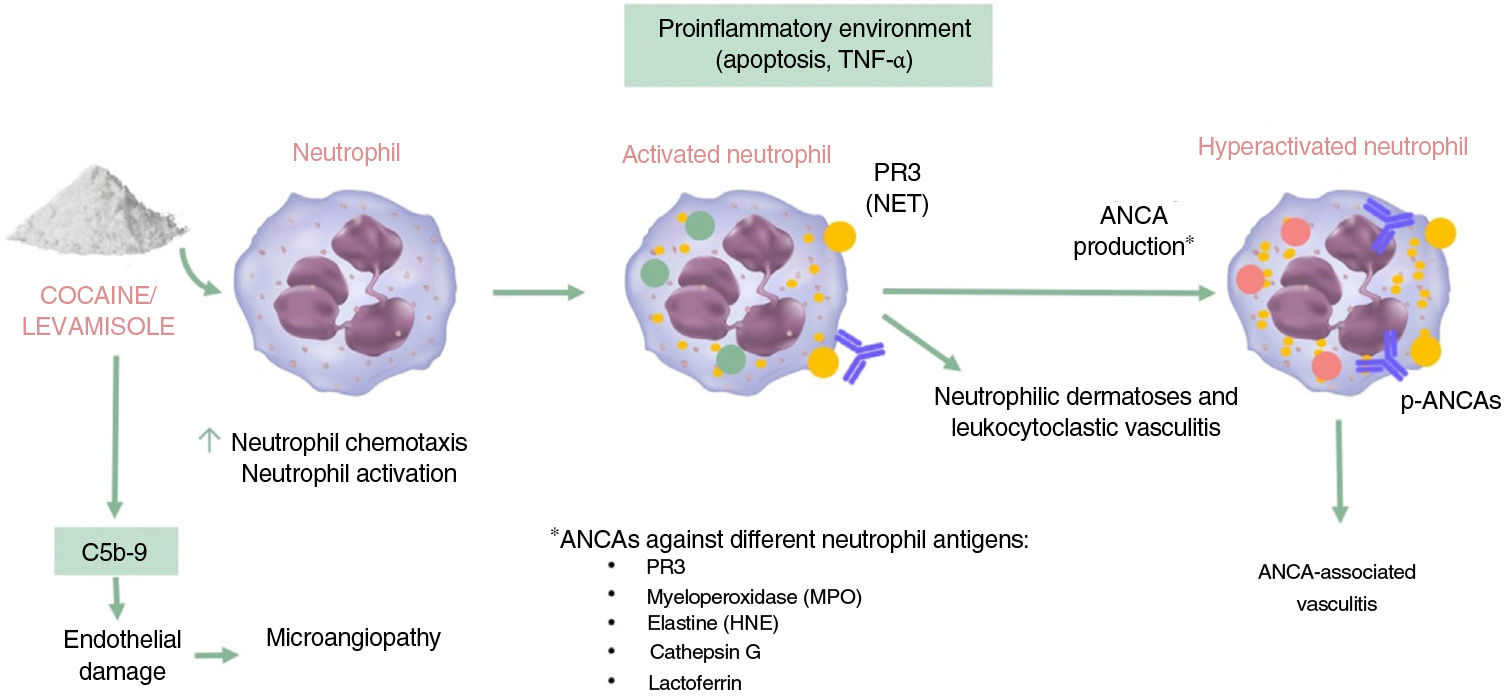
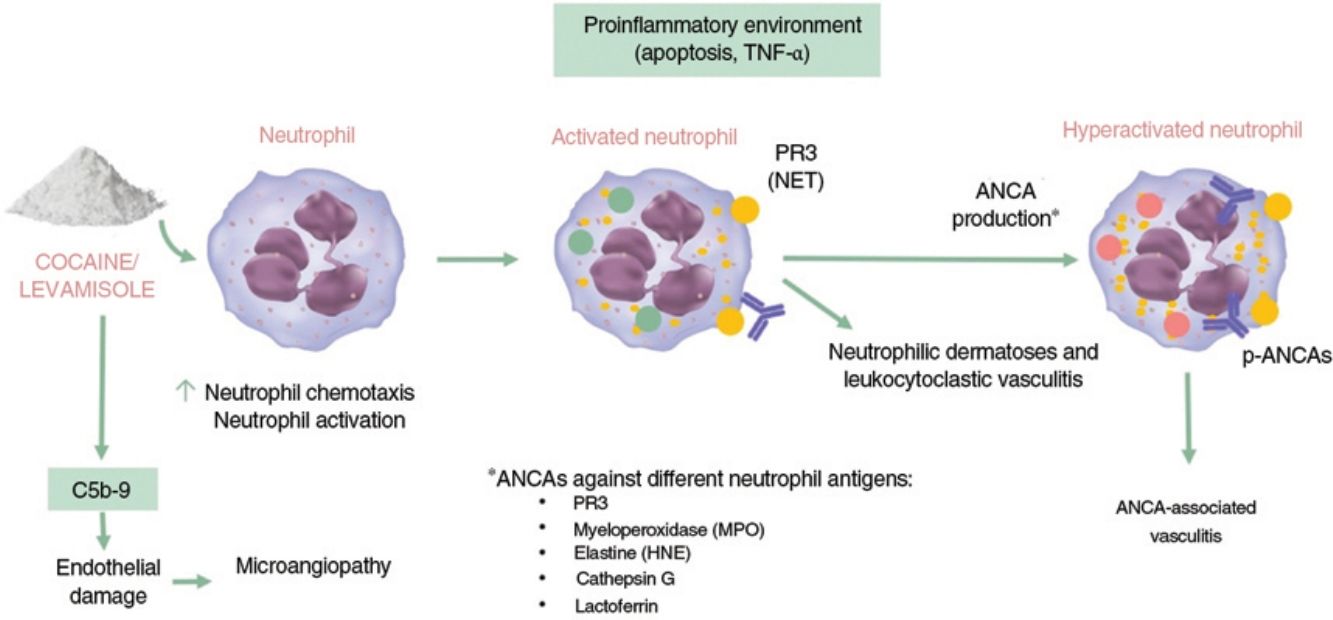
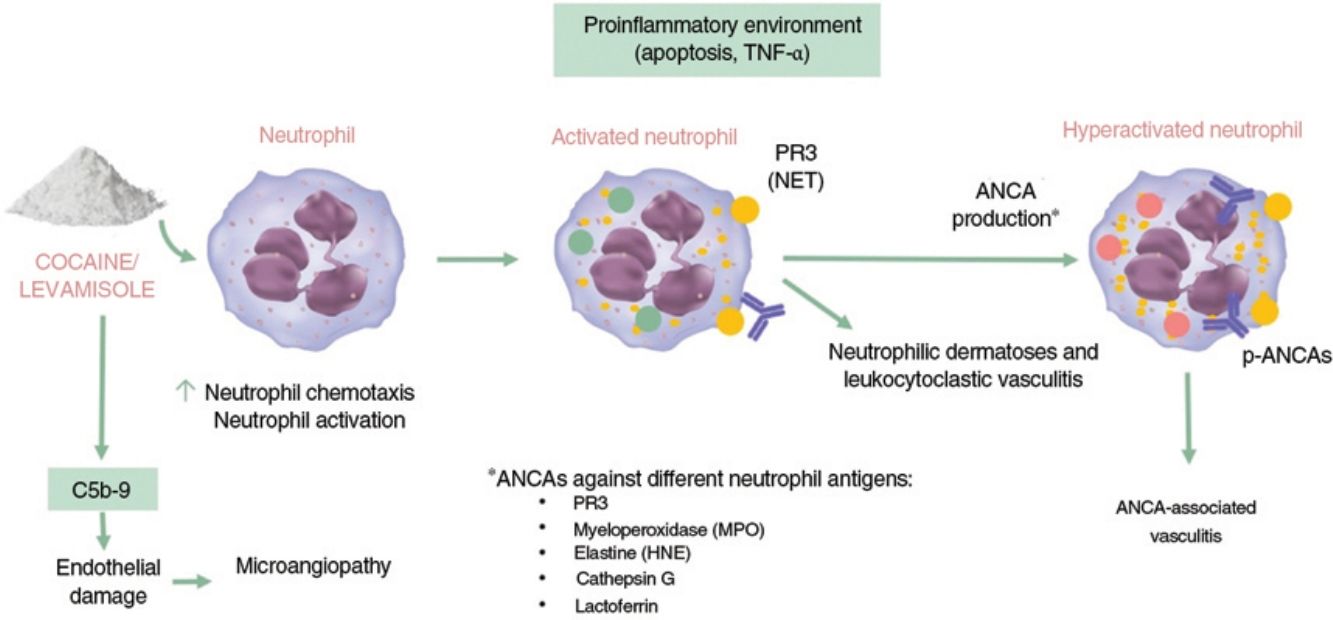
Autoimmunity and VasculitisIt has been well established that levamisole modulates immune function by enhancing the action of T cells and macrophages and increasing responses such as phagocytosis and neutrophil chemotaxis.3 Exposure to cocaine/levamisole can activate neutrophils, causing extracellular exposure of certain chromatin components (histones and double-stranded DNA) and granule proteins (myeloperoxidase and proteinase 3). The resulting structures are known as neutrophil extracellular traps (NETs). These NETs induce the formation of ANCAs targeting these proteins. The mechanism involved in the formation of these antibodies, however, is unknown, and it is also unclear why NETs are not formed following exposure to infection (Fig. 1).11,12
Immunogenic mechanisms of cocaine/levamisole. TNF indicates tumor necrosis factors; PR3, proteinase 3; NETs, neutrophil extracellular traps; ANCA, antineutrophil cytoplastic neutrophil; p-ANCAs, ANCAs with a perinuclear pattern; MPO, myeloperoxidase; HNE, human neutrophil elastase.
Commonly encountered ANCAs in cocaine/levamisole users are antimyeloperoxidase (MPO) antibodies with a perinuclear pattern (p-ANCAs) and, less frequently, antiproteinase 3 (PR3) antibodies with a cytoplasmic pattern (c-ANCAs). ANCAs concomitantly directed against other neutrophil antigens are also common and include human neutrophil elastase (HNE), lactoferrin, and cathepsin G. Other antibodies that may be observed are antiphospholipid, antinuclear, and anti-DNA antibodies.13
Patients with HLA-B27 have a greater susceptibility to neutropenia and agranulocytosis linked to levamisole consumption, although the mechanism involved is unclear.4,5
The resulting proinflammatory environment, combined with the presence of ANCAs, leads to vasculitis and endothelial damage; the alternative complement pathway also contributes to the formation of this environment. Cocaine metabolic products have been shown to enhance the synthesis and deposition of complement C5b-9, a mechanism directly involved in thrombotic microangiopathy.14
Clinical CharacteristicsCocaine/levamisole use is associated with multiple mucocutaneous manifestations. These are described below and summarized in Tables 1 and 2.
Mucocutaneous Manifestations of Cocaine Use.
| Nasal route | Inhaled route | Intravenous route |
|---|---|---|
| Intranasal viral wartsCrustsEpistaxisTurbinate asymmetry | Burns and viral warts on the hands (crack hands)Burns and abrasions on the lipsFacial burnsMadarosisPremature agingIncisor abrasions and fracturesPeriodontitis and caries | Track marksSkin poppingPuffy hand syndromeForeign body granulomasPhlebitis and thrombophlebitisSkin and subcutaneous tissue infections |
Systemic Symptoms Secondary to Cocaine Use.
| Ischemic, necrotic, and apoptotic conditions | Immune-mediated conditions | Neutrophilic conditions | Other |
|---|---|---|---|
| Systemic ischemia:- Raynaud phenomenon- Livedo reticularis- Distal ulcers- Necrosis- Digital gangreneLocal ischemia:- Nasal mucosal erythema- Anosmia- Chronic rhinitis- Epistaxis- Facial pain- Nasal and mouth ulcers- Destruction of underlying bone and cartilageInduction of apoptosis: cocaine-induced midline destructive lesions | ANCA-associated vasculitis/cocaine-levamisole-associated autoimmune syndrome | Pyoderma gangrenosumNeutrophilic dermatosis of the dorsal hands- Pyostomatitis vegetans-pyodermatitis vegetans | - Systemic scleroderma- Blistering diseases: pemphigus vulgaris and pemphigus vegetans- Drug-related eruptions: acute generalized exanthematous pustulosis, fixed drug eruption, and erythema multiforme/Stevens-Johnson syndrome- Other non-ANCA-associated vasculitides: Henoch-Schönlein purpura and urticaria vasculitis |
Abbreviation: ANCA, antineutrophil cystoplasmic antibody.
Mucocutaneous manifestations of cocaine use vary according to route of administration, which can be nasal, inhaled, or intravenous. They may be identical to those of other illicit drugs administered via the same routes.
Nasal RouteIntranasal cocaine use (snorting) has been linked to intranasal viral warts (snorters’ warts), intranasal and perinasal crusts, epistaxis, and nostril asymmetry.15,16
Inhaled RouteCocaine is inhaled via a glass or metal pipe, which when heated can cause hand burns and hyperpigmentation and favor the appearance of viral warts (crack hands). In addition, the smoke released is very hot and contains toxic, irritating substances, which can cause burns and abrasions on the lips and face, madarosis, and premature skin aging. Oral manifestations include thrush, mucositis (which can even manifest in the form of verrucous plaques), incisor abrasions and fractures due to contact with the pipe, periodontitis, and caries.15,16
Intravenous RouteIntravenous cocaine use is very uncommon. It can cause track marks in the form of superficial hyperpigmentation and scarring of the veins due to inflammation from repeated nonsterile injections. Other characteristic findings are skin popping, which are depressed scars and ulcers covered by hemorrhagic crusts; puffy hand syndrome, which consists of edema of the arms and hands due to venous and lymphatic insufficiency secondary to the toxic effects of the injected drug; foreign body granulomas, especially when adulterants such as talc are used; and phlebitis, thrombophlebitis, and skin and subcutaneous tissue infections.16
Ischemic and Necrotic ManifestationsSystemic IschemiaCocaine users can develop Raynaud phenomenon, livedo reticularis, distal ulcers, necrosis, and digital gangrene.16
Local IschemiaLocal ischemia in cocaine users can cause nasal mucosa erythema, anosmia, chronic rhinitis, epistaxis, tooth loss, facial pain, and nasal and oral ulcers. It can also affect underlying bone and cartilage structures and cause CIMDLs.17
Cocaine-Induced Midline Destructive LesionsCIMDLs involve centrifugal destruction of the oronasal mucosa and perichondrium and maxillary sinuses. Cocaine-induced vasoconstriction and massive apoptosis may even lead to orbital erosion.10,18 The true prevalence of CIMDLs is unknown, as many patients do not seek medical help, possibly because the anesthetic effect of the drug suppresses symptoms or because they wish to conceal their habit.18,19
Early manifestations of CIMDLs include intranasal crusting, foul-smelling exudate, epistaxis, nasal obstruction, headache, regurgitation, hypernasal speech, excessive sniffing, saddle nose deformities, nasocutaneous fistulae, and chronic sinusitis of the maxillary, ethmoidal, and sphenoidal sinuses. CIMDL is not usually accompanied by systemic manifestations, such as fever or raised inflammatory markers. It mostly involves the nasal septum but contiguous anatomic structures may sometimes be affected9,18,19 (Figs. 2 and 3).
Computed tomography scan of the patient in Fig. 2. Note the perforation of the nasal septum.
Blood tests may show positivity for anti-MPO antibodies, HNE, lactoferrin, and cathepsin G with a perinuclear pattern, and, less frequently, anti-PR3 antibodies with a cytoplasmic pattern.
Histologic findings include tissue necrosis, acute or chronic perivascular inflammatory infiltrates, microabscesses, leukocytoclastic vasculitis, and thrombosis of venules and arterioles, which may be partially or totally organized. Granulomatous inflammation has not been described.9
Immune-Mediated and Neutrophilic ConditionsANCA-Associated Vasculitis/Cocaine-Levamisole-Associated Autoimmune SyndromeSkin manifestations are the most common presentation of cocaine/levamisole-associated autoimmune syndrome (CLAAS). They usually appear within 24 to 96h of consumption in the form of retiform purpura, which can ulcerate and become necrotic. Lesions are bilateral and affect the lower limbs, trunk, ears, nose, cheeks, and fingers and toes. Extracutaneous symptoms are less common, and include arthralgia, fever, nephritis, hematologic alterations (mainly leukopenia, neutropenia, and agranulocytosis, but also thrombocytopenia and eosinophilia), and pulmonary, gastric, and neurologic manifestations. Histology shows leukocytoclastic vasculitis with fibrinoid necrosis of the vascular wall, extravasation of red blood cells, and intravascular fibrin thrombi in the dermis.20–22
Neutrophilic DermatosesMore than 20 cases of pyoderma gangrenosum (PG) associated with cocaine/levamisole use have been published. Lemieux23 et al. described several differences between cocaine/levamisole-induced PG and classic PG. The former is typically characterized by multiple, larger, lesions and has a predilection for the trunk, face, and ears, as opposed to the lower limb involvement seen in classic PG. Lesions appear within 1 to 4 weeks of consumption (Fig. 4). Similar histology and serology findings to those seen in other cocaine/levamisole-induced conditions may be observed. These include thrombotic vasculopathy and leukocytoclastic vasculitis and positivity for ANCAs and anticardiolipin and lupus anticoagulant antibodies. Why cocaine/levamisole induces neutrophilic dermatoses is unclear, but the mechanism is probably related to its chemotactic effect on neutrophils and ability to form NETs.
Two cases of pyostomatitis vegetans-pyodermatitis vegetans in the nasal and perinasal area have also been described in association with inhaled cocaine.24 There has also been a report of neutrophilic dermatosis of the dorsal hands.25
Other ConditionsTen cases of systemic scleroderma have been described in cocaine users. The etiology and pathogenesis are unknown, but it is believed that cocaine may act as a trigger. Patients have similar clinical manifestations, markers (ANA, anti-SCL70, anti-topoisomerase), and histology findings to those with primary systemic scleroderma, but more pronounced Raynaud phenomenon and digital ulcers. ANCAs may also be observed. Cocaine use should be suspected when investigating a case of systemic scleroderma in an unusually young man (<30 years) or a patient with positive ANCAs.26
There have also been isolated reports of pemphigus vulgaris,27 pemphigus vegetans,28 acute generalized exanthematous pustulosis,29 fixed drug eruption,30 erythema multiforme/Stevens-Johnson syndrome,31 Henoch-Schönlein purpura,32 and urticarial vasculitis.33
Differential DiagnosisThe differential diagnosis in systemic ischemic lesions is broad and should always include toxic causes. Because cocaine-induced distal ischemia usually occurs in young people and smokers, it can be confused with thromboangiitis obliterans or Buerger disease. Cocaine-induced ischemia also affects other tissues and may be associated with myocardial, cerebral, or digestive infarctions. On histology, intravascular thrombosis tends to more striking, while inflammatory infiltrates are milder and less common.34
The differential diagnosis of CIMDLs should include other causes of destructive midline lesions, such as vasculitis, sarcoidosis, mucocutaneous leishmaniasis, tuberculosis, tertiary syphilis, lepromatous leprosy, rhinoscleroma (Klebsiella rhinoscleromatis), invasive fungal infections (mucormycosis, paracoccidioidomycosis, and blastomycosis), and natural killer/T-cell lymphoma. Observation of ANCAs requires exclusion of granulomatosis with polyangiitis (GPA, formerly known as Wegener disease). Trimarchi9 et al. described clinical, laboratory, radiologic, and serologic differences between GPA and CIMDLs. Systemic symptoms such as fever, fatigue, arthritis, and elevated acute-phase reactants are much more frequent in GPA. Patients with CIMDLs will always show destruction of one or more contiguous structures, especially in the anterior part of the nose, which is most exposed to snorted cocaine. Anatomic destruction of the nasal septum has only been described in some cases of GPA. Massive apoptosis is the most characteristic histologic feature of CIMDLs, although other previously mentioned vascular changes may also be observed. Typical extravascular changes seen in GPA, such as granulomas, microabscesses, and deep necrosis, have not been described in CIMDLs. In serology, anti-PR3 c-ANCAs are typically seen in GPA. Lower-titer anti-MPO p-ANCAs are more common in CIMDLs and are nearly always accompanied by other ANCAs, such as anti-HNE, lactoferrin, and cathepsin G. HNE ANCAs are a highly sensitive and specific marker of cocaine/levamisole use. Antiphospholipid antibodies, ANAs, anti-double-stranded DNA, and decreased complement levels may also be observed.13 Less common findings include anti-MPO ANCAs with a cytoplasmic pattern and anti-PR3 ANCAs with a perinuclear pattern. These findings should raise suspicion as they are the inverse of typical patterns.
The differential diagnosis in CLAAS should include primary ANCA-associated small-vessel vasculitides. The distinction, however, can be challenging especially when differentiating between GPA and CLAAS presenting with ear, nose, and throat (ENT) manifestations, which are very common in cocaine users. Retiform purpura at typical CLAAS sites should raise suspicion of cocaine/levamisole use. As in CIMDL, systemic manifestations and inflammatory markers are not usually observed. Serology findings are very similar in CLAAS and CIMDLs, but in CLAAS, ANCA titers are usually higher than in primary ANCA-associated vasculitides. Extravascular changes such as granulomas are not an expected histology finding in CLAAS.20–22
Finally, the presence of multiple PG lesions in atypical locations such as the face, combined with positivity for ANCAs or other autoantibodies and histologic findings of thrombotic vasculopathy and leukocytoclastic vasculitis, should point to a possible case of cocaine-induced PG.23
DiagnosisDetermining whether a patient is a cocaine user or not is key to distinguishing between a primary condition and one caused by cocaine. Drug tests should be performed when cocaine use is suspected but denied by the patient, a common situation. The most common method to test for cocaine is a urine test, which can detect cocaine up to 2 or 3 days after use or up to 2 weeks in the case of regular users. Cocaine is detectable in blood and saliva for less than 48hours, but remains in sweat for several weeks. Detection in hair depends on the length of the follicles, but traces of cocaine can be observed several months after use.
Chromatography and mass spectrophotometry can detect levamisole in serum and urine, but levamisole has a short half-life (5–6hours), and these tests are not widely available. This explains why it has not been possible to determine whether the above conditions are caused by cocaine, levamisole, or both.15
Integration of clinical, histologic, and autoantibody findings can aid diagnosis, particularly when cocaine/levamisole use cannot be confirmed.
TreatmentTreatment should always be based on abstinence from cocaine use, appropriate support measures, and multidisciplinary management. Following cessation of use, PG lesions usually resolve within a week and CLAAS lesions within 2 to 3 weeks. Resumed consumption tends to result in the reappearance of, generally more severe, lesions. Antibodies usually become negative within 2 to 14 months.35
Topical antibiotics may be indicated for ear, nose, and throat lesions, given the high prevalence of colonization by S. aureus.
The use of corticosteroids and immunosuppressive agents in CLAAS is controversial. There is some evidence that corticosteroids are beneficial, and they may be contemplated when supportive measures are insufficient, when C-reactive protein levels are very high, or when an intense inflammatory component is observed on biopsy.3 For other conditions associated with or triggered by cocaine use, the treatment is the same as that indicated for the primary condition.
The definitive treatment for CIMDLs is surgical reconstruction, which usually requires between 6 and 18 months of abstinence.35
ConclusionsCocaine use is highly prevalent in Spain and adulteration with levamisole very common. Cocaine and levamisole are associated with diverse mucocutaneous and systemic conditions. As patients usually deny or underplay use, the differential diagnosis can be challenging.
Correct diagnosis is key to correct management, as immunosuppressive treatments are indicated for most primary conditions. Cessation and multidisciplinary management are essential for cocaine-induced conditions.
Conflict of InterestsThe authors declare they have no conflict of interest.