The patient, a 48-year-old woman from Marandúa, in Vichada, Colombia, was seen for an erythematous lesion that had developed on her right ear 3 months earlier. She denied any history of trauma or insect bite. On her own decision, she had taken oral fluconazole and had used topical corticosteroids and antibiotics, with no improvement.
Physical ExaminationOn physical examination, a shiny, infiltrated, edematous erythematous plaque with smooth borders and occasional pustules was observed on the helix and concha of the right ear (Fig. 1). The lesion was not tender and there were no palpable regional lymph nodes.
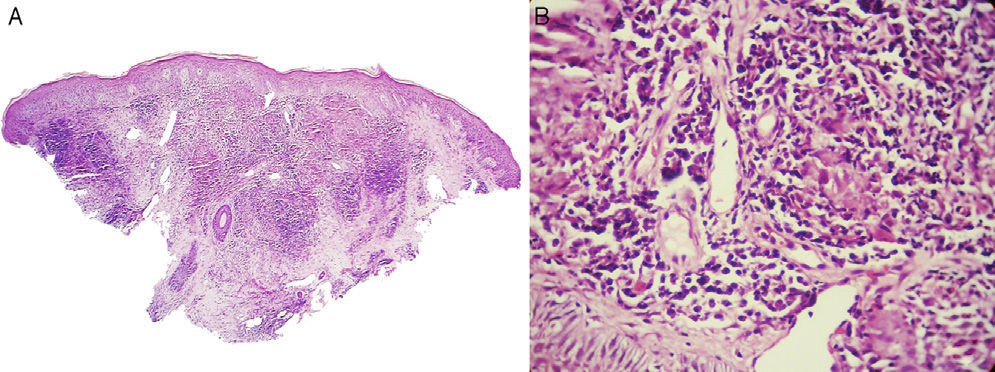
HistopathologySkin biopsy revealed epidermal hyperplasia with corneal pustules, a chronic diffuse dermal inflammatory infiltrate rich in plasma cells, epithelioid granulomas that contained numerous giant cells and some polymorphonuclear cells, and abscesses that extended from the dermis to the infundibula (Fig. 2, A andB).
Epidermal hyperplasia. Dermis showing chronic diffuse inflammatory infiltrate rich in plasma cells, with granulomas with numerous giant cells and occasional polymorphonuclear neutrophils. A, Hematoxylin and eosin (H&E), original magnification×2.5. B, H&E, original magnification×40.
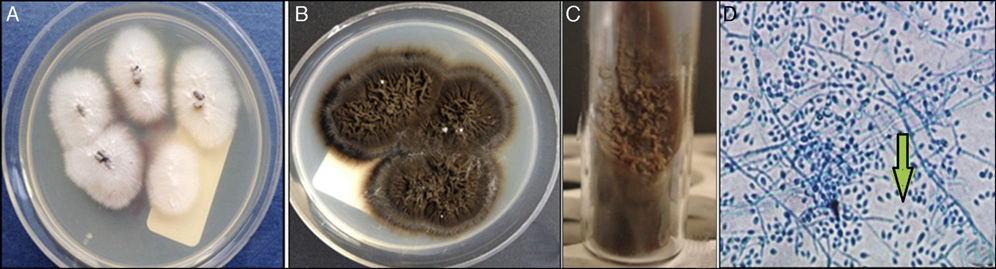
Direct microscopy and culture for Leishmania were negative. Culture on Sabouraud agar and potato dextrose agar to detect deep mycoses was positive for Sporothrix schenckii after 10 days of incubation at 25°C (Fig. 3, A andB). The yeast form was observed on Seneca agar (nutrient agar for the isolation of Leishmania spp.) after 15 days of incubation (Fig. 3C). The microscope image of the mycelial phase showed sympodial conidiation in a daisy-petal pattern (Fig. 3D).
What Is Your Diagnosis?
DiagnosisFixed cutaneous sporotrichosis.
Clinical Course and TreatmentThe patient was treated with oral itraconazole in pulses of 200mg every 12hours for 7 consecutive days per month for 6 months,1,2 leading to resolution of the condition.
CommentSporotrichosis is a deep mycosis with a subacute or chronic course. It is caused by the dimorphic fungus S schenckii. It typically affects farmers and is more common in men.3,4 The main route of inoculation is by trauma to skin soiled with contaminated material. Classic or lymphangitic sporotrichosis is the most common form of presentation. Other forms include fixed cutaneous and systemic sporotrichosis.2
Fixed cutaneous sporotrichosis usually affects exposed areas such as the face, neck and limbs; involvement of the ears is unusual. The disease presents as an infiltrated, verrucous, or ulcerated nodule or plaque with no lymph node enlargement; it can simulate other diseases such as cutaneous leishmaniasis, lupus vulgaris, scrofuloderma, lobomycosis, nocardiosis cutaneous, chromomycosis, cutaneous B-cell lymphoma, or sarcoidosis.2,3,5 According to the literature, its fixed form is due to a good immune response in patients who have had previous contact with the microorganism, limiting the infection to the site of inoculation.5,6 The frequency of the different presentations varies between geographical areas; the fixed form accounts for 10% to 30% of cases, compared with 85% for the classic lymphangitic form.2
Culture is the diagnostic method of choice. The colonies have a radial appearance and have a whitish color that usually becomes coffee colored at 25°C (Fig. 3, A andB). The definitive diagnosis is made on observing transition from the filamentous phase to the yeast form at 37°C (Fig. 3C). Microscopically, mycelia formation is observed with microconidia in a daisy-petal or peach flower arrangement,2,5 as was seen in our case (Fig. 3D).
Histopathology shows no specific pattern, but can suggest the diagnosis. Epidermal hyperplasia is present, with or without ulceration, and there is a chronic inflammatory reaction with the formation of suppurative granulomas containing neutrophilic microabscesses surrounded by epithelial cells and giant cells and an external region made up of lymphocytes, plasma cells, and fibroblasts. Asteroid bodies are only observed in 20% of cases and are not therefore pathognomic.2,5
We have presented a patient with fixed cutaneous sporotrichosis on the auricle of the right ear, an uncommon presentation at an unusual site. The clinical characteristics of this disease can mimic other diseases of noninfectious origin, such as sarcoidosis and cutaneous B-cell lymphoma, or of infectious origin, such as scrofuloderma, lobomycosis, nocardiosis, chromomycosis, or cutaneous leishmaniasis. In tropical countries such as Colombia, the main differential diagnosis is with cutaneous leishmaniasis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Arenas-Soto CM, Téllez-Kling AM, Alvarado-Álvarez ZL. Lesión infecciosa del pabellón auricular en el trópico. Actas Dermosifiliogr. 2016;107:599–600.