Lipoblastoma is a childhood tumor that usually appears in the first 3 years of life, although it may sometimes be present at birth. It occurs as a well-circumscribed lesion in the superficial subcutaneous tissue.1
Lipoblastoma accounts for between 5% and 30% of all soft-tissue tumors in children. The most common sites of occurrence are the upper and lower extremities, although the head, neck, and trunk may also be affected. On fewer occasions, there have been reports of retroperitoneal, mesenterial, mediastinal, and parotid lipoblastomas.1,2 The classic presentation is that of a smooth, painless, slow-growing mass that can sometimes displace neighboring structures or cause deformity of the anatomic region in which it is located.3
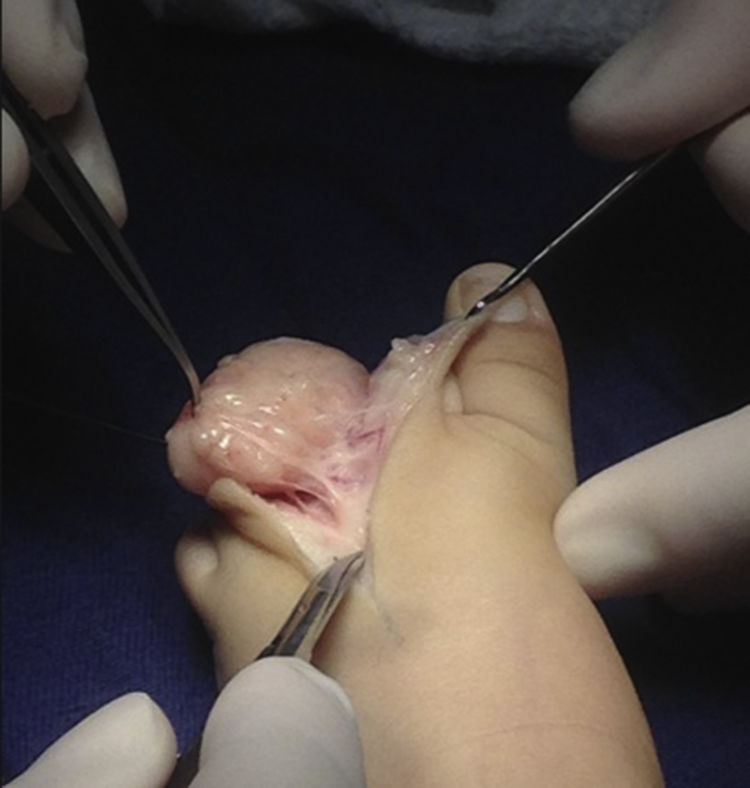
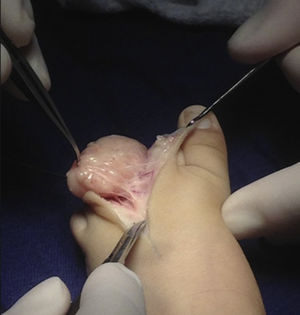
We report the case of a 5-month-old boy with a soft, recalcitrant mass on his middle left toe (Fig. 1). The mass had appeared in the first month of life and had exhibited fast, progressive growth. Soft-tissue ultrasound showed a solid, circumscribed lesion with a vascular appearance. Contrast magnetic resonance imaging (MRI) showed a well-defined solid mass with a vascular appearance consistent with a hemangioma or a low-flow vascular malformation.
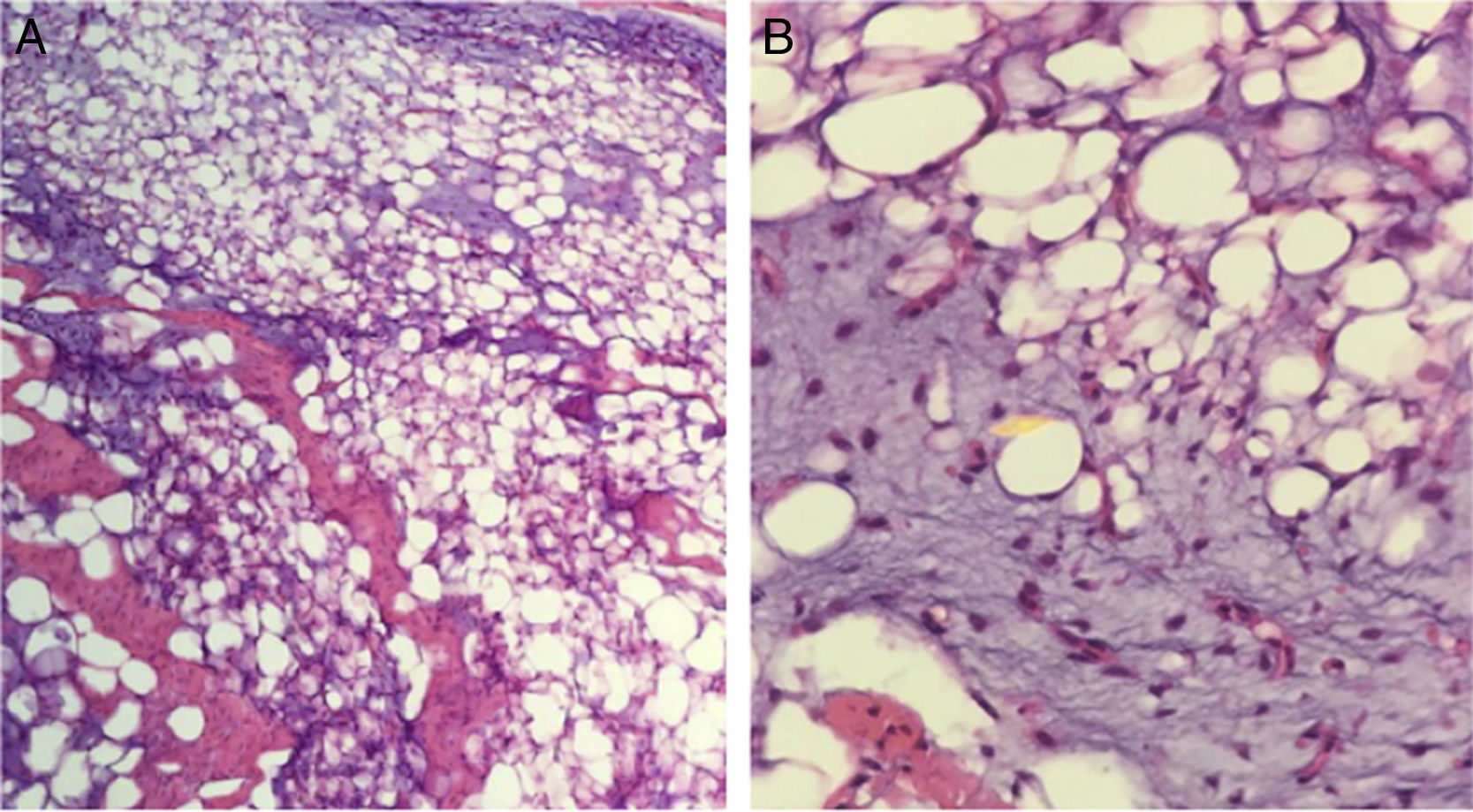
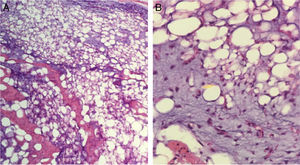
Because of its fast growth and deforming nature, the mass was removed by complete skin-sparing surgical excision with Z-plasty repair (Fig. 2). The pathology report described a well-defined, expansive mesenchymal lesion with multiple lobules of fat cells, some of which were immature, accompanied by an abundant myxoid matrix and a proliferation of nonatypical spindle cells with a soft appearance (Figs. 3A and B)
The patient progressed adequately and showed no signs of recurrence in the 6 months after the procedure.
Lipoblastomas are rare, benign mesenchymal tumors. They can be superficial (slow-growing well-circumscribed lesions) or diffuse (multicentric lesions arising in skeletal muscle or in the retroperitoneum or mesentery).3
Diagnosis should be based on the integration of clinical manifestations and diagnostic images, such as ultrasound, computed tomography (CT), and MRI. A definitive diagnosis, however, should be based on histopathological findings, and malignancy must be ruled out.
Histologically, lipoblastoma presents as a cellular tumor composed of immature fat cells (lipoblasts) with relatively well-defined septae and a fine vascular network. There is no pleomorphism or atypia.3 The most common form is myxoid lipoblastoma, which has abundant interstitial mucin in over 50% of the specimen. Genetic and pathological studies may be of use when microscopy does not provide a definitive diagnosis.3 Cytogenetic analyses and certain molecular tests are proving to be of diagnostic value. Evidence of genetic anomalies in lipoblastoma includes chromosomal rearrangements involving the 8q11.13 region and rearrangement of the pleomorphic adenoma gene 1 (PLAG1) in chromosome 8.3,4 These anomalies have not been observed in malignant tumors, such as liposarcoma. The differential diagnosis should include malignant soft-tissue tumors, such as liposarcoma, myxoid liposarcoma, rhabdomyosarcoma, and desmoid tumor, in addition to other benign tumors, such as lipoma, spindle-cell lipoma, and hibernoma. While clinically similar, some of these tumors present in adults. In addition, fat cells in both hibernoma and spindle-cell lipoma stain positively for protein S100.5,6 Lipoblastomas can also simulate vascular tumors, such as hemangiomas and angiolipomas.7 MDM2 and CDK4 are overexpressed in liposarcoma and positive immunohistochemical staining can therefore confirm malignancy and rule out other benign entities.8
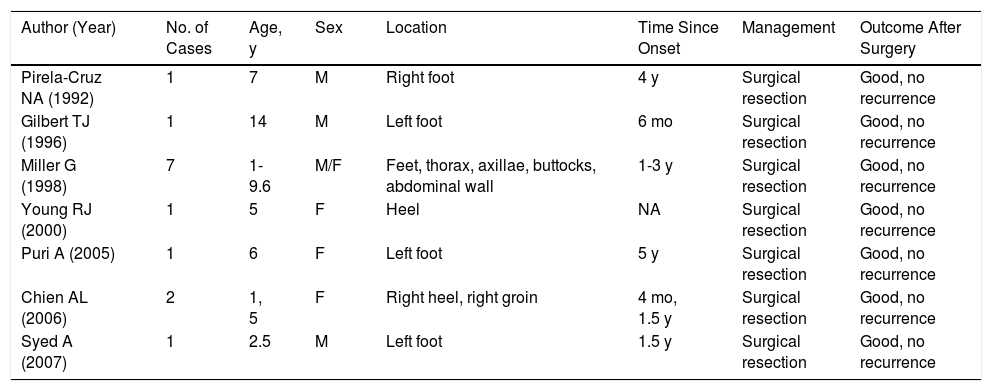
There have been few reports of childhood lipoblastoma involving the lower extremities and some of these are summarized in Table 1.9–15
Summary of Lipoblastoma Cases Reported in the Literature to Date.
| Author (Year) | No. of Cases | Age, y | Sex | Location | Time Since Onset | Management | Outcome After Surgery |
|---|---|---|---|---|---|---|---|
| Pirela-Cruz NA (1992) | 1 | 7 | M | Right foot | 4 y | Surgical resection | Good, no recurrence |
| Gilbert TJ (1996) | 1 | 14 | M | Left foot | 6 mo | Surgical resection | Good, no recurrence |
| Miller G (1998) | 7 | 1-9.6 | M/F | Feet, thorax, axillae, buttocks, abdominal wall | 1-3 y | Surgical resection | Good, no recurrence |
| Young RJ (2000) | 1 | 5 | F | Heel | NA | Surgical resection | Good, no recurrence |
| Puri A (2005) | 1 | 6 | F | Left foot | 5 y | Surgical resection | Good, no recurrence |
| Chien AL (2006) | 2 | 1, 5 | F | Right heel, right groin | 4 mo, 1.5 y | Surgical resection | Good, no recurrence |
| Syed A (2007) | 1 | 2.5 | M | Left foot | 1.5 y | Surgical resection | Good, no recurrence |
Abbreviations: F, female; M, male.
The treatment of choice is surgical excision. Recurrence following excision occurs in 9% to 33% of cases and tends to occur within 2 years of treatment.3–7
Lipoblastoma is a rare soft-tissue mesenchymal tumor that occurs almost exclusively in childhood. It is important to contemplate this entity in the differential diagnosis of fast-growing lesions that can simulate vascular lesions in imaging studies. This occurred in our case, where the histopathological examination had a key diagnostic role.
Conflicts Of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mordecay LG, Candia MPN, Fuentes CET, Zuluaga AMS. Lipoblastoma en la extremidad inferior de un lactante. Un caso representativo. Actas Dermosifiliogr. 2018;109:450–452.