A 14-year-old boy with no medical history of interest was seen for an asymptomatic lesion of stable size that had appeared 2 years earlier. The patient believed that the lesion may have been associated with trauma.
Physical ExaminationPhysical examination revealed a sclerotic-looking atrophic plaque of approximately 3cm in size with a central purple macule located in the right costolumbar area (Fig. 1).
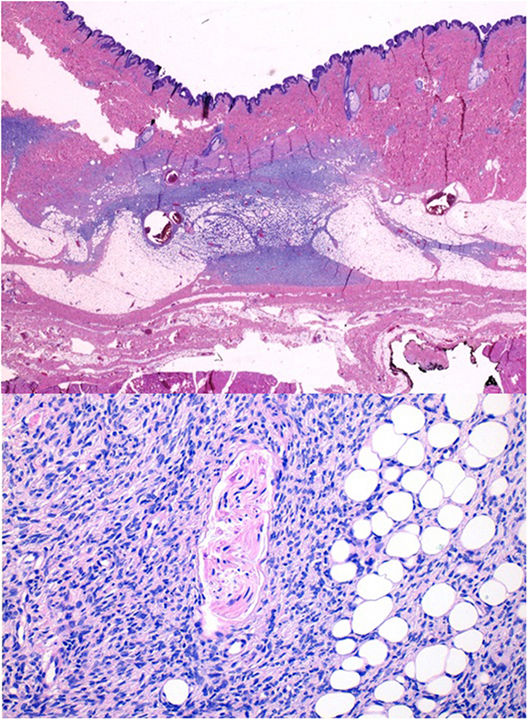
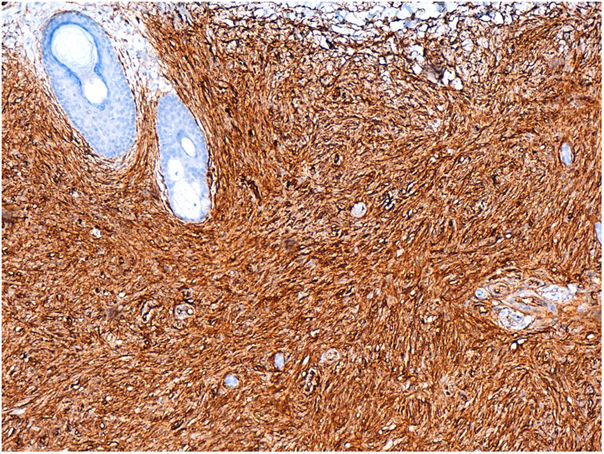
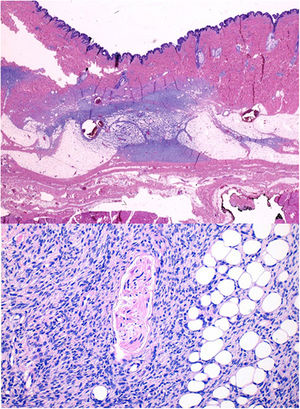
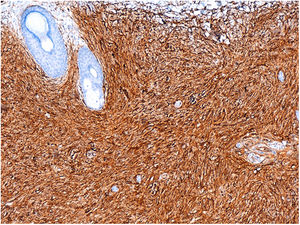
HistopathologyHistopathology showed a hypercellular tumor with poorly defined borders located in the reticular dermis and extending into the hypodermis. The cells were spindle-shaped and arranged horizontally to the epidermis, with a focal swirling pattern and honeycomb-like fat infiltration (Fig. 2). Immunohistochemistry revealed CD34 expression (Fig. 3).
Doppler ultrasound performed prior to biopsy showed a poorly defined, subcutaneous echogenic area (30mm×18mm) of absent flow.
Based on the histological diagnosis the patient underwent magnetic resonance imaging, which revealed a subcutaneous lesion that did not reach deep planes and no locoregional lymphadenopathy.
What Is Your Diagnosis?DiagnosisAtrophic dermatofibrosarcoma protuberans (DFSP).
Clinical Course and TreatmentThe tumor was excised with wide surgical margins, achieving tumor-free margins. The patient showed no signs of recurrence after 23 months of follow-up.
CommentDFSP is a cutaneous mesenchymal neoplasm of intermediate malignancy, characterized by a marked tendency to local recurrence and a low metastatic capacity.1 It accounts for 0.1% of all malignant skin tumors. It predominantly appears between the second and fifth decades of life, although it is thought that the proportion of pediatric cases is underestimated due to late diagnosis.1,2 Fortunately, in children this tumor appears to be less aggressive and to recur less frequently.1 It typically manifests as pinkish or brownish plaques on which exophytic nodules appear (as implied by the word protuberans), and is usually located on the trunk. In children, DFSP most commonly affects the lower extremities and acral areas, supporting an etiological role of trauma.1 Other clinical and pathological subtypes have been described, including an atrophic variant (which may also correspond to an early stage of a prolonged presentation).3 This subtype can be difficult to distinguish clinically from morphea, atrophoderma, atrophic scar (as in the present case), anetoderma, aplasia cutis, and lipoatrophy.1,4 Histology shows a dermal tumor that is thinner than the healthy dermis and retracts the skin, and consists of monomorphic spindle cells with mild atypia arranged in a storiform pattern.1,4 Immunohistochemistry is key to distinguishing this lesion from other tumors such as atrophic dermatofibroma, atypical fibroxanthoma, and undifferentiated pleomorphic sarcoma. DFSP is strongly positive for CD34 and negative for S100, EMA, desmin, and smooth muscle actin.4 Most DFSP patients carry a translocation in chromosomes 17 and 22, giving rise to the chimeric gene COL1A1-PDGFB, detection of which by fluorescence in situ hybridization (FISH) or reverse transcriptase polymerase chain reaction (RT-PCR) is highly specific for DFSP.1,5 The main treatment for DFSP is complete eradication of the tumor through excision with wide margins; Mohs surgery is considered the treatment of choice.1 Imatinib treatment can be considered in cases of unresectable tumors or in advanced stages of the disease.1 After surgery, follow-up every 6 to 12 months for at least 5 years is recommended.1 The prognosis for atrophic DFSP is the same as that for the classical form, but confusion of this tumor with benign atrophic lesions by both patients and doctors means that diagnosis and treatment, and subsequent cure, are often delayed.3,4 The present case underscores the importance of biopsy in cases of slow-growing atrophic plaques of uncertain diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank Dr. Juan Ayestaran of the Plastic Surgery Service and Dr. Alexandre Nogueira of the Pathological Anatomy Service of the Hospital Universitario de Cruces for their important contributions to the diagnosis and treatment of the patient.
Please cite this article as: Esteban Terradillos S, Allende Markixana I, Velasco Benito V. Placa atrófica en la espalda de un varón de 14 años. Actas Dermosifiliogr. 2020;111:413–414.