Recent years have seen important advances in our understanding of calciphylaxis, especially regarding newly identified risk factors and histologic findings that may aid diagnosis. This retrospective study of cases of calciphylaxis treated in our hospital in the last 13 years focuses on newly revealed aspects of this disease. We describe 16 patients (62.5% women; mean age, 67.9 years). In addition to advanced kidney disease (in 75% of our patients), other factors associated with the presence of calciphylaxis were a history of treatments related to phosphorus and calcium metabolism (75%) and anticoagulation (62.5%), usually with vitamin-K antagonists. Histology showed alterations in elastic fibers in only 25% of the biopsy specimens. Eleven of the patients died: sepsis was most often the cause.
En los últimos años se han producido importantes avances en el conocimiento de la calcifilaxis, al haberse identificado nuevos factores de riesgo para su desarrollo, y hallazgos histológicos que podrían ser de ayuda al diagnóstico. Nuestro propósito al realizar este estudio ha sido revisar retrospectivamente los casos de calcifilaxis atendidos en nuestro hospital en los últimos 13 años, con especial atención a los aspectos más novedosos de esta patología. Se incluyó un total de 16 pacientes, 62,5% mujeres, con edad media de 67,9 años. Entre los factores asociados destacaron, aparte de la enfermedad renal avanzada (75%), los tratamientos relacionados con el metabolismo fosfo-cálcico (75%) y la anticoagulación (62,5%), en su mayoría con fármacos antagonistas de la vitamina K. En el estudio histológico se hallaron alteraciones en las fibras elásticas solo en un 25% de las biopsias. Once de los pacientes han fallecido, siendo la sepsis la primera causa de muerte.
Calciphylaxis is an uncommon vascular disease characterized by ischemia and cutaneous necrosis resulting from calcification of the walls of small- and medium-caliber blood vessels. The condition was traditionally reported in patients with end-stage renal disease, although it can also affect patients with normal kidney function who have other risk factors1.
The etiology and pathogenesis of calciphylaxis are complex and have yet to be clarified. The interaction between various promoters and inhibitors of calcification has been implicated. Recent years have seen the involvement of extracellular matrix protein G1a, a potent inhibitor of vascular calcification whose action requires vitamin K–dependent carboxylation. Thus, the anticoagulant vitamin K antagonists could interfere with its action and thus boost the calcification process2–5. Furthermore, the presence of parathyroid hormone below recommended levels in 45% of cases of calciphylaxis suggests overuse of calcium and vitamin D supplements in affected patients, thus favoring adynamic bone disease and extraosseous calcification6.
The suspicion of calciphylaxis is based on clinical findings, namely, ulcerative-necrotic cutaneous lesions in a patient with risk factors1. Skin biopsy continues to be the gold standard for diagnosis, although its role is controversial owing to the associated risks7–9. Histopathology findings include calcium deposits on the medial layer of the vascular wall, hyperplasia/fibrosis of the arterial intimal layer, and thrombosis of dermal and hypodermal small vessels. More recently, some studies have reported alterations similar to pseudoxanthoma elasticum (PXE) and consisting of fragmentation and calcification of the elastic fibers, which take on a basophilic coloring. This finding is observed in up to 50% of biopsy specimens from patients with calciphylaxis and may prove useful for diagnosis in cases where vascular calciphylaxis is not easy to identify10–12. A potential explanation of these changes could be that calcium metabolism abnormalities may lead to calcification of the elastic fibers and their subsequent fragmentation, although, undoubtedly, there are other, as yet unknown factors that account for the lack of consistency in alterations that are similar to PXE in biopsy specimens from patients with calciphylaxis. Furthermore, caution is warranted, since these changes have also been reported in other diseases, such as stasis dermatitis, gangrene, various granulomatous diseases, and conditions affecting adipose tissue11.
We describe the epidemiological and clinical characteristics (with emphasis on risk factors such as anticoguation therapy), as well as the histopathological characteristics (including the study of changes in elastic fibers, recently described as an additional finding), of patients with calciphylaxis seen in the Dermatology Department of Hospital General Universitario de Alicante (HGUA), Alicante, Spain.
MethodsWe performed a retrospective study of patients with calciphylaxis seen in the Dermatology Department of HGUA between January 2006 and December 2019. Data were obtained from the clinical history and biopsy findings. In addition, all specimens were stained with orcein to highlight elastic fiber abnormalities. Calciphylaxis was diagnosed based on a histological examination of the skin specimens, through observation of calcification affecting the medial layer of dermal vessels within a compatible clinical context. The study was approved by the Clinical Research Ethics Committee of HGUA and complied with the ethical principles of the Declaration of Helsinki on medical experiments with human subjects.
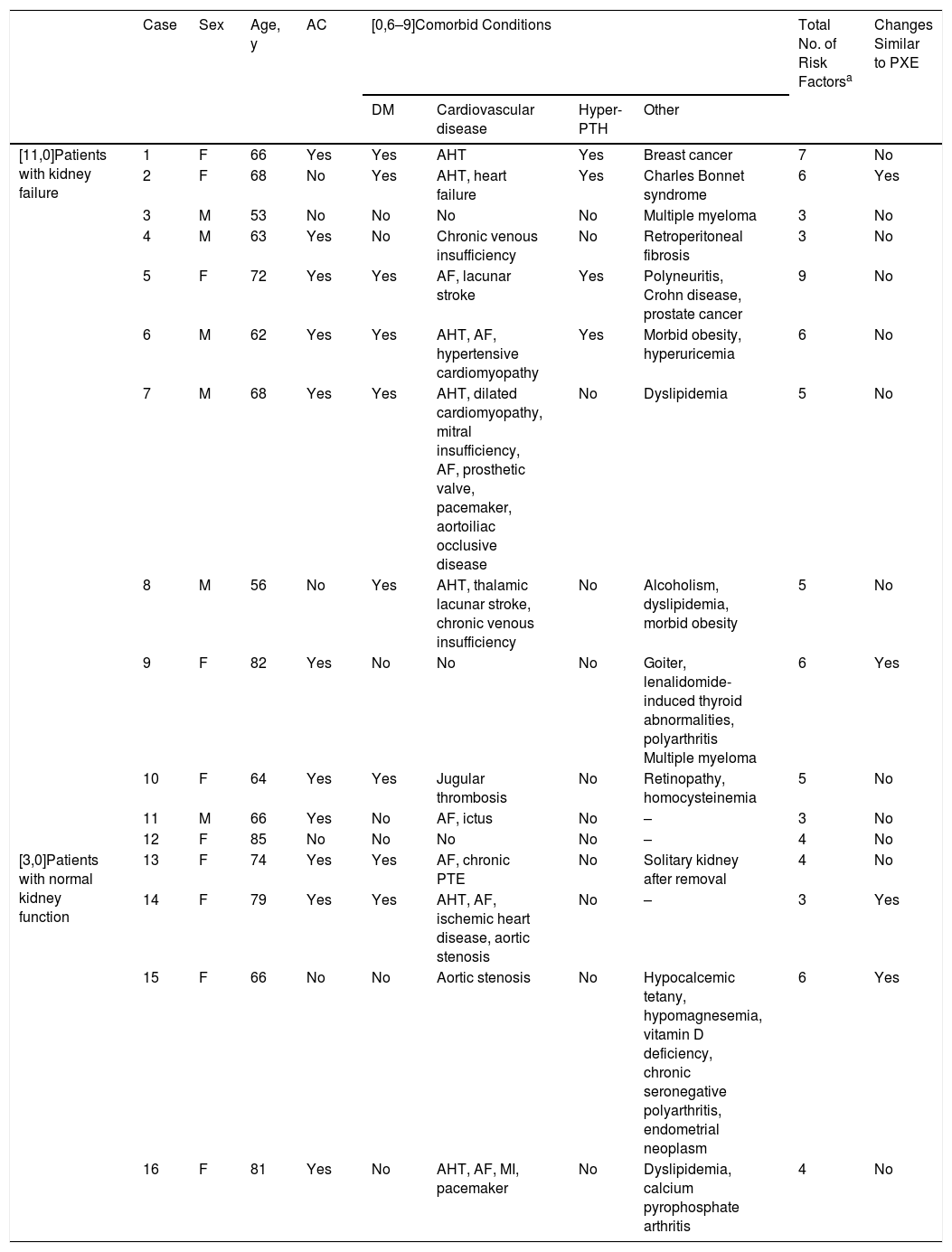
ResultsA total of 16 patients were diagnosed with calciphylaxis during the study period. Mean age was 67.9 years, and 62.5% were women (Table 1). All lesions were on the thighs or legs. Comorbid conditions are shown in Table 1. Of note, most patients had kidney failure (n = 12) and/or were receiving anticoagulation therapy (n = 10), mainly with vitamin K antagonists.
Patients With Calciphylaxis
| Case | Sex | Age, y | AC | [0,6–9]Comorbid Conditions | Total No. of Risk Factorsa | Changes Similar to PXE | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| DM | Cardiovascular disease | Hyper-PTH | Other | |||||||
| [11,0]Patients with kidney failure | 1 | F | 66 | Yes | Yes | AHT | Yes | Breast cancer | 7 | No |
| 2 | F | 68 | No | Yes | AHT, heart failure | Yes | Charles Bonnet syndrome | 6 | Yes | |
| 3 | M | 53 | No | No | No | No | Multiple myeloma | 3 | No | |
| 4 | M | 63 | Yes | No | Chronic venous insufficiency | No | Retroperitoneal fibrosis | 3 | No | |
| 5 | F | 72 | Yes | Yes | AF, lacunar stroke | Yes | Polyneuritis, Crohn disease, prostate cancer | 9 | No | |
| 6 | M | 62 | Yes | Yes | AHT, AF, hypertensive cardiomyopathy | Yes | Morbid obesity, hyperuricemia | 6 | No | |
| 7 | M | 68 | Yes | Yes | AHT, dilated cardiomyopathy, mitral insufficiency, AF, prosthetic valve, pacemaker, aortoiliac occlusive disease | No | Dyslipidemia | 5 | No | |
| 8 | M | 56 | No | Yes | AHT, thalamic lacunar stroke, chronic venous insufficiency | No | Alcoholism, dyslipidemia, morbid obesity | 5 | No | |
| 9 | F | 82 | Yes | No | No | No | Goiter, lenalidomide-induced thyroid abnormalities, polyarthritis Multiple myeloma | 6 | Yes | |
| 10 | F | 64 | Yes | Yes | Jugular thrombosis | No | Retinopathy, homocysteinemia | 5 | No | |
| 11 | M | 66 | Yes | No | AF, ictus | No | – | 3 | No | |
| 12 | F | 85 | No | No | No | No | – | 4 | No | |
| [3,0]Patients with normal kidney function | 13 | F | 74 | Yes | Yes | AF, chronic PTE | No | Solitary kidney after removal | 4 | No |
| 14 | F | 79 | Yes | Yes | AHT, AF, ischemic heart disease, aortic stenosis | No | – | 3 | Yes | |
| 15 | F | 66 | No | No | Aortic stenosis | No | Hypocalcemic tetany, hypomagnesemia, vitamin D deficiency, chronic seronegative polyarthritis, endometrial neoplasm | 6 | Yes | |
| 16 | F | 81 | Yes | No | AHT, AF, MI, pacemaker | No | Dyslipidemia, calcium pyrophosphate arthritis | 4 | No | |
Abbreviations: AC, anticoagulation; AF, atrial fibrillation; AHT, arterial hypertension; DM, diabetes mellitus; MI, myocardial infarction; PTE, pulmonary thromboembolism; PTH, parathyroid hormone; PXE, pseudoxanthoma elasticum.
Risk factors for calciphylaxis were as follows: kidney failure, abnormal serum levels of inorganic phosphorus and calcium, female sex, other comorbid conditions (e.g., obesity, diabetes mellitus, liver disease, autoimmune disease, metastatic cancer, malnutrition, hypoalbuminemia, rapid weight loss, hypotension, vitamin K deficiency), and treatment with calcium, vitamin D, vitamin K antagonists, iron, corticosteroids, albumin, or erythropoietin1.
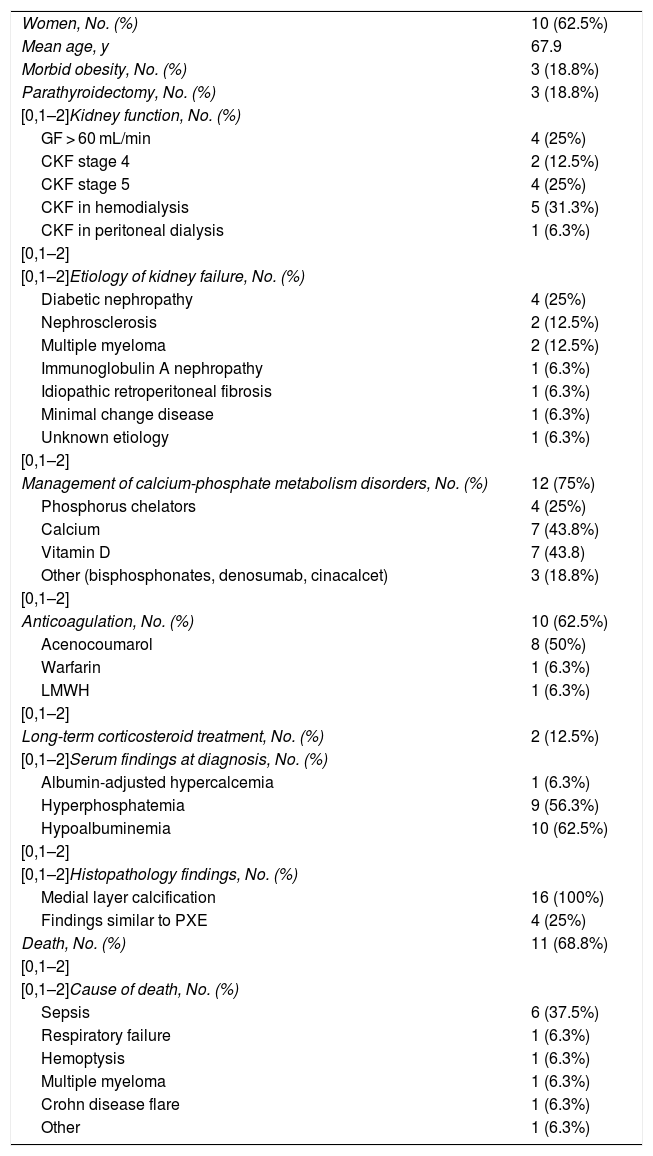
Mean age at diagnosis of kidney failure was 61 years, although in 3 cases, the diagnosis was made a few weeks before onset of the skin lesions of calciphylaxis. The causes of kidney disease, the most frequent of which was diabetic nephropathy, are summarized in Table 2. Of the 4 patients with normal kidney function, 3 had anticoagulation with acenocoumarol as a risk factor owing to the presence of atrial fibrillation, and 1 of these patients had only 1 kidney, although this had no effect on her glomerular filtration rate. One patient without kidney failure who was not receiving anticoagulation therapy had a comorbid condition, namely, a major disorder of phosphorus and calcium metabolism, and had to be admitted with symptomatic hypocalcemia, hypomagnesemia, and vitamin D deficiency, as well as endometrial carcinoma.
Epidemiological, Clinical, Laboratory, and Histopathologic Characteristics of Patients With Calciphylaxis
| Women, No. (%) | 10 (62.5%) |
| Mean age, y | 67.9 |
| Morbid obesity, No. (%) | 3 (18.8%) |
| Parathyroidectomy, No. (%) | 3 (18.8%) |
| [0,1–2]Kidney function, No. (%) | |
| GF > 60 mL/min | 4 (25%) |
| CKF stage 4 | 2 (12.5%) |
| CKF stage 5 | 4 (25%) |
| CKF in hemodialysis | 5 (31.3%) |
| CKF in peritoneal dialysis | 1 (6.3%) |
| [0,1–2] | |
| [0,1–2]Etiology of kidney failure, No. (%) | |
| Diabetic nephropathy | 4 (25%) |
| Nephrosclerosis | 2 (12.5%) |
| Multiple myeloma | 2 (12.5%) |
| Immunoglobulin A nephropathy | 1 (6.3%) |
| Idiopathic retroperitoneal fibrosis | 1 (6.3%) |
| Minimal change disease | 1 (6.3%) |
| Unknown etiology | 1 (6.3%) |
| [0,1–2] | |
| Management of calcium-phosphate metabolism disorders, No. (%) | 12 (75%) |
| Phosphorus chelators | 4 (25%) |
| Calcium | 7 (43.8%) |
| Vitamin D | 7 (43.8) |
| Other (bisphosphonates, denosumab, cinacalcet) | 3 (18.8%) |
| [0,1–2] | |
| Anticoagulation, No. (%) | 10 (62.5%) |
| Acenocoumarol | 8 (50%) |
| Warfarin | 1 (6.3%) |
| LMWH | 1 (6.3%) |
| [0,1–2] | |
| Long-term corticosteroid treatment, No. (%) | 2 (12.5%) |
| [0,1–2]Serum findings at diagnosis, No. (%) | |
| Albumin-adjusted hypercalcemia | 1 (6.3%) |
| Hyperphosphatemia | 9 (56.3%) |
| Hypoalbuminemia | 10 (62.5%) |
| [0,1–2] | |
| [0,1–2]Histopathology findings, No. (%) | |
| Medial layer calcification | 16 (100%) |
| Findings similar to PXE | 4 (25%) |
| Death, No. (%) | 11 (68.8%) |
| [0,1–2] | |
| [0,1–2]Cause of death, No. (%) | |
| Sepsis | 6 (37.5%) |
| Respiratory failure | 1 (6.3%) |
| Hemoptysis | 1 (6.3%) |
| Multiple myeloma | 1 (6.3%) |
| Crohn disease flare | 1 (6.3%) |
| Other | 1 (6.3%) |
Abbreviations: CKF, chronic kidney failure; GF, glomerular filtration; LMWH, low-molecular-weight heparin; PXE, pseudoxanthoma elasticum.
Hypercalcemia: albumin-adjusted serum calcium > 10.4 mg/dL.
Hyperphosphatemia: serum phosphate > 4.5 mg/dL.
Hypoalbuminemia: serum albumin < 3.5 g/dL.
CKF, stage 4: GF < 30 mL/min.
CKF, stage 5: GF < 15 mL/min.
Table 2 shows patients’ clinical characteristics, the treatment they had been receiving before developing calciphylaxis, and histopathology findings. Twelve patients (75%) were receiving treatment for calcium-phosphate metabolism disorders (most with calcium or vitamin D supplements). As for histopathology findings, all the patients had calcifications on the vessel wall, although elastic fiber abnormalities, specifically changes similar to PXE, were only identified in 4. Eleven patients (68.8%) died after the diagnosis of calciphylaxis within varying periods (1 month to 5 years); sepsis was the most common cause.
All patients received support therapy, and dialysis was intensified where necessary. Similarly, risk factors were corrected wherever possible (phosphorus and calcium abnormalities, suspension of vitamin K antagonists). In recent years, we have begun to use topical treatment with sodium thiosulfate 25% in Beeler base, although it was impossible to ensure long-term follow-up of those in whom it was used, since they died.
DiscussionThe clinical characteristics of the patients in this study are consistent with those reported in the literature we reviewed4,6,13–18, with a predominance of women in the seventh decade of life, lesions on the lower limbs, advanced kidney failure, and high mortality. Nevertheless, no patients in our series died of cardiovascular disease, which the literature revealed to be a major cause of death.
We found that 4 patients with calciphylaxis had normal kidney function and that a further 3 had been diagnosed with kidney failure a few weeks before the appearance of the skin lesions. Therefore, calciphylaxis diagnosed in patients with normal kidney function should be considered in the case of typical clinical lesions when there are other risk factors.
Another noteworthy finding is the fact that more than half of the patients in the present series were receiving anticoagulation therapy (62.5%), that is, higher than percentages reported elsewhere (25%-40%)2–5, with acenocoumarol being the most common drug. Warfarin is the most prescribed vitamin D antagonist in English-speaking countries, and, therefore, has been more commonly associated with onset of calciphylaxis. In Spain, on the other hand, acenocoumarol is the most prescribed vitamin K antagonist in the general population and in many patients with end-stage renal disease. Apixaban, an oral selective factor Xa inhibitor with no vitamin K antagonist effect and, therefore, no association with the development of calciphylaxis, was recently reported to be efficacious and safe in patients with kidney failure19. Consequently, this anticoagulant agent should be preferred in patients with renal disease and other risk factors for calciphylaxis. Furthermore, vitamin K supplements are being evaluated as prophylaxis in these patients20.
As for other drugs, 75% of patients in the present series were receiving treatment for calcium-phosphate metabolism disorders, mainly calcium and vitamin D supplements. In this sense, given the data reported here and our review of the literature, we would like to insist on the need for close monitoring of patients undergoing dialysis who are receiving supplements so as not to excessively suppress production of parathyroid hormone, since this could lead to extraosseous calcification6.
Analysis of biopsy specimens and staining with orcein to detect elastic fiber abnormalities only revealed changes similar to PXE in 4 patients, that is, 25% of biopsy specimens, which is lower than in other studies, where this finding was reported in more than half10,12. This histopathology finding, which seemed so promising for reaching a diagnosis of calciphylaxis in less expressive cases, is probably nonspecific and, as demonstrated elsewhere, can be seen in other granulomatous diseases or conditions affecting subcutaneous adipose tissue11.
Our study is limited by the fact that data were obtained retrospectively from clinical histories and may therefore be subject to bias. In addition, since the sample is small, all observations based on it must be confirmed with additional studies. However, it is necessary to remember that calciphylaxis is an uncommon condition and that the present series is the largest published in recent years in our setting.
In conclusion, calciphylaxis is uncommon, has a poor prognosis, and carries a high risk of short-term mortality. Our findings are consistent with those of other published series in terms of the risk factors reported, mainly kidney failure, although we also highlight the association with acenocoumarol. Therefore, caution is warranted when prescribing anticoagulation with vitamin K antagonists, as well as calcium and vitamin D supplementation, in patients with risk factors for calciphylaxis. As for the histopathology workup, we highlight that elastic fiber abnormalities did not prove to be sensitive for diagnosis of calciphylaxis in our series. Collection of data in broad registries, such as the European Calciphylaxis Network or the Partners Calciphylaxis Biobank, will improve our knowledge of this condition in the future.
FundingThe authors declare that no funding was received for the present study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Pujol MJ, Docampo Simón A, Illán Gambín F, Niveiro de Jaime M, Blanes Martínez M. Calcifilaxis: factores de riesgo y hallazgos histológicos en una serie de casos de un hospital terciario. Actas Dermosifiliogr. 2021. https://doi.org/10.1016/j.ad.2020.08.014