Hailey-Hailey disease (HHD), or benign familial pemphigus, is a rare autosomal dominant genodermatosis characterized by the formation of blisters. Eruptions are usually located in large skin folds, and when blisters become infected the condition can be very painful and disabling. HHD is difficult to treat. Many topical and systemic treatments have been used to bring exacerbations under control, but none have achieved medium- to long-term remission.
Patients and methodsRetrospective study of 8 patients with HHD treated with carbon dioxide laser therapy in our hospital between 1999 and 2011. The patients’ mean age was 50.7 years. The 4 men and 4 women were followed for between 1 and 12 years.
ResultsSatisfactory outcomes were achieved for 6 of the patients. Clinical improvement was observed in more than 75% of the affected area in 4 patients and in 50% to 75% of the area in 2 patients. The effect of treatments was maintained over time. The poorest outcomes were observed in patients treated at lower potencies. When blistering recurred after treatment, a second laser session achieved a good response. We observed no adverse events other than slight changes in skin texture and pigmentation.
ConclusionsCarbon dioxide laser therapy was safe and effective in producing medium- to long-term improvement in HHD symptoms that were refractory to conventional treatments.
La enfermedad de Hailey-Hailey (EHH) o pénfigo familiar benigno es un rara genodermatosis ampollosa con herencia autonómica dominante. Cursa erosiones cutáneas, localizadas principalmente en los grandes pliegues, que se sobreinfectan y pueden ser muy dolorosas e incapacitantes para los pacientes. Es una patología difícil de tratar y aunque se han usado múltiples tratamientos tópicos y sistémicos para controlar los brotes de la enfermedad, ninguno de ellos consigue remisiones a medio-largo plazo.
Pacientes y métodoRealizamos un estudio retrospectivo de una serie de 8 casos de EHH tratados con láser CO2 en nuestro centro desde 1999 a 2011. Los pacientes tratados tenían una media de edad de 50,7 años, siendo 4 de ellos hombres y 4 mujeres. El seguimiento de los pacientes osciló entre 1 y 12 años.
ResultadosDe los 8 pacientes tratados, 6 obtuvieron unos resultados satisfactorios (4 pacientes con mejoría clínica > 75% y 2 pacientes entre 50-75%). Esta eficacia se mantuvo a lo largo del tiempo. Los peores resultados se observaron en los pacientes tratados con potencias más bajas. Las zonas con recidiva de la enfermedad después del tratamiento, se trataron con una segunda sesión de láser con buena respuesta. No observamos efectos adversos, salvo ligeros cambios texturales y de la pigmentación.
ConclusionesEl láser de CO2 es un tratamiento eficaz y seguro a medio-largo plazo en los casos de EHH sintomáticos y refractarios a tratamientos convencionales.
Hailey-Hailey disease (HHD), or familial benign pemphigus, is a rare autosomal dominant blistering skin disorder caused by a mutation in the gene encoding a Ca2+-dependent ATPase located within the Golgi apparatus.1 Patients develop blisters and erosions, which predominantly affect the large skinfolds, and in particular axillary and inguinal folds. It is a chronic condition, characterized by recurrent flares generally triggered by factors such as friction, sweating, heat, stress, local infection, and UV radiation.2
HHD is difficult to treat. The literature contains many accounts of different topical and systemic treatments being used to control disease flares. Treatments include antibiotics and antivirals to treat secondary bacterial and viral infections; botulinum toxin to minimize aggravating factors, such as excessive sweating,3–5 and immunomodulators, such as corticosteroids,6 ciclosporin,7–9 and tacrolimus10–12 to reduce the associated inflammatory response. Photodynamic therapy has also been tested, but with little success.13,14 The above treatments, however, only result in temporary improvements in symptoms; they do not alter the course of disease, and they only rarely lead to long-term remission.
Surgical treatment of HHD should be considered in patients who do not respond to general measures or to conventional oral or topical treatments. Several cases published in recent years have shown carbon dioxide (CO2) laser skin resurfacing to be effective in HHD. We present a series of 8 cases of HHD treated with this technique and conclude that it is a safe and effective treatment option in this setting.
Material and MethodsWe performed a retrospective study of patients with HHD treated with CO2 laser resurfacing at Clínica Universitaria de Navarra in Spain between 1999 and 2011.
Diagnosis of HHD was based on clinical and histological criteria (coalescing blistering lesions, typically located in the skinfolds, that rupture to form erosions; histology showing intraepidermal blisters associated with acantholytic cells; a negative direct immunofluorescence test; and the absence of other diseases that could explain the manifestations of HHD).
The patients were all aged over 18 years, had disabling symptoms that interfered with activities of daily living, and had not responded to conventional topical or systemic treatment (topical and oral corticosteroids and antibiotics). They had no concomitant conditions.
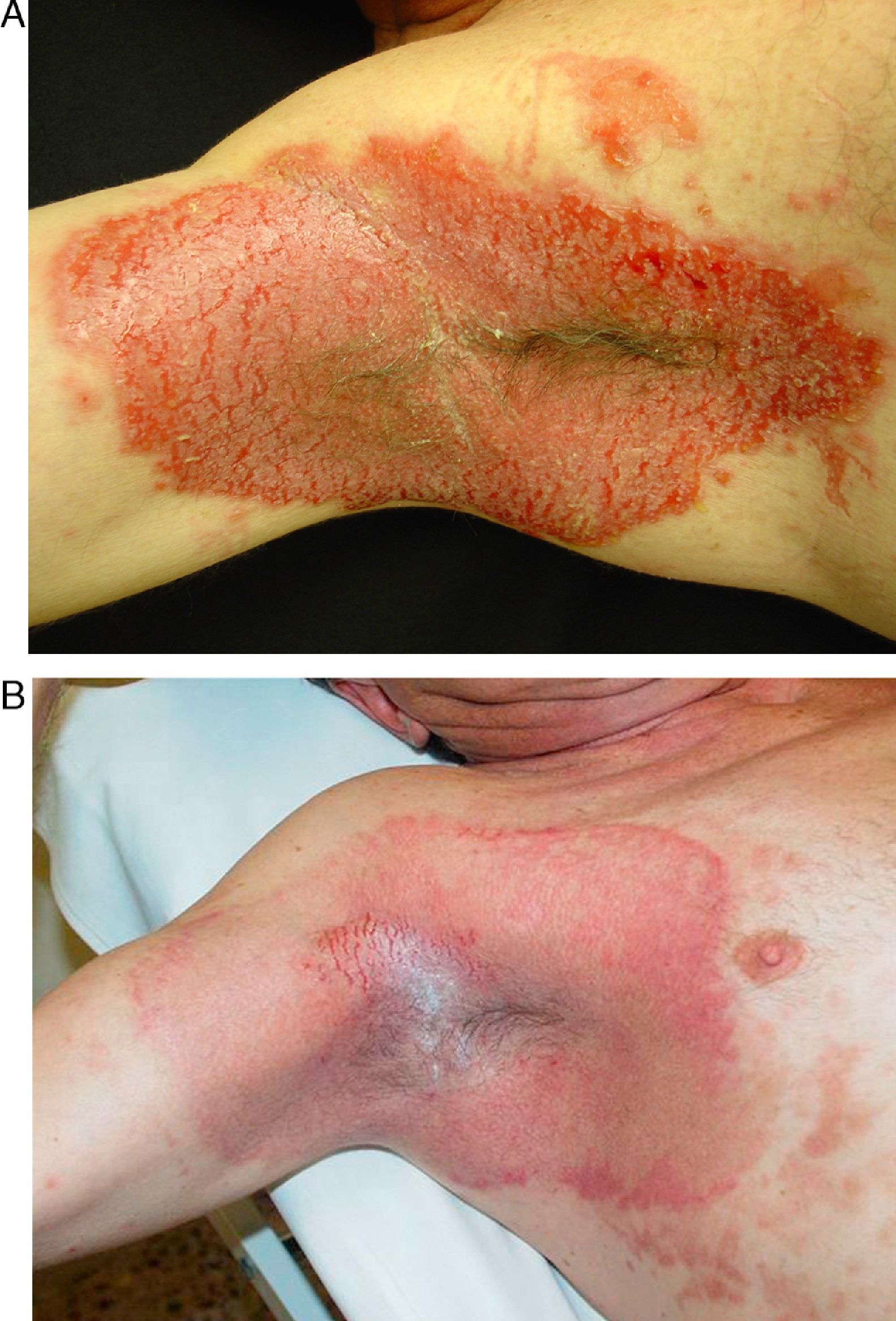
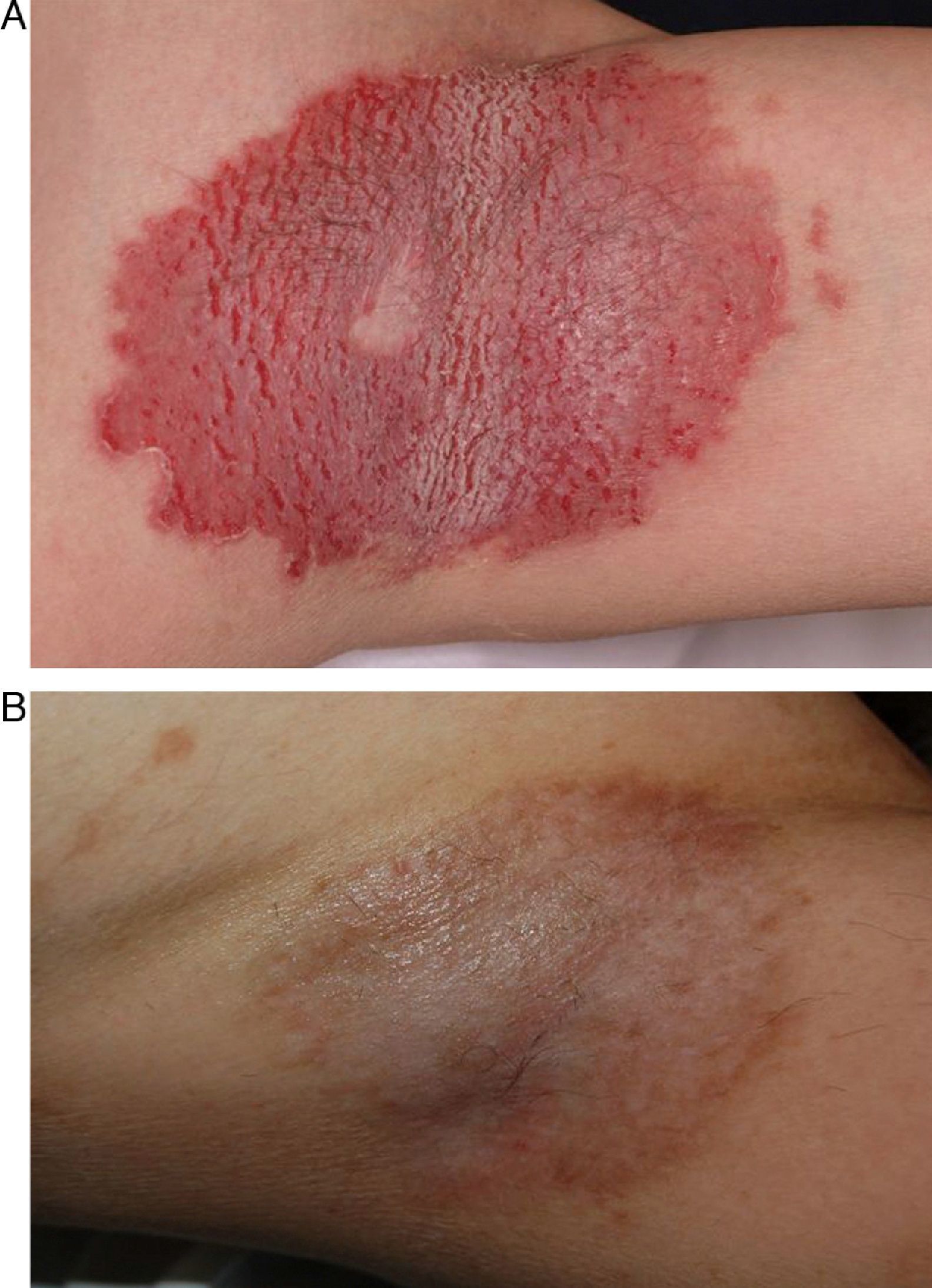
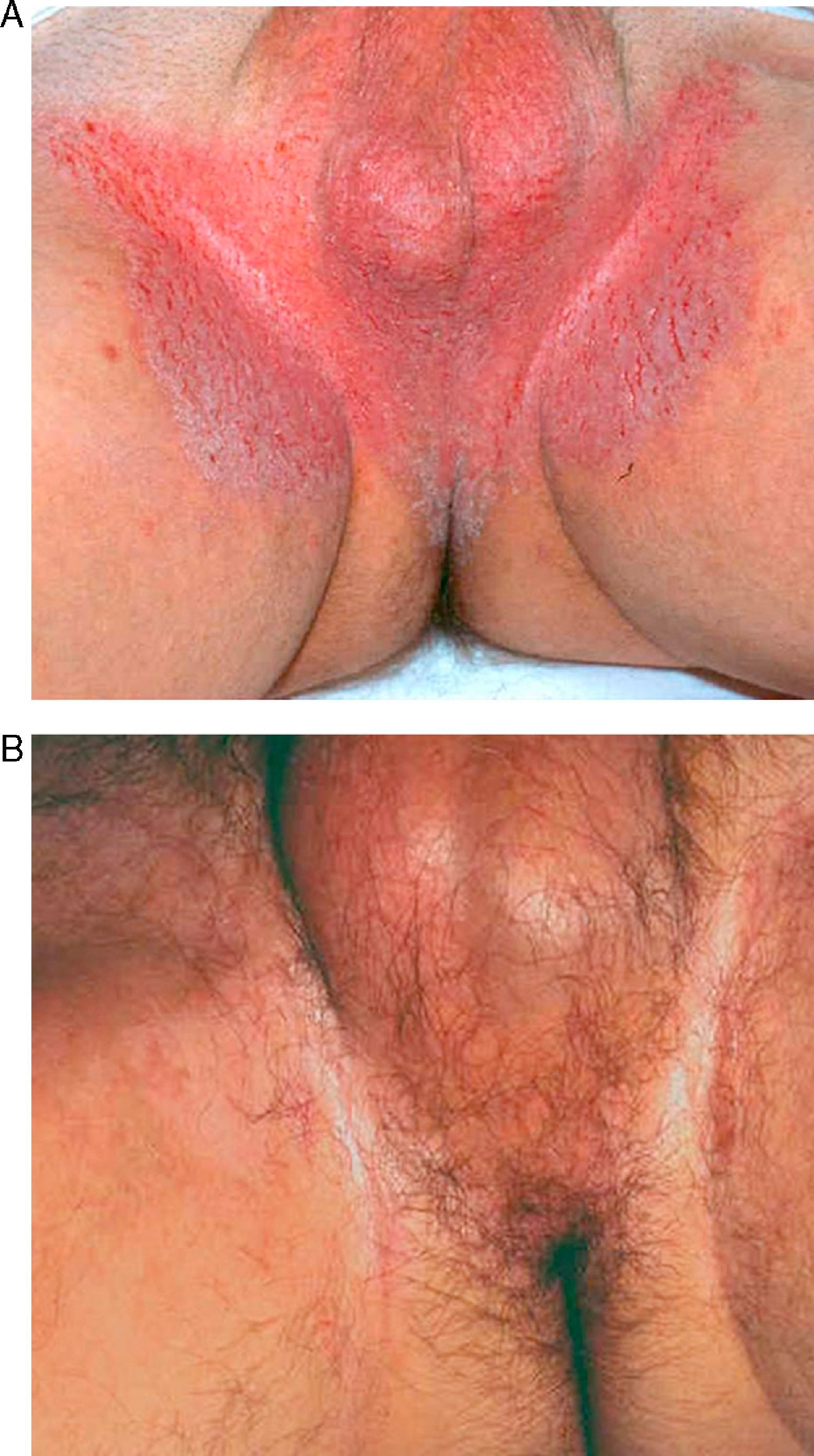
We studied 8 patients (4 men and 4 women), with a mean age of 50.7 years (range, 27-69 years). Mean age at the time of diagnosis was 35.5 years. Half of the patients had a family history of HHD. Lesions affected the groin in 100% of cases, the axillae in 87%, the genital area in 75%, the perianal area in 50%, and the trunk and arms in 25% each. Several areas were affected in a considerable number of cases (Table 1). All the patients signed an informed consent form before undergoing laser treatment. They were examined by an anesthesiologist, who confirmed their suitability for general or spinal anesthesia. The areas to be treated, generally the axillae (Figs. 1 and 2) and genitocrural area (Fig. 3), were marked before the procedure. In 1 patient with a particularly severe form of HHD, treatment also targeted the thorax, arms, legs, neck, and back (Fig. 4). This patient asked for treatment to be targeted at more visible areas, namely the back, the abdomen, and the elbow and knee pits, even though she had been informed that the procedure would probably result in textural changes to the skin and hypopigmentation and/or hyperpigmentation (Fig. 4).
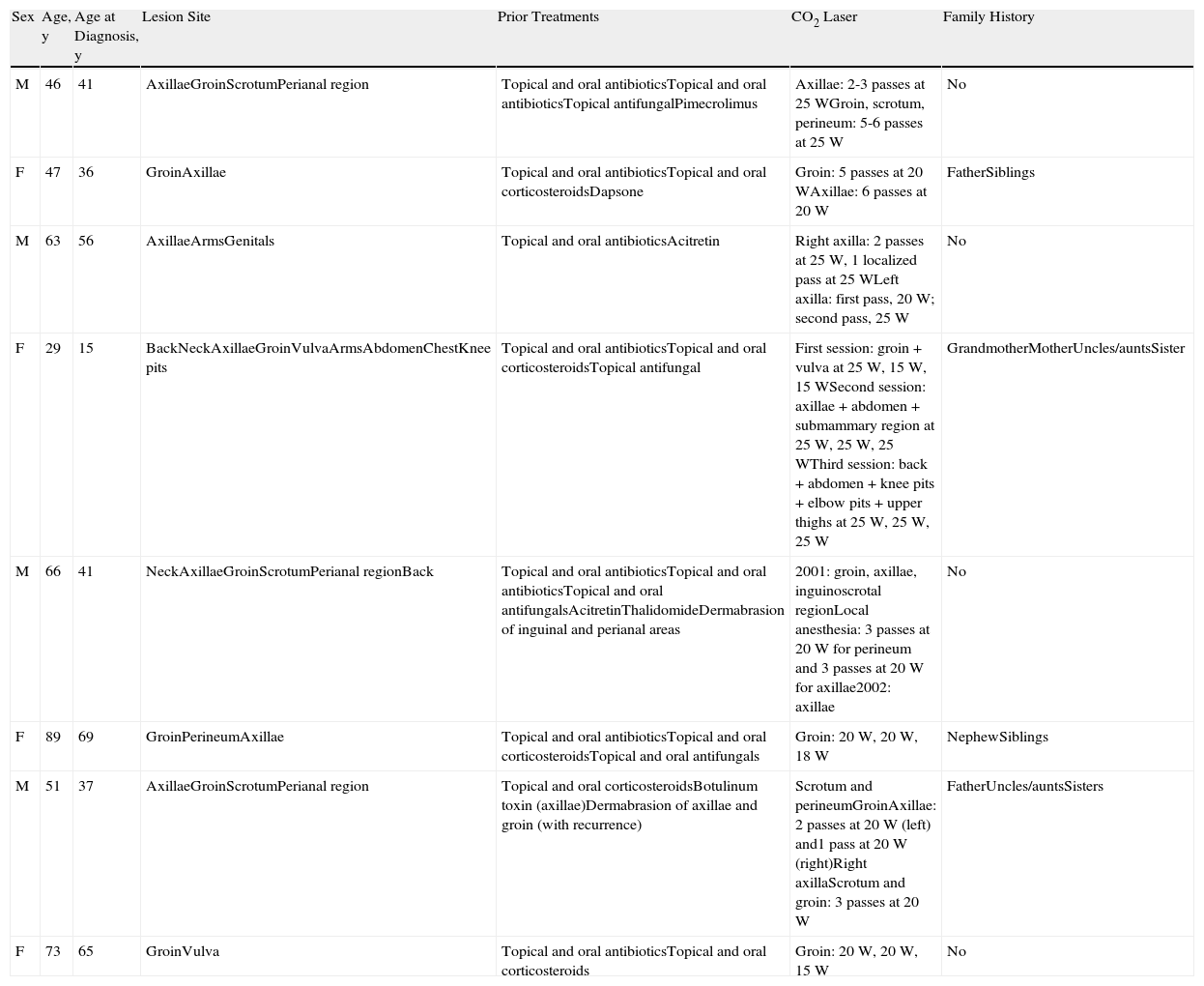
Results of Treatment With Carbon Dioxide (CO2) Laser in Hailey-Hailey Disease.
| Sex | Age, y | Age at Diagnosis, y | Lesion Site | Prior Treatments | CO2 Laser | Family History |
| M | 46 | 41 | AxillaeGroinScrotumPerianal region | Topical and oral antibioticsTopical and oral antibioticsTopical antifungalPimecrolimus | Axillae: 2-3 passes at 25WGroin, scrotum, perineum: 5-6 passes at 25W | No |
| F | 47 | 36 | GroinAxillae | Topical and oral antibioticsTopical and oral corticosteroidsDapsone | Groin: 5 passes at 20WAxillae: 6 passes at 20W | FatherSiblings |
| M | 63 | 56 | AxillaeArmsGenitals | Topical and oral antibioticsAcitretin | Right axilla: 2 passes at 25W, 1 localized pass at 25WLeft axilla: first pass, 20W; second pass, 25W | No |
| F | 29 | 15 | BackNeckAxillaeGroinVulvaArmsAbdomenChestKnee pits | Topical and oral antibioticsTopical and oral corticosteroidsTopical antifungal | First session: groin + vulva at 25W, 15W, 15WSecond session: axillae + abdomen + submammary region at 25W, 25W, 25WThird session: back + abdomen + knee pits + elbow pits + upper thighs at 25W, 25W, 25W | GrandmotherMotherUncles/auntsSister |
| M | 66 | 41 | NeckAxillaeGroinScrotumPerianal regionBack | Topical and oral antibioticsTopical and oral antibioticsTopical and oral antifungalsAcitretinThalidomideDermabrasion of inguinal and perianal areas | 2001: groin, axillae, inguinoscrotal regionLocal anesthesia: 3 passes at 20W for perineum and 3 passes at 20W for axillae2002: axillae | No |
| F | 89 | 69 | GroinPerineumAxillae | Topical and oral antibioticsTopical and oral corticosteroidsTopical and oral antifungals | Groin: 20W, 20W, 18W | NephewSiblings |
| M | 51 | 37 | AxillaeGroinScrotumPerianal region | Topical and oral corticosteroidsBotulinum toxin (axillae)Dermabrasion of axillae and groin (with recurrence) | Scrotum and perineumGroinAxillae: 2 passes at 20W (left) and1 pass at 20W (right)Right axillaScrotum and groin: 3 passes at 20W | FatherUncles/auntsSisters |
| F | 73 | 65 | GroinVulva | Topical and oral antibioticsTopical and oral corticosteroids | Groin: 20W, 20W, 15W | No |
| Recurrence | Pain | Recovery | Adverse Effects | Improvement, % | Follow-up | Patient Satisfaction |
| No | Severe | 8 wk | No | >75% | 3 y | High |
| No | Severe | 20 wk | Hyperpigmentation | 50%-75% | 6 y | Moderate |
| Local (axillary area) | Severe | 4 wk | Hyperpigmentation | 50%-75% | 6 y | Moderate |
| No | Severe | 6 wk | Hyperpigmentation | |||
| Small hypertrophic scar | ||||||
| Textural changes | >75% | 1 y | High | |||
| Local (axillary area) | Moderate | 3 wk | No | 25%-50% | 5 y | Low |
| No | Mild | 3 wk | No | >75% | 10 y | High |
| Local (axillary, | ||||||
| scrotal, inguinal areas) | Moderate | 2 wk | Hypopigmentation | >75% | 12 y | High |
| No | Severe | 6 wk | Hypopigmentation | <25% | 2 y | Low |
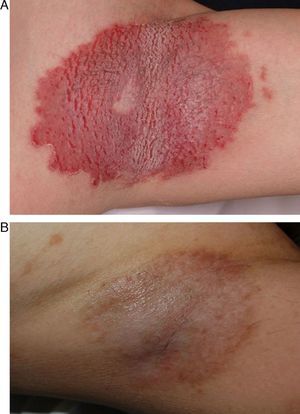
A, 56-year-old patient with severe Hailey-Hailey disease affecting both axillae. B, Photograph taken 1 month after treatment with carbon dioxide laser skin resurfacing. Note the considerable improvement in lesions and the small area of local recurrence in the armpit. The patient decided not to undergo partial treatment of this small area in a second laser session.
A 29-year-old patient with Hailey-Hailey disease. A, Lesions in the axillary area. B, Lesions in the submammary region. C, Lesions on the posterior aspect of the trunk. D, E, F. Appearance of lesions 9 months after treatment with carbon dioxide laser skin resurfacing. Note the considerable improvement in the lesions and the areas of residual hypopigmentation and hyperpigmentation. Despite these skin changes, the patient decided to undergo further treatment of lesions in other areas.
The procedure was performed under general or spinal anesthesia, depending on the location of the lesions. Local anesthesia was used in patients with lesions confined to small areas. All areas were disinfected with povidone iodine before treatment.
A continuous-wave CO2 laser with computerized scanning (Sharplan SilkTouch laser; Sharplan Lasers, Inc.) was used in all cases. The procedure was performed with a 200-mm handpiece, an output power of 20 to 25W, a pulse duration of 450ms, and a spot diameter of 9mm. The laser was connected to a plume removal system. Two to 3 passes were used in most cases; after each pass, all traces of abraded skin were removed using saline-moistened gauze. At the end of each session, the skin had a yellowish appearance with red pinpoint dots. Topical gentamicin was applied to the treated area, which was covered with Linitul or Mepitel dressings covered with gauze.
All the patients received prophylactic antibiotic treatment and analgesics (metamizole or morphine derivatives) after the procedure. Topical gentamicin and dressings were applied daily for a week, during which time the patients remained in hospital.
ResultsConsiderable improvement was observed in almost all patients (Table 1). In 1 patient, new lesions developed at the edge of the treated area several days after the procedure. Local recurrence was observed in 3 patients (38%) 6 months after treatment (Fig. 1). The lesions were successfully treated in a second CO2 laser session involving more passes than in the first session. The poorest outcomes were observed in patients who had been treated at the beginning of the study period, possibly because the lower output powers used initially were insufficient.
Postoperative pain was moderate to intense in most patients, with analgesics being required in some cases. Complete reepithelialization was observed within 7 to 10 days in the majority of cases. The average time missed from work was 7 weeks.
None of the patients developed postoperative contact dermatitis or bacterial, viral, or fungal infections. Three patients developed postinflammatory hyperpigmentation, which improved with time. Permanent mild hypopigmentation was observed in 1 patient and a small hypertrophic scar in the elbow pit in another. The scar responded very well to corticosteroid injections. Treatment satisfaction—assessed by questionnaire after several years of follow-up—was high in almost all cases. Six of the 8 patients rated the treatment outcome as satisfactory; 4 of these had a clinical improvement of more than 75%, while 2 had a clinical improvement of between 50% and 75%; Table 1). The patients were followed for between 1 and 12 years.
DiscussionHHD is a rare hereditary blistering skin disease. It runs a chronic course, with periods of remission punctuated by flares triggered by friction, sweating, heat, stress, local infection, UV radiation, or skin conditions such as contact dermatitis.2
Patients with HDD have severely impaired quality of life. The lesions are painful and cause continuous discomfort as they are located in areas prone to friction from clothes. Furthermore, they frequently become infected, causing an unpleasant smell that can be highly distressing for patients.
Treatment outcomes in HDD are not very satisfactory, and in many cases, the lesions are aggravated by friction and bacterial, viral, or fungal infections. Avoidance of trauma and the treatment of secondary infections with antiseptic products and topical or systemic antibiotics can help to improve lesions. Long-term remission, however, is rare.
Satisfactory results have been reported patients treated with botulinum toxin,3–5 which reduces excessive sweating, an aggravating factor in HHD. Treatment with topical and oral corticosteroids or with immunomodulators, such as ciclosporin7–9 and tacrolimus,10–12 may reduce the inflammatory response associated with the disease. Effective results have been reported for other drugs, such as dapsone, methotrexate,15 and retinoids,16,17 but the evidence is limited to isolated, anecdotal cases. However, none of these treatments alter the course of the disease; they provide only temporary relief from symptoms.
Surgical treatment is indicated in cases of HHD that are refractory to general measures and conventional oral or topical treatment. The surgical removal of lesions followed by skin grafting has produced successful outcomes in some patients,18,19 but the cosmetic and functional sequelae of surgery have led to the search for more superficial ablative techniques that would be equally effective but less aggressive.
Several reports of the use of dermabrasion to treat HHD have been published.20,21 Dermabrasion may be an effective treatment for lesions confined to small areas and it does not cause the highly visible scars associated with conventional surgery and skin grafts; it is also associated with a lower risk of scar retraction. Another advantage is that a skin donor site is not required. However, since the depth of skin removal in dermabrasion is highly dependent on the surgeon, there is an increased risk of secondary scarring. Furthermore, hemostasis is not attained and there is a greater risk of infection due to the dispersion of abraded tissue.
Laser therapy offers significant advantages over dermabrasion. On the one hand, it allows more precise control of treatment depth, thereby minimizing the risk of inadvertent penetration of the reticular dermis and scarring. On the other hand, treatment depth is predictable during each pass of the laser, making the technique more reproducible and less operator-dependent than dermabrasion and other techniques.
Two types of lasers are used for ablative skin resurfacing: the erbium:yttrium-aluminum-garnet (Er:YAG) laser and the CO2 laser. Both are used for cosmetic and therapeutic purposes (e.g., photorejuvenation and removal of skin hamartomas).
The Er:YAG laser emits light with a wavelength of 2940nm and permits precise ablation of tissue with minimal thermal damage to adjacent skin. The depth of penetration is more superficial than that achieved with the CO2 laser and hemostasis is not attained. Only 1 study to date has shown Er:YAG laser treatment to be effective in HHD.22
The CO2 laser emits light with a wavelength of 10600nm, which is largely absorbed by water in the tissues.23 It is used for skin rejuvenation and offers precise control of ablation depth and thermal damage.
It offers several advantages over other lasers and techniques, including hemostasis in the treated area, greater reproducibility of results, and less operator dependency. Furthermore, when used with a plume removal system, it is cleaner—and associated with less biological risk—than dermabrasion.
In recent years, several reports of cases of HHD treated with CO2 lasers have been published.24–30 In most of the cases, the treatment was very effective and associated with few adverse effects.
We used the Sharplan Silk Touch laser with computerized scanning in our series. To minimize lateral thermal damage and consequently the risk of scarring and pigmentary changes in such cases, the pulse duration should be shorter than the thermal relaxation time of the target tissue (approximately 200-600ms for skin).31 The depth of ablation using this approach is 80 to 100 μm with 2 passes and 150 μm with 3 passes.31 We used 3 passes.
Based on our experience, we believe that an aggressive approach, consisting of 3 passes with a laser output power of at least 25W, is necessary for CO2 laser resurfacing to be effective in HHD. Such an approach is sufficient to reach the deep papillary dermis and to cause fibrous bands of scar tissue in the treated area. A certain degree of thermal damage is also believed to be necessary to achieve good results and prevent recurrence. Insufficient thermal damage could explain why recurrence is sometimes observed in cases treated with lower output powers or short pulse durations. In our series, recurrence was more common in such cases. Specifically, new lesions appeared in patients who were treated with fewer than 3 passes and with an output power of less than 25W. Recurrence is also common at the edges of treated areas. These lesions improve with time, and if they persist, they can be treated in a second laser session if the patient so wishes. Adverse effects associated with CO2 laser resurfacing can be of a short or long duration. Short-term complications include erythema, pruritus, acneiform eruptions, infections, and allergic or irritant contact dermatitis.32 All the patients in our series developed intense erythema that lasted for several months. No postoperative infections were observed, but it should be noted that all the patients received prophylactic antibiotics after the procedure.
Postoperative wound care is easier with CO2 laser therapy than with other techniques, such as dermabrasion, because it is associated with less bleeding, exudation, and crusting. In our series, open dressings were used to protect the wounds until complete reepithelialization.
Closed methods (semi-occlusive dressings) have been reported to result in less postoperative pain and faster reepithelialization. They are, however, more expensive and also associated with a higher rate of infection.33 In our patients, the treated areas healed in approximately 10 days.
The main limitation of CO2 laser resurfacing in HHD is that it is a painful procedure. While topical anestetics can relieve a certain amount of pain, they are generally insufficient in larger areas or in areas in which more than 2 passes are used; in such cases, general or locoregional anesthesia is indicated. Postoperative pain tends to last for 10 to 14 days. In our series, most of the patients rated the pain as moderate or severe.
The long-term adverse effects caused by CO2 laser therapy include erythema, hypopigmentation, hyperpigmentation, and permanent scarring.34 The incidence of postoperative hyperpigmentation varies according to skin type, with figures ranging between 26% and 36%; this adverse effect is more common in patients with dark skin.32 Hyperpigmentation tends to be transient and generally resolves with time. Hypopigmentation has been reported in between 8% and 19% of patients and is related to ablation depth.32 Because an aggressive approach is necessary to achieve good results, patients will almost certainly experience pigmentary or textural changes. Hyperpigmentation was observed in practically all the patients in our series; hypopigmentation was also seen, but in fewer cases. Skin changes due to CO2 laser resurfacing improve with time. However, as HHD affects areas that are normally covered, these changes are generally well tolerated by the patient.
While certain textural changes were observed in our patients, only 1 patient developed a scar. This was located in an elbow pit and responded well to corticosteroid injections. No scars were observed in areas that are more prone to scarring, such as the back and the thorax.
Some authors have indicated that deep ablation, extending as far as the hair follicle, is necessary to prevent recurrence in Darier disease and HHD35; we agree with their opinion that these depths are necessary to achieve favorable outcomes.
A small number of cases have reported the successful use of CO2 lasers in HHD and other acantholytic disorders.24–30
In all cases reported to date, the lesions treated covered less extensive areas than in our series. Furthermore, all the reports in the literature have described the treatment of lesions in the axillary, genitocrural, and submammary areas. In our series, 1 of the patients had extensive lesions that also affected the back, the neckline, the arms, and the abdomen. Treatment outcomes were good and the adverse effects were acceptable.
The underlying mechanism through which laser therapy causes lesions to improve or disappear is not yet fully understood. It is known that ablation of the epidermis and dermis leads to reepithelialization based on cells from skin appendages. Under normal conditions, reepithelialization after deep erosion of the epidermis occurs through the expansion of keratinocytes derived from follicular stem cells.36 The question that remains unanswered is why the new epidermis in patients with HHD is not defective, given that this disease is based on germinal mutations,37 present in every cell. It would be logical to assume that follicular and interfollicular stem cells would carry the same mutation. One hypothesis is that the mutation exists in both types of cells but is not expressed in follicular cells. Several types of epidermal cell clones (mutated and unmutated) may exist, and unmutated cells would possibly have a greater chance of surviving when there is dermal and epidermal damage followed by wound healing.38 If this were the case, unmutated clones would replace the defective clones in treated areas. We think that it would be interesting to explore this hypothesis in future studies.
Some authors have reported that successfully treated lesions are replaced by atrophic scars.37 The area of fibrous tissue might harden the skin in this area, making it more resistant and consequently less prone to external mechanical damage. Another theory is that the destruction of eccrine glands could, at least in part, explain the success of CO2 laser therapy, as it would reduce triggers such as sweating.38 Nevertheless, biopsies of treated areas have shown the persistence of eccrine glands.38
Taken together, the above hypotheses suggest that treatment with CO2 laser may affect the threshold expression of the HHD mutation by inducing physical changes in the treated skin.
CO2 laser skin resurfacing in HHD is a reproducible, operator-independent technique. It provides a bloodless surgical field and offers acceptable cosmetic results and long-term effectiveness, with few adverse effects. Given that HHD is an incurable condition, we believe that CO2 laser skin surfacing is a good alternative for cases that do not respond to conventional treatments. Patients should be informed that the energy required for effective treatment may cause textural and pigmentary skin changes. In general, this may not be a problem because the lesions are frequently located in unexposed areas, but the possible consequences should be considered in other, more visible, areas.
The main limitations of this study are its retrospective design and the fact that we did not compare CO2 laser therapy with other treatment modalities.
We believe that our findings are of interest as our series is the largest reported to date of HHD treated with CO2 laser resurfacing. Furthermore, we have provided the first-ever report of this modality being used to treat extensive lesions involving areas beyond the intertriginous areas.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of patient data and that all the patients included in this study have been appropriately informed and gave written informed consent to participate in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This documentation is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pretel-Irazabal M, et al. Tratamiento de la enfermedad de Hailey-Hailey con láser de dióxido de carbono: tratamiento en 8 pacientes. Actas Dermosifiliogr. 2013;104:325–33.