Chemical peeling is a common treatment in cosmetic dermatology. A peel that has been used for many years is trichloroacetic acid. Its adverse effects have for a long time been a major limitation. We present a practical review of the characteristics, mechanisms of action, indications, and complications of superficial chemical peels and of peeling with trichloroacetic acid.
Las exfoliaciones químicas (más conocidas como peelings químicos) son tratamientos utilizados frecuentemente en dermatología estética. En concreto el peeling con ácido tricloroacético se ha utilizado desde hace años y una de sus principales limitaciones clásicamente era sus efectos secundarios. Presentamos una revisión práctica de las características, mecanismos de acción, indicaciones y complicaciones de los peelings en general, tanto los superficiales como el peeling con ácido tricloroacético.
Chemical peeling consists of the application of a chemical substance to the skin in order to produce desquamation of the stratum corneum and normalization of the epidermis with remodeling of the skin, leading to improvement in a number of skin alterations. They are one of the most commonly used cosmetic procedures, as they can produce a considerable improvement in quality of the treated skin after a short and, in some cases, very mild recovery period.
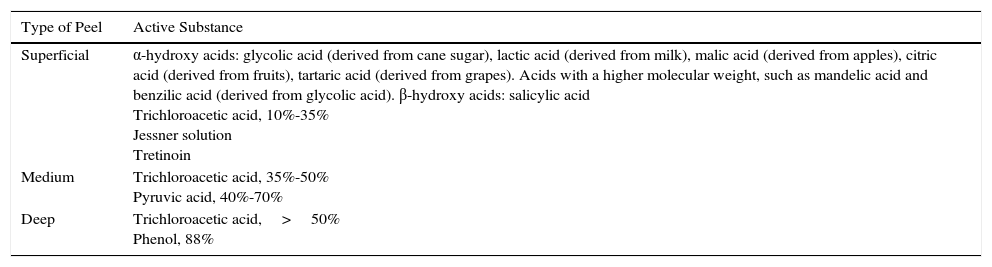
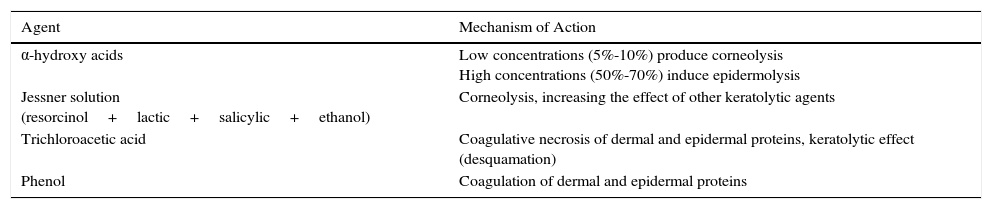
Chemical peels are traditionally classified as superficial, medium, or deep according to their depth of action (Table 1). In addition, the mechanisms of action can vary depending on the active substance or substances contained in the peel (Table 2).
Classification of the Types of Peel According to The Depth of Action.
| Type of Peel | Active Substance |
|---|---|
| Superficial | α-hydroxy acids: glycolic acid (derived from cane sugar), lactic acid (derived from milk), malic acid (derived from apples), citric acid (derived from fruits), tartaric acid (derived from grapes). Acids with a higher molecular weight, such as mandelic acid and benzilic acid (derived from glycolic acid). β-hydroxy acids: salicylic acid Trichloroacetic acid, 10%-35% Jessner solution Tretinoin |
| Medium | Trichloroacetic acid, 35%-50% Pyruvic acid, 40%-70% |
| Deep | Trichloroacetic acid,>50% Phenol, 88% |
Mechanism of Action of the Distinct Peeling Agents.
| Agent | Mechanism of Action |
|---|---|
| α-hydroxy acids | Low concentrations (5%-10%) produce corneolysis High concentrations (50%-70%) induce epidermolysis |
| Jessner solution (resorcinol+lactic+salicylic+ethanol) | Corneolysis, increasing the effect of other keratolytic agents |
| Trichloroacetic acid | Coagulative necrosis of dermal and epidermal proteins, keratolytic effect (desquamation) |
| Phenol | Coagulation of dermal and epidermal proteins |
Superficial peels act on the epidermis, without penetrating the basement membrane. They stimulate keratinocyte renewal from the basal layers of the epidermis and produce a reactive inflammation in the upper dermis that stimulates neocollagenesis by activating fibroblasts that synthesize new collagen (types I and IV) and elastic fibers. They can act on the dermis by direct induction of type i collagen synthesis by fibroblasts or by indirect mechanisms, through the action of keratinocyte-derived factors that secondarily stimulate collagen production by dermal fibroblasts. Glycolic acid peels have been reported to induce the release of interleukin-1α in the epidermis, with particularly high levels in the area of the basement membrane.1,2 The term very superficial is used to refer to those peels that only produce mild desquamation of the corneal layer; these are often called home peels.3
Medium peels affect the whole of the epidermis and the papillary dermis, and can penetrate to the upper reticular dermis. In this case, skin regeneration occurs from the cells of the follicular epithelium, which generate new layers of epidermis and stimulate the synthesis of collagen and elastic fibers.2
Finally, deep peels eliminate the epidermis and penetrate to the mid reticular dermis. The majority of these peels produce protein coagulation, observed clinically as frosting. In these cases, epidermal regeneration also develops from the cells of the follicular epithelium and there is intense synthesis of collagen and elastin that can persist for years after performing the peel.2
The main indications for treatment with chemical peels include the following: melasma, ephelides, postinflammatory hyperpigmentation, photoaging, under-eye circles, acne vulgaris, rosacea, and scars.
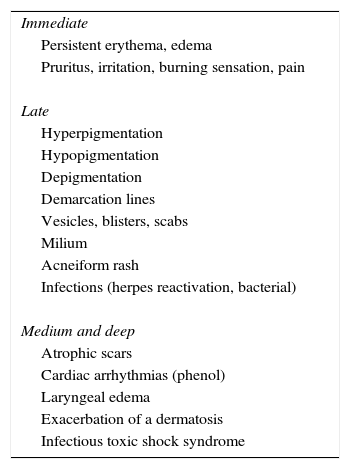
Although complications (Table 3) are rare when peeling is performed using the correct technique for the active substance, a number of factors must be taken into consideration to minimize the risk.
General Postpeeling Complications.
| Immediate |
| Persistent erythema, edema |
| Pruritus, irritation, burning sensation, pain |
| Late |
| Hyperpigmentation |
| Hypopigmentation |
| Depigmentation |
| Demarcation lines |
| Vesicles, blisters, scabs |
| Milium |
| Acneiform rash |
| Infections (herpes reactivation, bacterial) |
| Medium and deep |
| Atrophic scars |
| Cardiac arrhythmias (phenol) |
| Laryngeal edema |
| Exacerbation of a dermatosis |
| Infectious toxic shock syndrome |
Source: Nikalji et al.4
The medical history and dermatologic examination will help to ensure correct patient selection. Skin preparation is an important step that contributes to achieving a more homogeneous effect and thus a more predictable result.
The type of acid employed, the vehicle, concentration, number of layers, and contact time are some of the factors that determine the depth of action of the peel and possible complications. In the case of glycolic acid, the pH and degree of neutralization are also relevant factors (Table 2).4,5
The dermatologist should have knowledge of the peeling agents described below, as these are some of the most widely used.
Jessner SolutionJessner solution is a combination of resorcinol, salicylic acid, and lactic acid in 95% ethanol. Several layers are applied, producing a frost that indicates epidermal changes similar to those achieved with tretinoin. The possibility of allergic contact dermatitis to resorcinol can limit the use of this product. Combination with trichloroacetic acid (TCA) has been shown to produce a nonsignificant increase in efficacy in melasma and acne scars and to reduce postinflammatory erythema. However, no studies have demonstrated the efficacy Jessner solution alone in these indications.6
α-Hydroxy Acid Peelsα-hydroxy acid peels are characterized by their ease of use and low risk of complications, even in dark skins.7
Glycolic acid peels have a keratolytic effect (they reduce corneocyte cohesion and increase thickness of the stratum granulosum) and favor epidermal renewal. The epidermolytic effect is only observed at high concentrations after long contact periods. These are some of the most widely used peels for their anti-inflammatory and antioxidant properties. Additionally, they are able to induce dermal remodeling by stimulating fibroblasts.8
Lactic acid is an α-hydroxy acid with a similar mechanism of action to glycolic acid, as it causes breakdown of the desmosomes between corneocytes and induces desquamation and melanin dispersion. In addition, it increases the synthesis of collagen and glycosaminoglycans and inhibits tyrosinase.9,10
Salicylic acid is a β-hydroxy acid that, at concentrations of 3% to 5%, has keratolytic and acantholytic effects mediated by rupture of keratinocyte membranes. The keratolytic effect explains the improvement seen in alterations of pigmentation. In addition, its lipophilic nature gives it a high affinity for the pilosebaceous unit.11
Several studies have shown that the hydroxy acids have anticarcinogenic potential.12 A study performed in mice irradiated with UV light and subsequently treated with various types of peel (35% glycolic acid, 30% salicylic acid, 10% and 35% TCA) versus a control group (no peel) showed that the different agents were all able to reduce tumor formation. The application of peeling agents was found to delay the appearance of skin tumors and to significantly reduce the number of tumors compared with the control group, with no differences between the different agents. Furthermore, the immunohistochemical markers of photodamage, such as mutated p53, were expressed in the basal and middle layers of the epidermis of the controls, whereas the epidermis in peel-treated animals hardly expressed this mutation. A fall in prostaglandin 2 synthesis was also observed, which was interpreted as a prevention of UV-induced immunosuppression.
Pyruvic AcidPyruvic acid is an α-keto acid that is transformed to lactic acid, but it has certain peculiarities that give it a medium potency, as it can produce epidermolysis in less than a minute, with rapid penetration into the dermis. It has antimicrobial and sebo-regulatory properties and it induces collagen and elastic fiber synthesis. The vapors given off can cause irritation.13
PhenolPhenol is classified as a deep chemical peel. It shows rapid percutaneous absorption and high penetration into the reticular dermis, being one of the most predictable in terms of dermal penetration and neocollagenesis.14 This agent is usually applied using the Baker-Gordon formula, which combines 3ml of 88% phenol with 2ml of distilled water, 8 drops of septisol, and 3 drops of croton oil. The croton oil is responsible for deep penetration. This peel is very painful and is associated with a risk of cardiac arrhythmias and of kidney and liver toxicity; it must therefore be performed in the operating room under sedation and with continuous monitoring of vital signs.
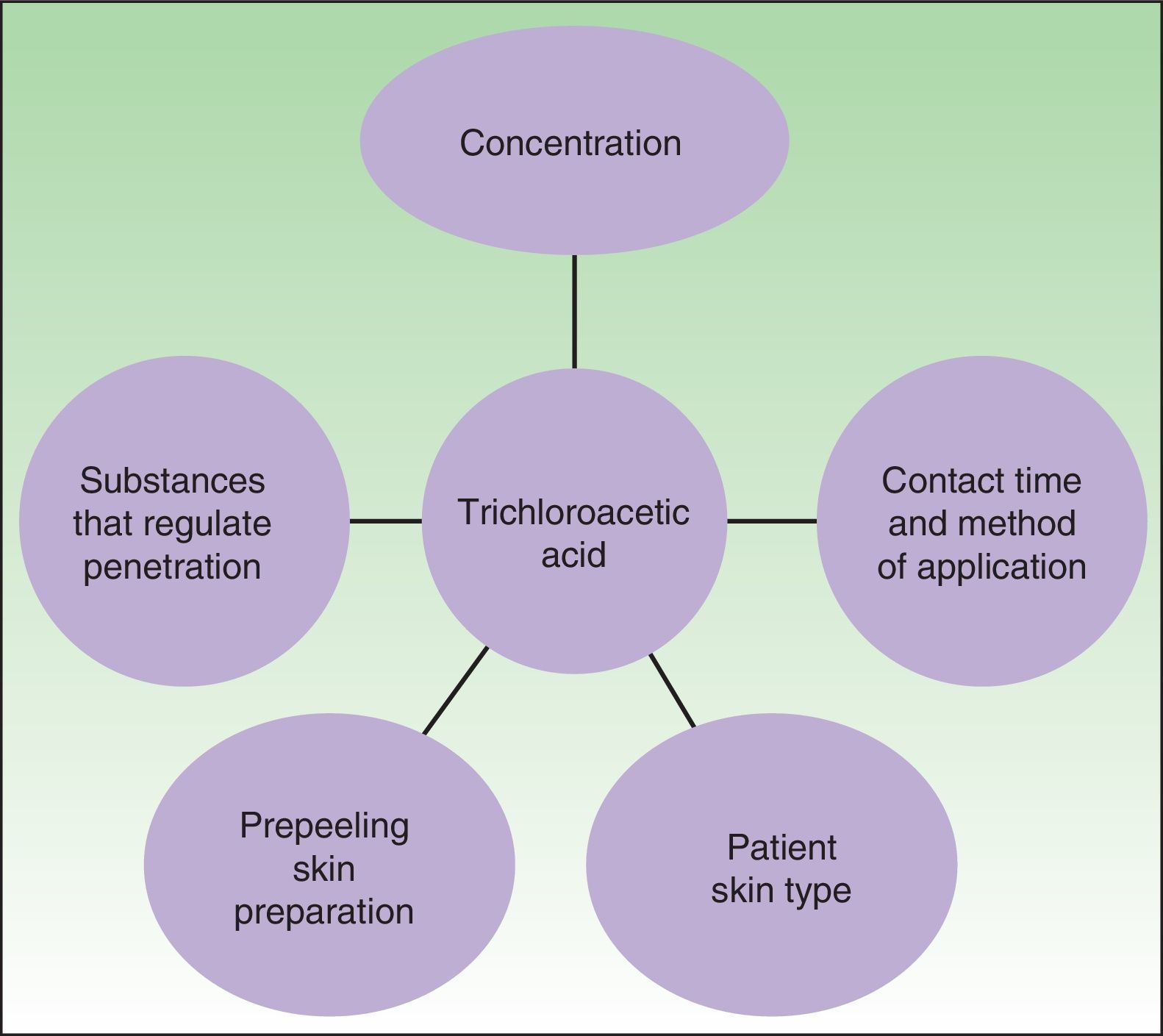
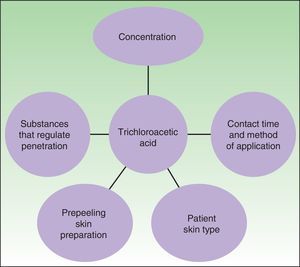
Trichloroacetic Acid PeelsTCA is derived from acetic acid by the chloration of 3 hydrogen ions. A particular characteristic of this agent is that it can induce coagulative necrosis of proteins and cells. The depth of action depends on various factors, most importantly the number of layers applied and its combination with substances that potentiate its action (croton oil, Jessner solution) or that regulate its cutaneous penetration, such as the saponins (Fig. 1).
Factors that determine the peeling action of trichloroacetic acid. Source: Vavouli et al.10
As mentioned above, TCA peels are usually classified into superficial, medium, or deep, depending on their concentration, although, to be more precise, the concentration actually determines the speed of skin penetration.15 In general, higher concentrations penetrate more rapidly and denature greater amounts of protein, producing a deeper peel; they are also associated with a higher risk of complications. Concentrations of 10% to 35% are typically considered superficial, producing the elimination of superficial alterations of pigmentation, superficial wrinkles, and perhaps some scars; concentrations of 35% to 50% are considered medium peels and improve deeper wrinkles, pigmentation, and scars, and produce a marked improvement in skin firmness.
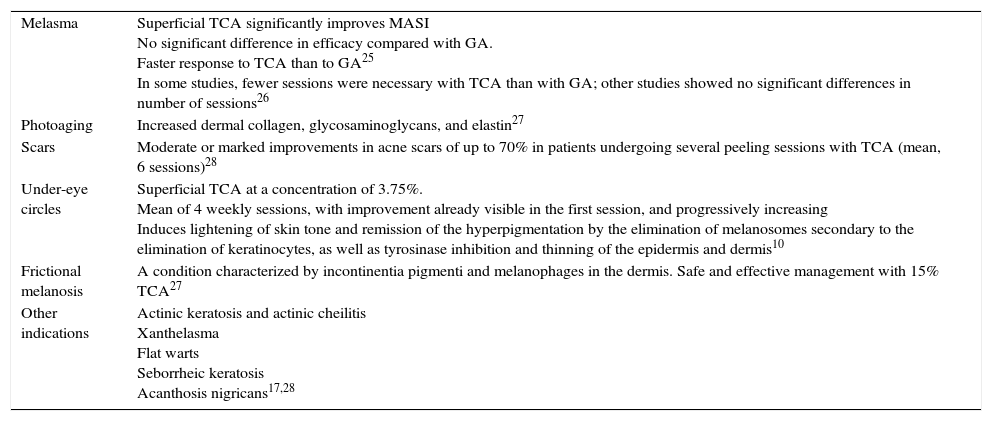
IndicationsThe main indications for TCA peels are listed in Table 4. Complications that can develop after a TCA peel are the same as those that encountered with other peeling agents. One of the most important factors in the risk of complications is skin phototype, with a higher risk of postinflammatory hyperpigmentation in the higher phototypes. As with the majority of peels, but in this case in particular, prior preparation of the skin is recommended.
Main Indications for Trichloroacetic Acid Peels.
| Melasma | Superficial TCA significantly improves MASI No significant difference in efficacy compared with GA. Faster response to TCA than to GA25 In some studies, fewer sessions were necessary with TCA than with GA; other studies showed no significant differences in number of sessions26 |
| Photoaging | Increased dermal collagen, glycosaminoglycans, and elastin27 |
| Scars | Moderate or marked improvements in acne scars of up to 70% in patients undergoing several peeling sessions with TCA (mean, 6 sessions)28 |
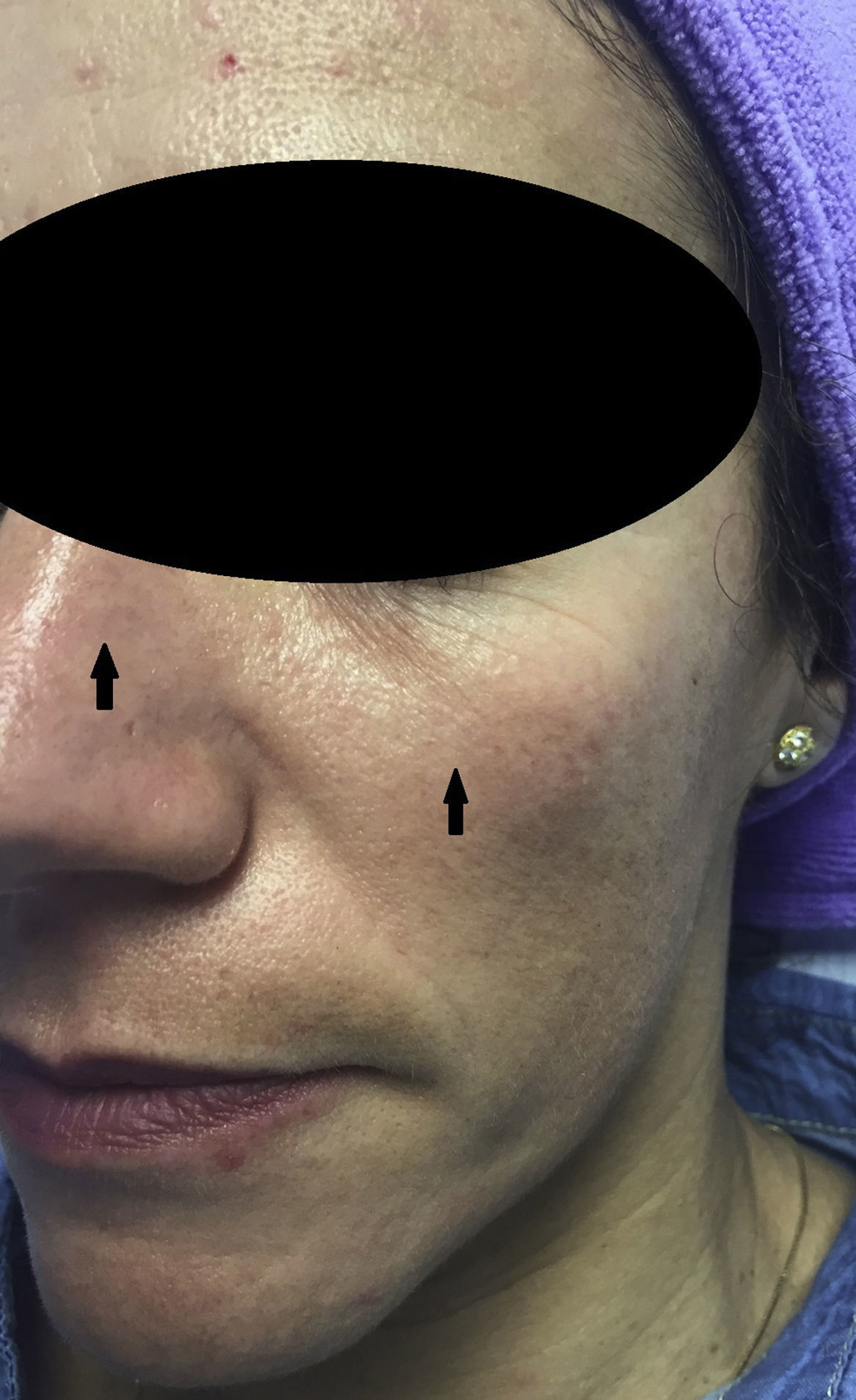
| Under-eye circles | Superficial TCA at a concentration of 3.75%. Mean of 4 weekly sessions, with improvement already visible in the first session, and progressively increasing Induces lightening of skin tone and remission of the hyperpigmentation by the elimination of melanosomes secondary to the elimination of keratinocytes, as well as tyrosinase inhibition and thinning of the epidermis and dermis10 |
| Frictional melanosis | A condition characterized by incontinentia pigmenti and melanophages in the dermis. Safe and effective management with 15% TCA27 |
| Other indications | Actinic keratosis and actinic cheilitis Xanthelasma Flat warts Seborrheic keratosis Acanthosis nigricans17,28 |
Abbreviations: GA, glycolic acid; MASI, Melasma Area and Severity Index; TCA, trichloroacetic acid.
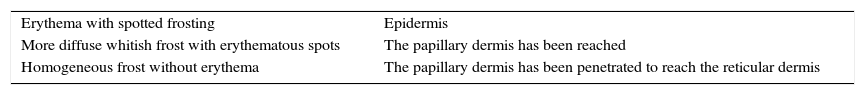
TCA induces reepithelialization, dermal remodeling, and cosmetic improvement through the coagulation of dermal and epidermal proteins.16–19 This agent does not need to be neutralized, because the irreversible protein coagulation induced by the chemical substance limits its penetration and also prevents its systemic absorption. TCA presents rapid self-neutralization at the concentrations used for both superficial and medium peels. This is observed as the slow formation of a white frost on the skin; in the superficial peel this is a pseudofrost. Neutralization occurs more slowly at concentrations over 50%, and the risk of greater penetration increases (Table 5).
Relationship Between Dermatologic Signs and the Depth of Peeling With Trichloroacetic Acid.
| Erythema with spotted frosting | Epidermis |
| More diffuse whitish frost with erythematous spots | The papillary dermis has been reached |
| Homogeneous frost without erythema | The papillary dermis has been penetrated to reach the reticular dermis |
The action of TCA on the epidermal cells induces the production of growth factors and cytokines, including platelet-derived growth factor B, tissue growth factor-α1 and β1, vascular endothelial growth factor, interleukin-1 and interleukin-10.20 Specifically, platelet derived growth factor increases in the cytoplasm of keratinocytes immediately after contact with TCA, but returns to normal levels within 24hours, when the epidermis is totally necrotic. This release of growth factors before necrosis plays a role in the reepithelialization and dermal regeneration characteristic of TCA. The only change identified in fibroblasts is an increase in the synthesis of keratinocyte-derived growth factor.20
Mode of UsePrior to the application of TCA, the skin is cleaned and degreased with alcohol or acetone to ensure uniform penetration of the agent. Topical anesthesia is not recommended as this could cause vasoconstriction, which would affect the concentration of the agent. TCA is applied using cotton buds or gauze swabs and always in a sequential manner until the desired frosting is achieved. Vaporized water or moisturizing cream can then be applied to relieve the burning sensation. The peeling is sealed using retinol cream.
Commercial peels are available that combine low concentrations of phenol with salicylic and other components. These peels are applied in exactly the same way as commented above.
The method of application of other peeling agents is similar, with certain peculiarities. In the case of glycolic acid, successive layers are applied with a gauze swab or brush until the patient reports an intense stinging sensation, the erythema is very intense, or whitish areas begin to appear; the peel is applied for a maximum of 3minutes in the first session and longer in successive sessions, depending on the tolerance of the patient. In this case, erythema is observed rather than a frost (Fig. 2), with a whitish appearance in areas of greater penetration; a grayish color indicates excessive penetration and must be avoided. Glycolic acid peels are neutralized with bicarbonate solution, which is applied until the patient states that the pruritus has resolved in all areas—pruritus indicates continued action of the acid.
The peculiarity of salicylic acid peels is that the patient reports an intense but transient burning sensation early in the process. Two to 4 layers are applied, waiting a couple of minutes between each layer to see if pseudofrosting develops. The appearance of a pseudofrost marks the end-point of the peel (Fig. 3). Fanning the patient should be avoided so as not to accelerate the crystallization process. Salicylic acid peels are usually removed with water (although this is not essential) to relieve the soreness.
A number of placebo controlled studies have shown that prior preparation with topical retinoids when using TCA peels will improve the regeneration process.21,22 Combination with retinoids improves the results by reducing the risk of complications and by accelerating epidermal regeneration.22 This is due to its capacity to compact the corneal layer, increase epidermal thickness, increase glycosaminoglycan concentration, increase vascularization, and reduce melanin synthesis. No standard prepeeling protocols have been drawn up for this agent, but the use of retinoic acid or retinol for 3 or 4 weeks prior to the peel is sufficient, in our experience, to optimize treatment.23
A new TCA combination called the ZO 3-Steps peel (Industrial Farmaceutica Cantabria, Santander, Spain) is now available in Spain. The first step is the application of a 10% solution of TCA combined with 5% lactic acid, 17% salicylic acid, and saponins to induce rapid neutralization. The second step consists of the application of 6% retinol, followed by the avoidance of contact with water for at least 5hours so as not to interrupt stimulation by the retinol. In the third step, a calming cream is applied. Exfoliation with this type of peel is very predictable and occurs on the third to fifth days. The aim of combining distinct chemical agents in a single peel is to increase efficacy and tolerance compared with the agents when used separately.
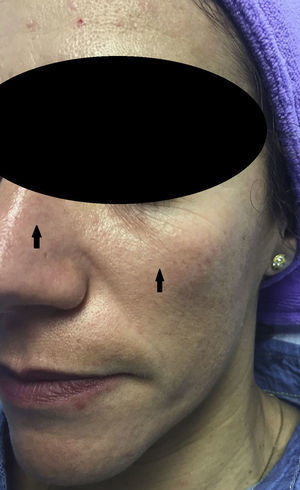
Experience in a series of 9 patients with melasma and photoaging treated with a single session of ZO 3-Step peel revealed clinical improvement with a high degree of safety. In patients with melasma, a marked increase was observed in luminosity and a reduction in skin roughness and seborrhea at 1 month after performing the peel. In patients with photoaging, improvement was observed in fine wrinkles, macules, telangiectasias, and sebaceous hyperplasia. The majority of patients reported an excellent improvement, similar to the results reported by the dermatologist. It should be noted that follow-up was only of a month and, as melasma shows a high tendency to recurrence and can occasionally deteriorate after performing a peel, these treatments must always be performed with maximum attention to safety (correct preparation, preferably in patients with stable, inactive melasma) (Figs. 4–6).
Combined peels have the advantage of acting on several pathways, with a synergic effect between the distinct components (exfoliation with the cocktail of acids, dermal stimulation with the retinol), minimizing possible side effects by using lower concentrations, and accelerating regeneration, which shortens the recovery period.
Combinations of TCA with other cosmetic procedures have also been investigated, showing synergic effects.24 TCA has been used in methods of skin rejuvenation in combination with other techniques such as botulinum toxin injection or ablative carbon dioxide laser. It has also been combined with other peeling agents such as phenol, Jessner solution, or tretinoin.17
In conclusion, chemical peels continue to be safe and effective tools that improve a number of cosmetic skin conditions without significant economic outlay. To optimize the cosmetic result and avoid the possible complications associated with peelings, it is essential to know the correct indications, to transmit realistic expectations to the patient, and to have in-depth knowledge of the technique for the application of each agent.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestM. T. Truchuelo is a consultant for Industrial Farmaceutica Cantabria.
The other authors declare that they have no conflicts of interest
We would like to thank Dr. M. Vital, dermatologist and medical director of the Medical Affairs and Research Department of Industrial Farmaceutica Cantabria, who participated in the review of this article.
Please cite this article as: Truchuelo M, Cerdá P, Fernández LF. Chemical Peeling: A Useful Tool in the Office. Actas Dermosifiliogr. 2017;108:315–322.