Merkel cell carcinoma (MCC) is a particularly aggressive tumor whose incidence has grown significantly in recent decades.1–3 Approximately 80% of MCCs contain Merkel cell polyomavirus, which was discovered in 2008.4 Although MCC is an aggressive tumor, about 40 cases of spontaneous regression have been described to date.5,6 We report on 2 patients who experienced complete regression of MCC after biopsy.
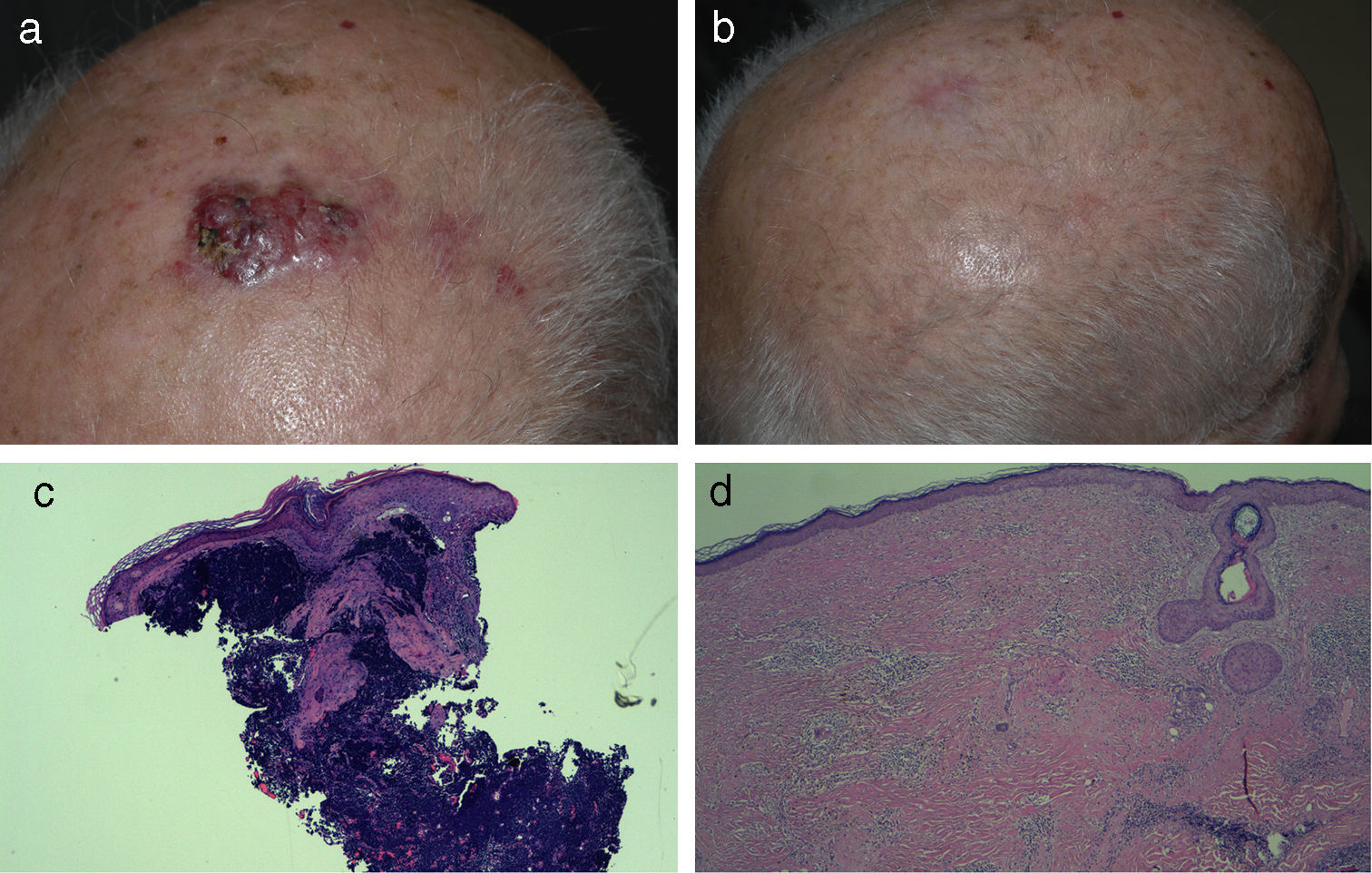
The first patient was a 69-year-old man with a history of hypertension and type 2 diabetes mellitus. Four months before being seen at our unit, he developed a fast-growing polylobulated nodular lesion with a diameter of 3cm in the parietal region. He also had 2 papules indicative of satellite metastases that measured 4 to 5mm and were located in the right parietal region, about 3 to 4cm from the primary tumor (Fig. 1A). Biopsy showed a proliferation of basophilic cells that stained positive for synaptophysin and negative for cytokeratin 20. Merkel cell polyomavirus was detected by polymerase chain reaction. A primary neuroendocrine tumor involving the internal organs was ruled out and despite the negative staining for cytokeratin 20, a diagnosis of primary cutaneous MCC was made. The patient was referred to the Plastic Surgery Department and scheduled for wide excision of the lesions and sentinel lymph node biopsy. Five weeks later, when the patient was seen in the operating room, the lesions had regressed (Fig. 1B). Biopsy of the residual lesion where the primary tumor had been showed only fibrosis and an inflammatory infiltrate (Fig. 1C & D). No adjuvant treatment was administered. After 4 years of follow-up, there have been no recurrences or metastasis.
Patient 1. A, Clinical image of Merkel cell carcinoma on the scalp. B, Appearance of scalp after regression of the lesions. C, Histologic image of initial biopsy of the scalp tumor showing a dense dermal proliferation of basophilic cells (hematoxylin-eosin, original magnification×40). D, Histologic image of biopsy of scalp tumor after regression, showing only residual fibrosis and a mild chronic inflammatory infiltrate (hematoxylin-eosin, original magnification×100).
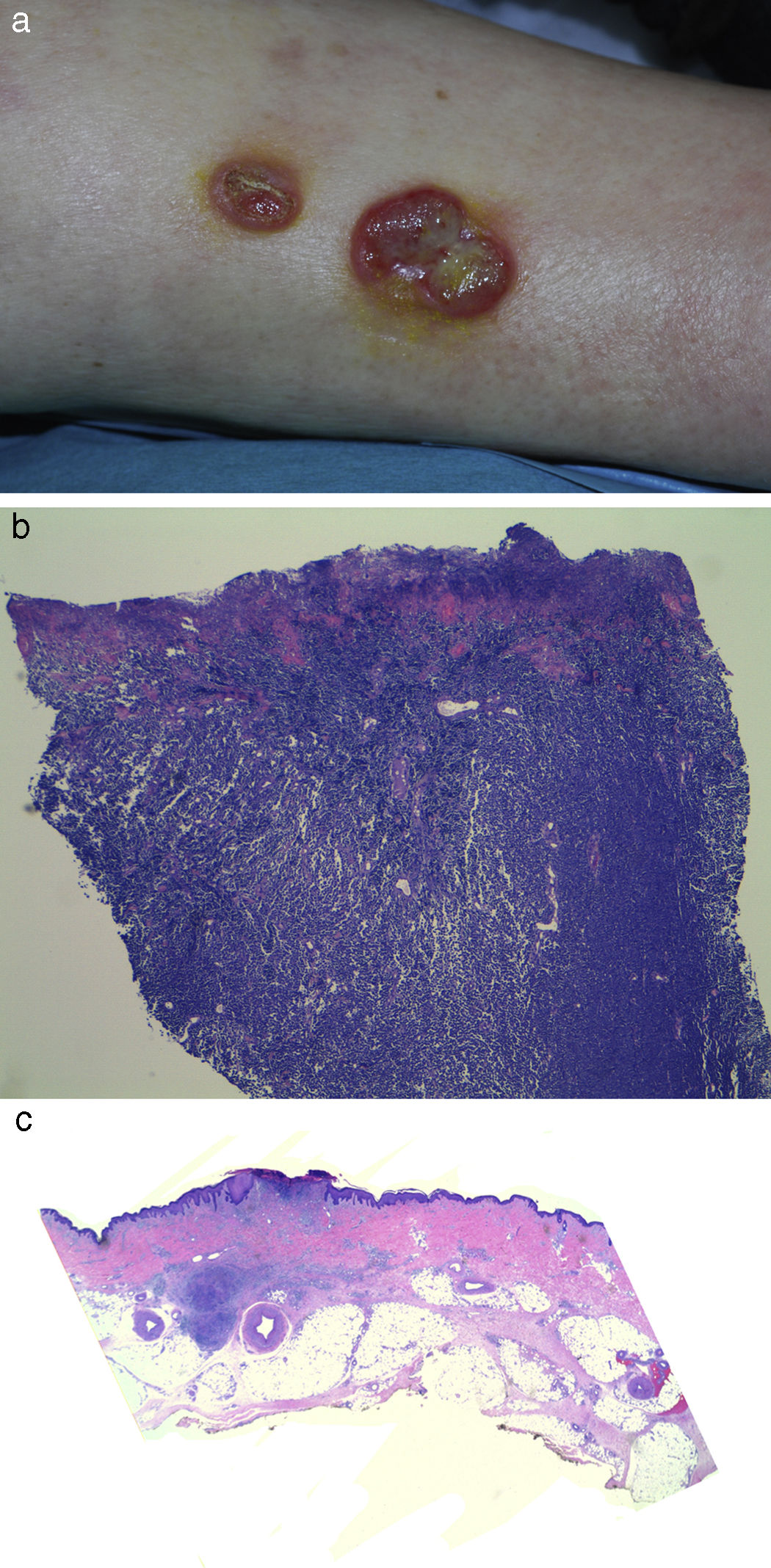
The second patient was a 72-year-old woman with a history of type 2 diabetes mellitus and a cerebrovascular accident with serious sequelae. She was referred to our unit with 2 polylobulated nodular lesions of 3 to 4 months’ duration located in the left pretibial region. The lesions were ulcerated and measured 2.5cm (proximal) and 5cm (distal) (Fig. 2A) Biopsy showed a proliferation of basophilic cells that were positive for both synaptophysin and cytokeratin in the immunohistochemical study and exhibited a dot-like paranuclear pattern (Fig. 2B). Merkel cell polyomavirus was detected by immunohistochemistry. The patient was referred to the Plastic Surgery Department for wide excision and sentinel lymph node biopsy. At the time of the operation 4 weeks after the biopsy, the lesions were no longer elevated and had the appearance of 2 nonspecific ulcers. They were excised using the same elliptical incision. The histologic study showed intense residual fibrosis and an accompanying infiltrate in the 2 ulcers. At the base of the proximal ulcer, there was a 2.5-mm tumor nest formed by basophilic that stained positive for synaptophysin and cytokeratin 20 (Fig. 2C). The sentinel lymph node biopsy was negative. Adjuvant therapy was not administered because of the patient's underlying disease. The patient died of urosepsis 2 years after diagnosis of the MCC. There were no signs of tumor recurrence in this period.
Case 2. A, Clinical image of Merkel cell carcinoma in pretibial region showing 2 ulcerated tumors. B, Histologic image of initial biopsy from 1 of the tumors showing a dense dermal proliferation of basophilic cells (hematoxylin-eosin, original magnification×40). C, Histologic low-magnification detail of 1 of the pretibial tumors after regression, showing intense residual fibrosis and a lymphocytic infiltrate. Biopsy showed just a tumor nest measuring 2.5mm and formed by basophilic cells at the base of the proximal ulcer (hematoxylin-eosin, original magnification×20).
Complete regression is defined as the spontaneous disappearance of an entire tumor without treatment.6 The estimated incidence of regression in MCC is 1.7% to 3%.7 Most cases have been reported in women aged around 80 years old with head and neck lesions.5,6 In most cases, regression was observed after a biopsy or incomplete resection and often within 3 months of the initial clinical presentation.5 Some authors have suggested that biopsy might trigger the spread of viral components capable of stimulating an immune response to tumor cells infected by Merkel cell polyomavirus.6 The mechanism responsible for this regression, however, has not been established. Some authors have suggested cell immunity as a possible cause,5 while others have proposed apoptosis of neoplastic cells.8
Complete regression seems to have a better prognosis in MCC than in other tumors such as melanoma. None of the patients who have experienced complete regression of MCC in the reports in the literature died because of recurrence during follow-up, but there have been many reports of metastasis in patients with melanoma following complete regression.6
Although it has not been possible to detect polyomavirus in some cases of MCC that have undergone complete regression,6 it has been suggested that the infectious etiology of this tumor might make the neoplastic cells more susceptible to the host's immune response.5 Merkel cell polyomavirus cells were detected in both our patients.
Fifty-one patients have been diagnosed with MCC at our hospital since 1988 and 2 of them have experienced complete spontaneous regression of a primary MCC. This corresponds to an incidence rate of 3.92%. Coinciding with reports in the literature, neither of the patients showed signs of recurrence. In our experience, complete regression of MCC is not uncommon and appears to be associated with a good prognosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Marcoval J, Valentí-Medina F, Penín RM, Bermejo J. Regresión completa espontánea del tumor primario en el carcinoma de células de Merkel. Actas Dermosifiliogr. 2018;109:752–754.