Molluscum contagiosum infection is very common in children and is one of the most frequent reasons for consultation in outpatient and hospital pediatric care.1 Infection occurs as a result of direct person-to-person contact through infected skin, contact with fomites, or autoinoculation.2 In adolescence and adulthood, infection may occur through sexual contact. Occurrence during the neonatal period is rare.
Case 1A 12-month-old girl with no relevant history born following a full-term pregnancy and vaginal delivery. The patient was brought for consultation due to 3 congenital lesions in the left occipital region. The patient's mother reported a history of molluscum contagiosum infection of the groin and the labia majora during pregnancy; the diagnosis was confirmed at the time by biopsy. An examination of the girl revealed 2 translucent umbilical papules 1 and 2 mm in diameter and another papule 4 mm in diameter with a crusted surface. The clinical suspicion of molluscum contagiosum was confirmed following curettage of the lesions (Fig. 1).
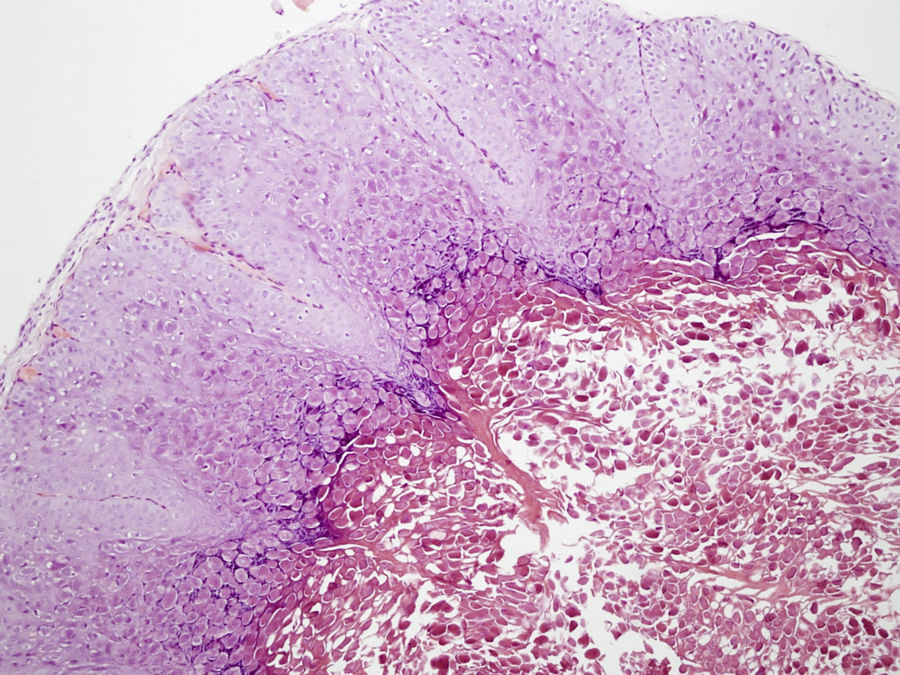
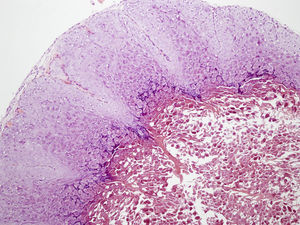
Case 2A 2-year-old boy with no relevant history was brought for consultation due to a lesion on the right shoulder which had developed in the first 4 days of life and had grown over the previous months. He had been born following a full-term pregnancy and vaginal delivery. The mother was healthy and had no history of cutaneous lesions. An examination revealed a single papule 6 mm in size on the right shoulder. The papule had well-defined borders, was the color of normal skin, and had a slightly umbilicated center (Fig. 2). Based on a clinical suspicion of molluscum contagiosum, curettage was performed of the lesion following application of a topical anesthetic cream. The procedure was carried out with ease and the lesion was removed completely. The pathology findings were consistent with molluscum contagiosum (Fig. 3).
Molluscum contagiosum is caused by a member of the poxvirus family, and manifests clinically as a flesh-colored or translucent, pearl-like papule with an umbilicated center measuring 1 to 5 mm in diameter.3 The most frequently affected areas are the trunk, the limbs, and the scalp. The diagnosis of this disorder is clinical. A pathology study is performed only occasionally, when the diagnosis is uncertain. Histology reveals a well-defined hyperplastic lesion of the epidermis sometimes with a central crater, and, commonly, eosinophilic inclusion bodies within the keratinocytes that later become basophilic inclusion bodies as they rise in the epithelium.4 Molluscum contagiosum infection results in benign lesions that usually resolve spontaneously, although this may take months to years.5 Treatment is the subject of debate. Because of the self-resolving nature of the disease, one option is no treatment. The aim of active treatment is to prevent contagion and autoinoculation. A number of treatment approaches exist, but these are all the subject of debate and none are free of risk; some examples include topical treatments (e.g., cantharidin, potassium hydroxide 5%, salicylic acid, imiquimod, tretinoin, podophyllotoxin, topical cidofovir, tincture of iodine, trichloroacetic acid) and physical treatment with cryotherapy, curettage, electrosurgery, or laser.6,7
Few cases of congenital molluscum contagiosum lesions or molluscum contagiosum developing in the neonatal period have been described in the literature. A search of PubMed yielded only 9 cases of molluscum contagiosum lesions presenting congenitally or in the first days of life. In 6 of these cases the lesions were located on the scalp, with the rest appearing on the foot, the thigh, and the sacrum.3,8–10 Only the most recently published of these cases reports in the clinical history that the mother had a history of molluscum contagiosum infection.10
The authors of the previous cases all agree that the infection may have occurred through vertical transmission during delivery. This same mechanism is behind other viral infections such as those caused by the herpes virus and the human papillomavirus. The human papillomavirus has a long latency period from infection to clinical manifestation, potentially leading to laryngeal papillomatosis or common warts appearing years after infection; the incubation period of molluscum contagiosum, on the other hand, is quite short (2-8 weeks), thus causing the lesions to appear in the neonatal period.5
We have presented 2 new cases of congenital molluscum contagiosum, including a case of maternal genital infection during pregnancy and delivery. This is the second case to appear in the literature in which molluscum lesions that developed during gestation were treated and the diagnosis was confirmed by histological study. These histological findings provide firm support for the theory of vertical transmission of the virus during delivery. In the second case, the lesions appeared on the shoulder, a location not described previously. In cases where the mother's genitals are not identified as infected, transmission probably occurs through undiagnosed vaginal infection, as the poxvirus causing molluscum contagiosum may also affect the mucous membranes.
It is important to consider congenital molluscum contagiosum as a possible diagnosis in neonatal patients with one or more umbilicated papules.
Please cite this article as: Méndez C, Vicente A, Suñol MA, González-Enseñat M. Molluscum contagiosum congénito. Actas Dermosifiliogr. 2013;104:836–837.