We describe the case of an 84-year-old woman who consulted our dermatology department with facial actinic keratosis that had been treated with cryotherapy on several occasions. Her medical history included a gastric adenocarcinoma treated with gastrectomy over 30 years earlier.
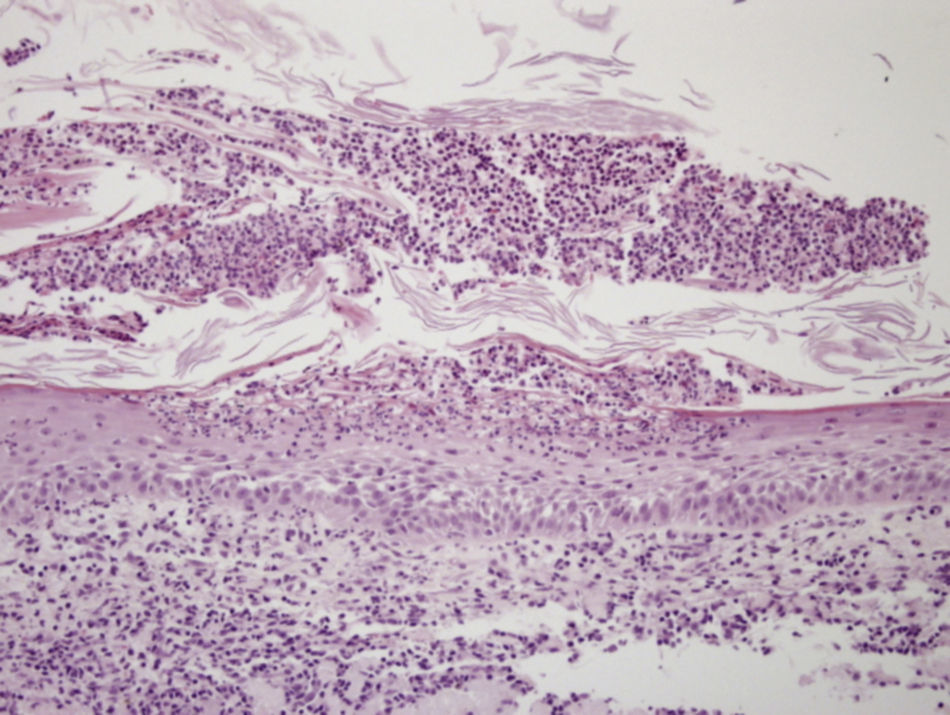
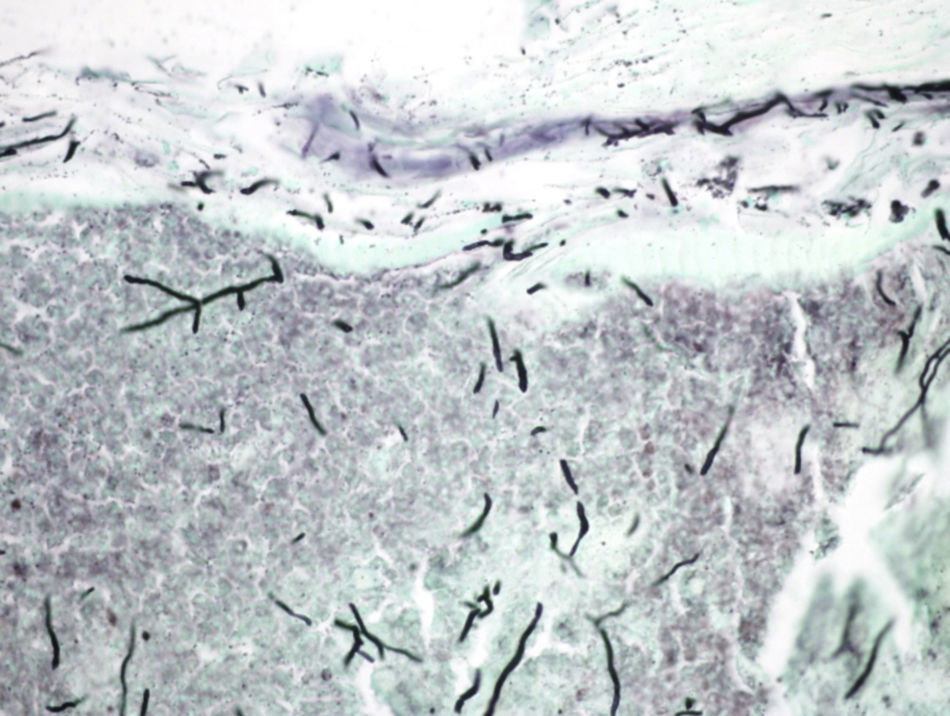
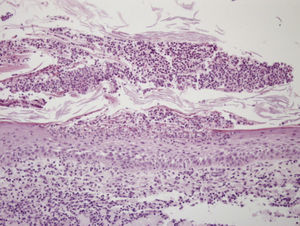
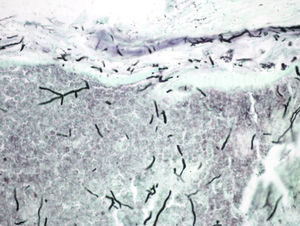
She presented with persistent crusted pustular lesions that had appeared on her forehead (Fig. 1) 3 months earlier, following the application of liquid nitrogen. Biopsy showed multiple pustules with acute inflammation and a large number of septate hyphae measuring approximately 2μm in diameter with dichotomous acute-angle branching (45°) (Figs. 2 and 3). Culture of one of the lesions was positive for Aspergillus niger and Klebsiella oxytoca.
A full laboratory workup showed iron-deficiency anemia but all the other results were within normal limits. There was no evidence of masses or infiltrates on the chest radiograph.
We established a diagnosis of primary cutaneous aspergillosis following cryotherapy in an immunocompetent patient. Based on the antibiogram, we initiated treatment with oral ciprofloxacin (500mg/12h) for 2 weeks and oral itraconazole (100mg/12h) for 6 weeks. At follow-up, the lesions had resolved and the culture findings were negative.
Aspergillus species are filamentous fungi found in humid environments or in decaying organic matter.1 They are among the most common fungi as they can tolerate a wide range of temperatures and produce large numbers of spores, which are easily dispersed by air. They form part of the normal outdoor flora but they also tend to enter hospital buildings through windows and ventilation systems. They can cause allergic hypersensitivity and may act as opportunistic pathogens causing local or disseminated infection. The main routes of entry are inhalation of spores or penetration of spores during surgery or other invasive procedures, or following a break in skin integrity.
Primary cutaneous aspergillosis is a chronic skin infection that does not appear to affect other organs. It is very uncommon as it is caused by the direct inoculation of the fungus into injured skin. It tends to affect preterm neonates2 and immunocompromised patients and is much rarer in immunocompetent individuals.3-5 The lesions, which are usually located at the site of inoculation, are nonspecific and include erythematous macules, pustules, plaques, and nodules that can become necrotic.2,5-7 The differential diagnosis should include other fungal or bacterial infections, insect bites, noninfectious pustulosis, vasculitis, ecthyma, polyarteritis nodosum, and pyoderma gangrenosum.2 It is essential to rule out systemic disease in immunocompromised patients, as there is a risk of progression to invasive disease, with spread to other organs and high associated morbidity and mortality. Diagnosis is based on histologic examination, which reveals hyaline septate hyphae with a diameter of between 2 and 4μm and dichotomous acute-angle branching (45°).5,6 Culture of a lesion or biopsy sample enables identification of the species.4 Immunocompetent individuals with exclusive skin involvement can be treated with oral itraconzole,1,5,6 but the treatment of choice in patients with invasive disease is voriconazol.3,7 Echinocandins (caspofungin, micafungin, and anidulafungin) are licensed for use in invasive aspergillosis that is refractory to standard treatment. Surgical resection with wide margins is recommended in patients with extensive tissue necrosis.6
Secondary cutaneous aspergillosis occurs when the infection spreads to the skin from another organ by hematogenous dissemination. It is a very serious condition that affects immunodepressed patients.
In a review of the indexed literature, we found no reports of primary cutaneous aspergillosis following cryotherapy, although cases associated with burns due to other causes have been reported.
The Klebsiella oxytoca isolated in the culture was probably a contaminant as this bacterium seldom causes infections of the skin and soft tissue.
Please cite this article as: Palomo-Arellano A, et al. Lesiones costrosas y pustulosas después de aplicar crioterapia. Actas Dermosifiliogr.2012;103:333-334.