Dermoscopy has improved diagnostic precision in the clinical evaluation of complex skin lesions by helping to pinpoint small clinically suspicious areas that are not visible to the naked eye but require histopathologic examination. Derm dotting is a new technique for selectively marking areas of interest to ensure they are examined under a microscope. Left unmarked, suspicious areas might not appear in routinely prepared cross sections or might be difficult to correlate with dermoscopic images. In vivo or ex vivo derm dotting involves the application of nail polish, which, unlike stains, leaves tissues unaltered. Dots can be placed by the dermatologist or laboratory staff during macroscopic preparation of the sample. Derm dotting is a simple, inexpensive technique that any dermatopathology laboratory can quickly adopt to improve diagnostic precision through better dermoscopic–histologic correlation.
La dermatoscopia ha aumentado la precisión en el diagnóstico clínico de lesiones cutáneas complejas. Es una herramienta que permite identificar pequeñas áreas de sospecha, no apreciables a simple vista y que requieren examen histopatológico específico. El derm dotting es un método de marcaje selectivo de zonas de interés para asegurar que estos focos son estudiados microscópicamente, puesto que por su pequeño tamaño podrían no aparecer en las secciones de rutina o ser difíciles de correlacionar con la imagen dermatoscópica. Combina la dermatoscopia in vivo o ex vivo con la aplicación de esmalte ungueal. A diferencia de los colorantes usuales, el uso de esmalte ungueal no altera la histología. Puede ser aplicado por parte del dermatólogo o durante el procesamiento macroscópico en el laboratorio. El derm dotting es una técnica novedosa, sencilla y económica, que puede implementarse rápidamente en cualquier Laboratorio de Dermatopatología. Mejora la precisión diagnóstica ya que traslada los hallazgos dermatoscópicos al estudio histológico.
Diagnostic precision has improved with the routine use of dermoscopy to evaluate skin lesions and identify very small clinically suspicious areas that cannot be seen by the naked eye. The lesions are then excised so that changes can be studied under a microscope.
The biopsied tissue is processed in a specialist histopathology laboratory. After routine macroscopic inspection of the material, a technician prepares representative tissue samples, which are usually consecutive cross-sections. However, if a small area with suspicious changes falls between 2 sections, it will not be included for histologic evaluation. In order to improve the precision of a histopatologic diagnosis, clinical dermoscopic findings should be taken into consideration and reflected in both the macroscopic inspection and the directed histologic assessment. Selective marking of the tissue is therefore extremely useful.
The first such marking technique was the micropunch, described by Braun et al,1 who designated the area of interest with a 1-mm punch without removing any of the tissue. Their technique was relatively complex, however, and had the great disadvantage of altering the underlying tissue.
Derm dotting, described by Scope et al2 and extensively validated by Haspeslagh et al,3 uses ex vivo dermoscopy to locate problematic areas and mark them with a dot of nail polish. The polish withstands the next steps in tissue processing, leaves the morphology unchanged, and helps the technician locate the problem area when examining the sections under a microscope. The same author group later retrospectively compared the diagnostic results for melanoma and nevus evaluations before and after implementing ex vivodermoscopy and derm dotting in 15 110 biopsy specimens.4 They found that the rate of melanoma diagnosis increased from 15.5% before implementation to 33.3% afterwards, and the detection of ulceration in melanomas of Breslow depth less than 1 mm increased from 24% to 31.3%. Diagnoses of nevus with moderate atypia rose from 1% to 7.2%, and nevus with severe atypia from 0.65% to 1.4%. The detection of affected margins after removal of nonmelanoma skin tumors rose from 8.4% before derm dotting to 12.8% afterwards. The diagnosis of collision tumors likewise increased, from 0.07% to 1.07%. Time until a histologic diagnosis was found to decrease.
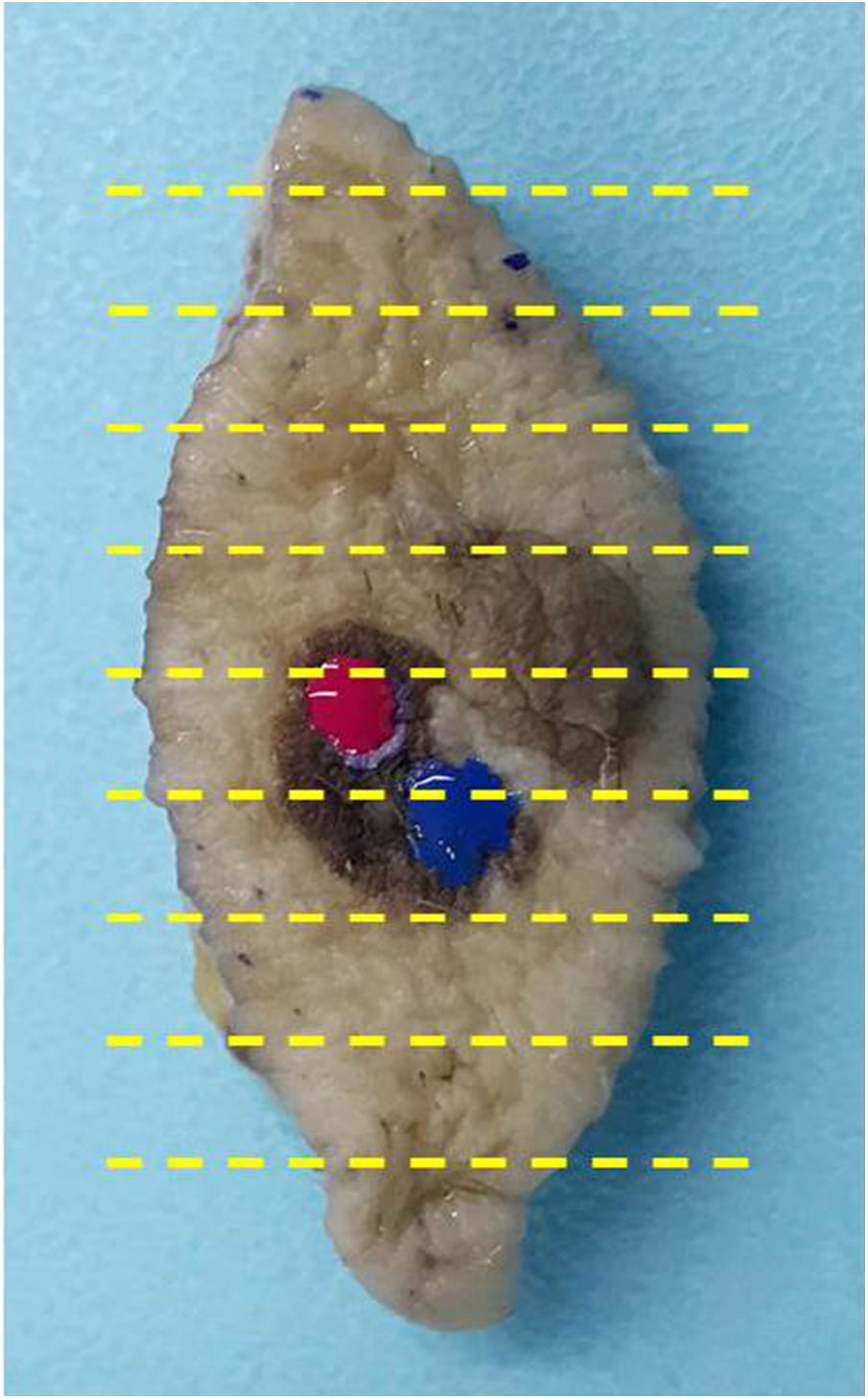
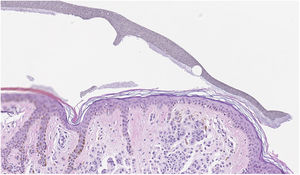
Material and MethodsDerm dotting involves using nail polish to selectively mark the areas of interest on skin or biopsied tissue. The points of focus (Fig. 1) are found with the aid of a dermoscope in vivo or ex vivo. The technique can also be used in the laboratory on formalin-fixed tissue, in which vascular patterns are lost but pigmentation patterns are enhanced.4 The laboratory technician can mark darker, lighter, or irregular areas of pigmented lesions as well as ulceration.
The area to be marked should be prepared before derm dotting begins. Hair, which will reduce the area of contact between the nail polish and skin, is first shaved; the field is then cleaned with alcohol to eliminate any substances that might interfere with adhesion.
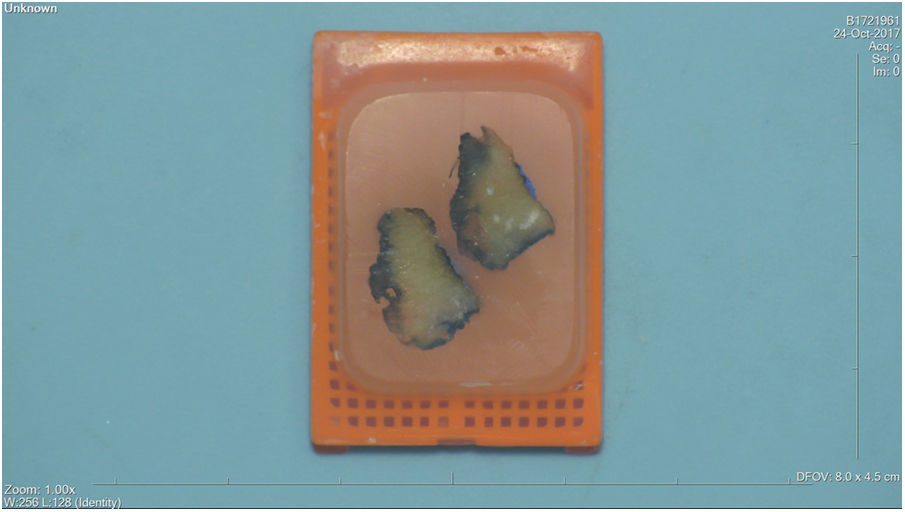
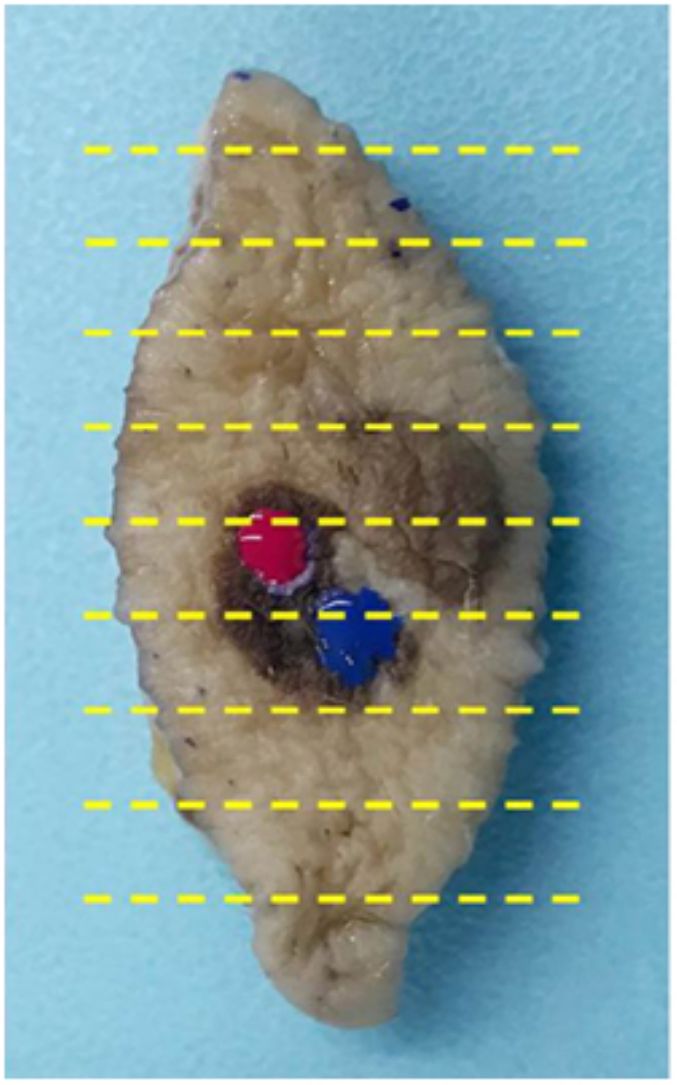
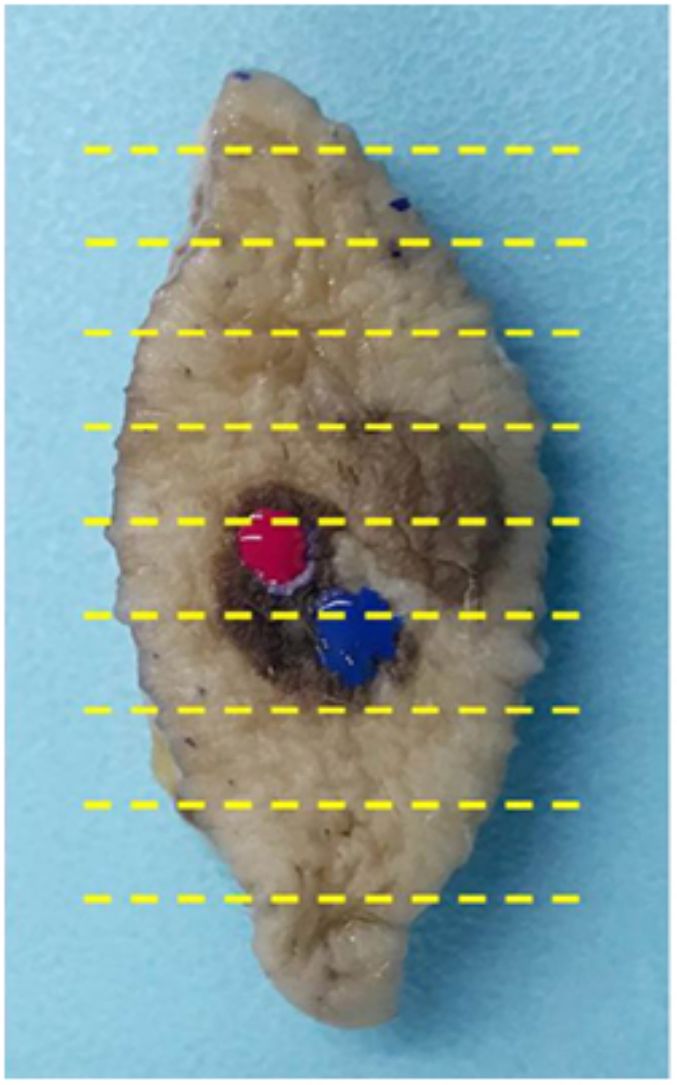
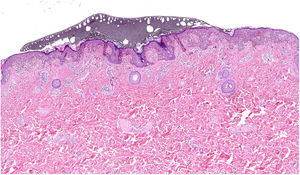
The 1- to 3-mm dots of polish, which can be applied with a brush (toothbrush or similar), dry quickly. Because the polish survives all the tissue processing steps, it serves to guide the cutting of cross-sections that provide optimal view of the areas of interest for diagnosis (Fig. 2). The original color of the polish remains unaltered in the paraffin block. It is important to try several commercial nail polishes in order to find the most suitable ones and to practice the application technique, observing how long drying takes.
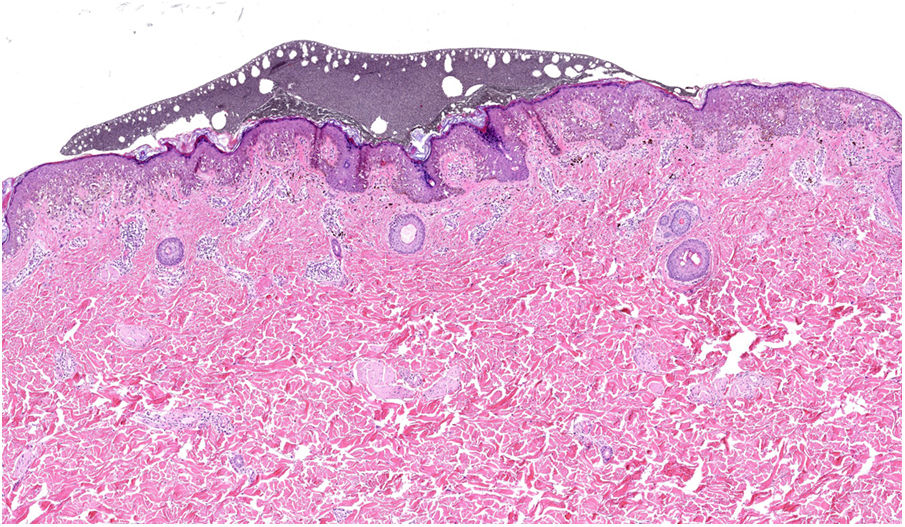
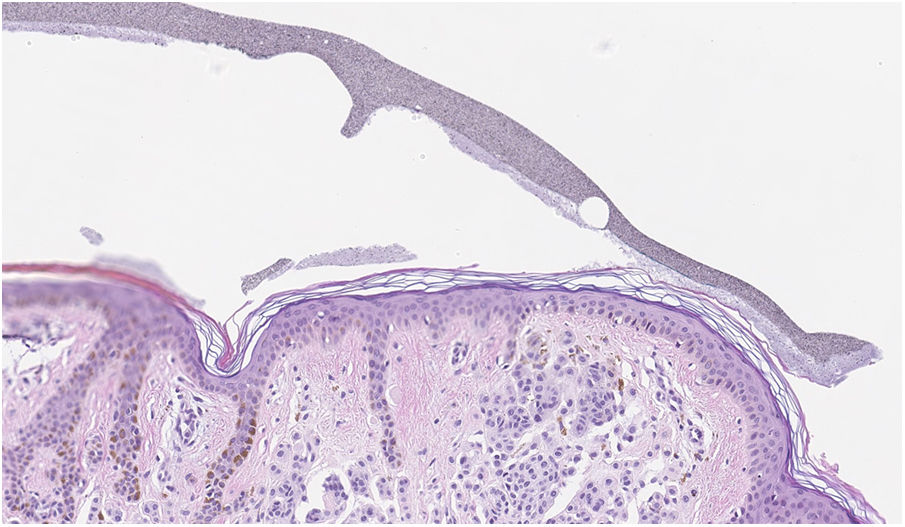
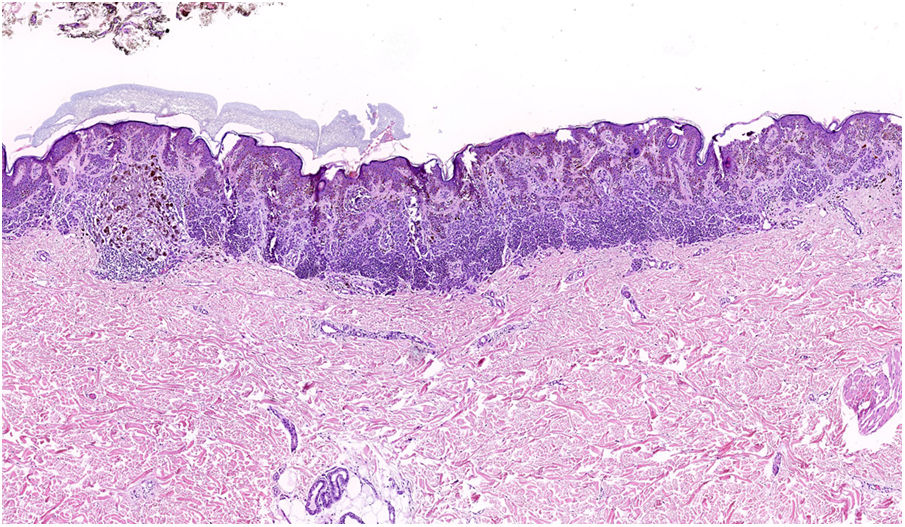
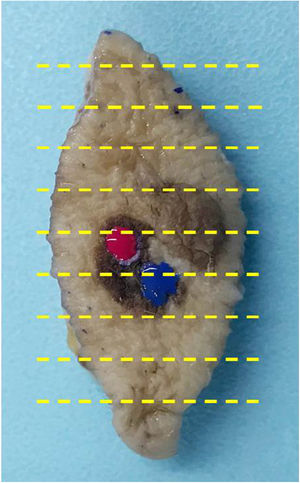
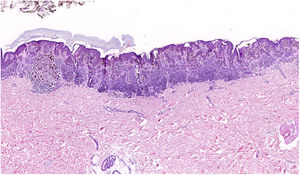
Under the microscope the polish will appear as a grayish granular area whose texture and tone vary according to the color used (Fig. 3). Small colored particles may also be visible: for example, points of yellow and blue might be observed if a green polish was applied. Several areas of interest can be marked within the same lesion by applying different colors, which will be recognized in the cross-sections by their differing gray tones. The best results are achieved by placing only a few dots of nail polish before removal of the lesion and later adding dots in the laboratory (Fig. 4).
Derm dotting has led to very good results in our practice. We went through a learning curve in which the laboratory technicians familiarized themselves with the use of ex vivo dermoscopy and tried different types of nail polish with varying textures and colors until they found the type that worked best. Nail polish is inexpensive, easy to find, and does not interfere with the technician's ability to evaluate the underlying tissue. Our parallel tests using histologic marking pens on the the surface of excised skin samples revealed the disadvantage of ink spreading on the stratum corneum and epidermis and into any fissure in the tissue, causing problems during tissue evaluation; we therefore abandoned use of these pens. The derm dotting technique has enabled us to provide more precise clinical-pathologic correlation and improve the histologic study of complex lesions by specifying the problem areas to focus on. We have applied the technique to melanocytic lesions and other types of tumors.
DiscussionSelective marking with derm dotting is a highly valuable tool for achieving accurate clinical-pathologic correlation when examining areas that in vivo or ex vivo dermoscopy reveals to be suspicious. Dermatopathologic analysis is optimal when points of interest are clearly identified. As a result, fewer additional sections need to be examined, leading to savings in laboratory time and costs and shortening the time to diagnosis.
We list some of the possible applications of this approach:
- -
Melanocytic lesions, where derm dotting is of greatest interest (Fig. 5): Before removing the lesions, the dermatologist can mark one or more areas of interest seen through the dermatoscope. Examples are the locations of the greatest degree of atypia, atypical points or globules, a blueish-whitish veil, or structureless or pigmented zones. Ulceration, which is particularly important for staging melanomas, can go unnoticed with traditional approaches to evaluation. In contrast, a dot of nail polish provides an easy-to-follow guide for slicing the tissue just near the ulcerated zone so that a melanoma can be accurately staged.
- -
Nonmelanocytic lesions: Ulcerated areas of basal cell carcinomas can be marked, as these zones usually coincide with the points of maximum depth. Derm dotting can also provide useful guidance for evaluating collision tumors or lesions that are asymmetrical or have differentiated portions. In porokeratosis, dots can also be used to mark the hyperkeratotic border and identify the cornoid lamella.
- -
Orientation of the sample: The cranial orientation of a tissue sample can be indicated with derm dotting without resort to the traditional placement of a suture for reference. Such sutures cause artifacts that make it difficult to evaluate the surrounding tissue.
- -
Surgical margins: A narrow margin can easily be marked on the epidermis if we suspect it might be affected or if its anatomical location is a cause for concern.
Derm dotting is a new, highly useful technique that is simple, economical, and easy to incorporate into the routine practice of any dermatopathology laboratory. Taking dermoscopy findings into consideration and communicating them to the laboratory by selectively marking tissue samples clearly favors more precise diagnosis of complex lesions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Moreno Romero JA, Pérez Muñoz N, Campoy Sánchez A, Urbano Carrillo M, Fernández Figueras MT. Derm Dotting: A New Technique That Improves Diagnostic Precision in the Evaluation of Skin Lesions. Actas Dermosifiliogr. 2019;110:193–196.