Sensitive skin has traditionally been viewed as a cosmetic problem or as a purely psychosomatic alteration with a major subjective component. Different studies of its pathophysiologic etiology, however, have shown it to be a complex entity that several authors now consider to be a neurodermatological syndrome. Because of this complexity, skin sensitivity can be difficult to diagnose and treat, particularly considering that it may present with another disease. Simple tools applicable to clinical practice are thus necessary to identify and manage this disease as an independent entity. In this study, we perform a practical review of the most recent scientific advances in the area of sensitive skin that justify it being considered an individual entity, and provide tools for its identification and treatment. We propose diagnostic and treatment algorithms based on evidence from the literature and our experience and expertise.
Tradicionalmente, la piel sensible se ha considerado como un problema cosmético o como una alteración puramente psicosomática con un fuerte componente subjetivo. Sin embargo, diversos estudios científicos sobre sus procesos fisiopatológicos y su etiopatogenia han demostrado que se trata de una entidad compleja que ya diversos autores consideran un síndrome neurodermatológico. Sus características hacen que su diagnóstico y tratamiento puedan resultar complicados en la práctica clínica habitual, siendo necesarias herramientas sencillas que se puedan usar de rutina, tanto para identificar esta entidad, que puede presentarse acompañada de otra patología, como para su manejo independiente. En este trabajo realizamos una revisión práctica de los avances científicos más recientes el campo de la piel sensible que justifican su consideración individual y ofrecen herramientas para identificarla y tratarla. Proponemos algoritmos de diagnóstico y de tratamiento basados en las evidencias de la literatura y en la opinión de los expertos que firman este artículo.
Sensitive or reactive skin is a dermatological disorder that affects many people. The definition and terminology of this condition have varied over the years1 and, while the number of studies on the topic has increased progressively over the last decade, the syndrome continues to be difficult to define and diagnose.2,3 Moreover, sensitive skin has often been defined as a cosmetic condition or a purely psychosomatic disorder. As we shall see, however, the literature reviewed in this article indicates that sensitive skin has definite causes and is a real condition and an entity distinct from other skin diseases. We should, therefore, be aware of the need to identify and manage this condition and to improve the quality of life of those affected.
Our aim in this article is to provide a simple and practical algorithm for the diagnosis and treatment of sensitive skin syndrome based on expert opinion and the most recent updates on the topic in the literature.
Sensitive Skin: Definition, Classification, Epidemiology, and PathophysiologyEvolution of the Concept of Sensitive SkinIn 2011, a review by Escalas-Taberner et al.2 listed the main definitions of the term sensitive skin in the literature and described the condition as a complex syndrome with a high component of subjectivity on the part of the patient. In 2013, the explanation of the etiology of sensitive skin was expanded to include environmental factors.4,5
The authors of subsequent publications have noted the lack of consensus on the meaning of the term and the challenge presented by any effort to research this syndrome.6,7 The most recent definition—and the first to achieve consensus—was published in a position paper drawn up by a group of European experts at the International Forum for the Study of Itch in 2017.8 The group used the Delphi method to reach a very specific definition of sensitive skin as follows: “A syndrome defined by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations.These unpleasant sensations cannot be explained by lesions attributable to any skin disease. The skin can appear normal or be accompanied by erythema. Sensitive skin can affect all body locations, especially the face”.
Moreover, it has been considered necessary to distinguish between sensitive skin syndrome and selective sensitivities to specific products. This led to a proposed amendment to the terminology (Misery, 2017 #202), with the suggested new term being reactive skin. Although this new term is more accurate if we take into account what is known about the etiology and pathogenesis of the condition, the use of the term sensitive skin is still more widespread.
Sensitive Skin TypesSeveral studies have posited a connection between sensitive skin and a disruption of epidermal barrier function, which is thought to give rise to a feeling of discomfort in the skin (Draelos, 1997; Effendy, 1995; Goffin, 1996; Roussaki-Schulze, 2005; Saint-Martory, 2008). In terms of epidermal barrier function, sensitive skin can be classified into 3 types9:
- 1.
Type I: low barrier function
- 2.
Type II: normal barrier function with inflammatory changes
- 3.
Type III: normal barrier function without inflammation but with reactivity problems
In all 3 groups, it has been observed that concentrations of nerve growth factor in the epidermis are higher than the levels observed in non-sensitive skin. Furthermore, in both type II and type IIIpatients, sensitivity to electrical stimuli is high.
In terms of the factors that cause a reaction in sensitive skin, the condition can be classified as follows10:
- 1.
High sensitivity: reactive to a wide variety of both endogenous and exogenous factors and associated with acute or chronic symptoms and a strong psychological component
- 2.
Environmental sensitivity: fair, dry, and fine skin that has a tendency to blush and is reactive to primary environmental factors
- 3.
Cosmetic sensitivity: skin that exhibits transient reactivity to specific cosmetic products.
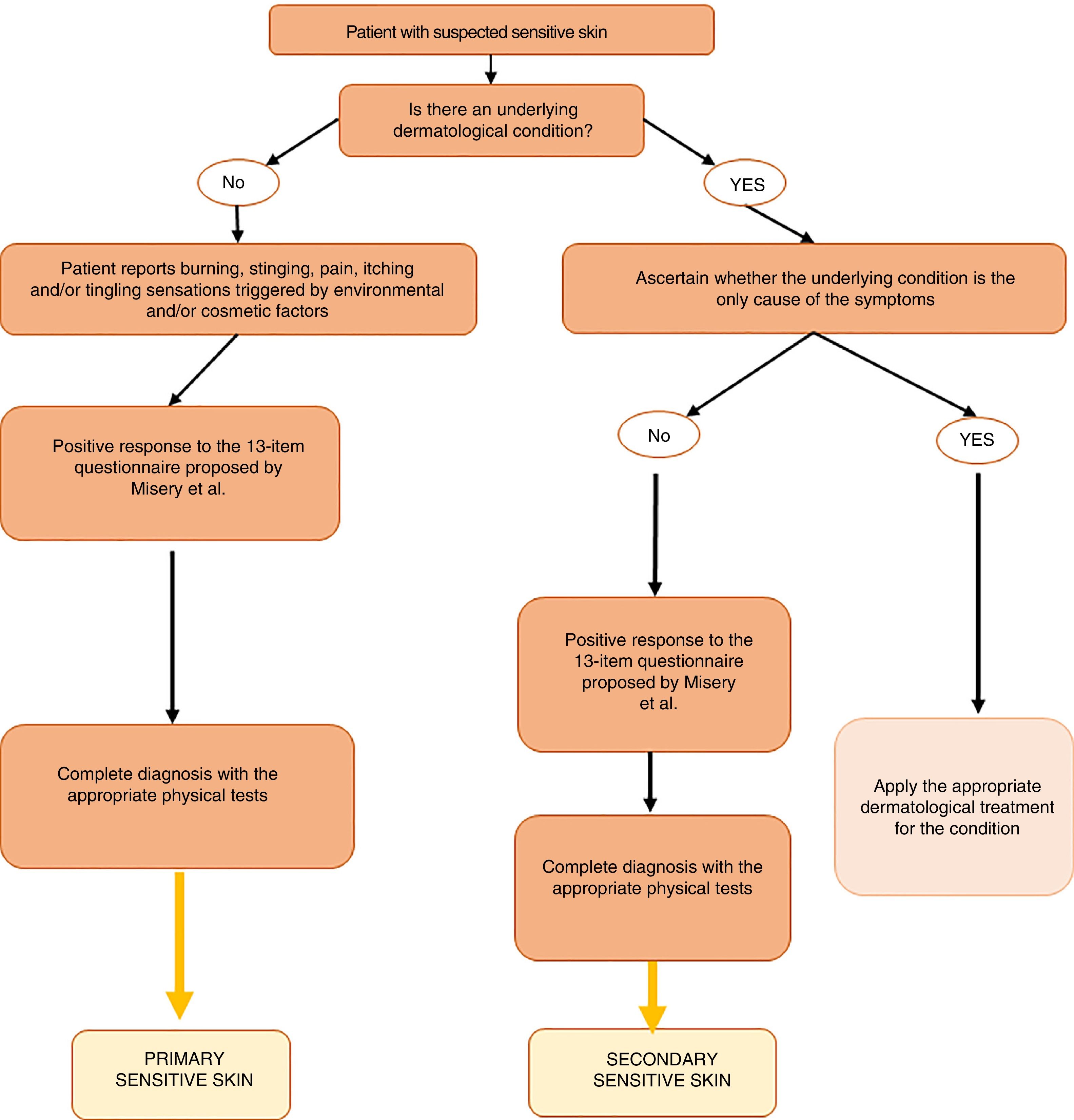
Finally, we propose a classification of the syndrome according to the presence or absence of associated skin diseases.
- 1.
Primary sensitive skin, in which the affected person has no associated underlying disease.
- 2.
Secondary sensitive skin, in which the patient has a skin condition, such as seborrheic, atopic, or contact dermatitis, rosacea, or acne.
The prevalence of sensitive skin syndrome in Europe is high, approximately 39%, and the condition appears to affect women more than men.11 The only reference to the prevalence of sensitive skin in Spain comes from a study published by Misery et al. in 2009.11 In that study, data were collected by telephone and through on-line surveys of representative samples of people aged 15 years or older in various European countries. The findings indicate that 11.6 million people in Spain could be affected by sensitive skin syndrome.
The data collected also showed a higher prevalence of the syndrome in women and no correlation with factors such as age, rural or urban setting, and socioprofessional category. Although these data provide an initial insight into the epidemiology of sensitive skin in Spain, further studies based on clinical diagnosis are needed to provide more consistent information on the prevalence of this syndrome.
Pathophysiology of Sensitive SkinThe mechanisms underlying sensitive skin syndrome continue to be studied and debated in the literature. Current evidence indicates that individuals with sensitive skin have one of the following cutaneous alterations: increased nerve fiber density, increased immune response, or low epidermal barrier function. All of these alterations contribute to the activation of a response to several factors. These factors may be environmental (pollution, radiation, UV exposure, weather), lifestyle-related (diet, use of cosmetics, alcohol consumption), or endogenous (psychological factors and emotional stress). In the following section, we will discuss the biological mechanisms activated by these different factors.
Neurosensorial MechanismsThere are several mechanisms through which the cutaneous nervous system may contribute to sensitive skin syndrome. One mechanism that could contribute to the condition is hyperreactivity of the cutaneous nerve endings. A lower density of intraepidermal nerve fibers, especially those of the peptidergic amyelinic C-fiber type, has been reported in patients with sensitive skin.12 This alteration would help to explain the neurogenic inflammation some people experience,12 irrespective of the presence of barrier function alterations. Transient receptor potential [TRP) channels expressed on the membrane of group C nerve fibers would appear to play a central role.13 While the evidence remains inconclusive, it appears likely that TRP channels play a central role in the perception and pathophysiology of sensitive skin as they can be activated by the many stimuli—physical, chemical, and thermal—that trigger sensitive skin.14–16 Vanilloid receptor 1 (TRPV1) appears to play a particularly important role, since it mediates the response to many of these factors.16–20
Immune Response MechanismsThe activation of TRPV1 channels in reactive skin triggers the cutaneous release of substance P and other neuropeptides and subsequently the release of proinflammatory cytokines, such as interleukin (IL) 2, tumor necrosis factor α, interferon γ, IL-23, and IL-31. This, in turn, enhances the immune response by recruiting more immune cells to the skin.6 All of these factors are related to the itching and burning sensations characteristic of sensitive skin syndrome.
Mechanisms Related to Altered Epidermal Barrier FunctionThe integrity of the epidermal barrier is essential to the maintenance of the skin's structure and functions. Disruption of this barrier, resulting in a thinner and more permeable stratum corneum,10,13,21 has been proposed as a trigger mechanism for the symptoms associated with sensitive skin. A weak epidermal barrier facilitates the penetration of irritants and allergens10 and is associated with poor protection of nerve endings and increased transepidermal water loss.22,23 The integrity of the epidermal barrier is highly dependent on lipid composition. In fact, it is known that sensitive skin results in changes in levels of neutral lipids, sphingolipids, and ceramides.24,25
Today, it is also known that barrier function also depends largely on the community of microorganisms that inhabit the skin, known as the skin microbiome. While sensitive skin, unlike dermatitis, is not associated with any imbalance or dysbiosis,6 the microbiome is a new field of study and numerous questions remain unanswered.
Practical Recommendations for the Diagnosis of Sensitive SkinThe diagnosis and treatment of sensitive skin is hindered by the lack of consensus in its definition noted by many authors. The following are a series of practical recommendations which, together with the algorithm proposed in Fig. 1, have been drawn up to serve as a guide for use in clinical practice.
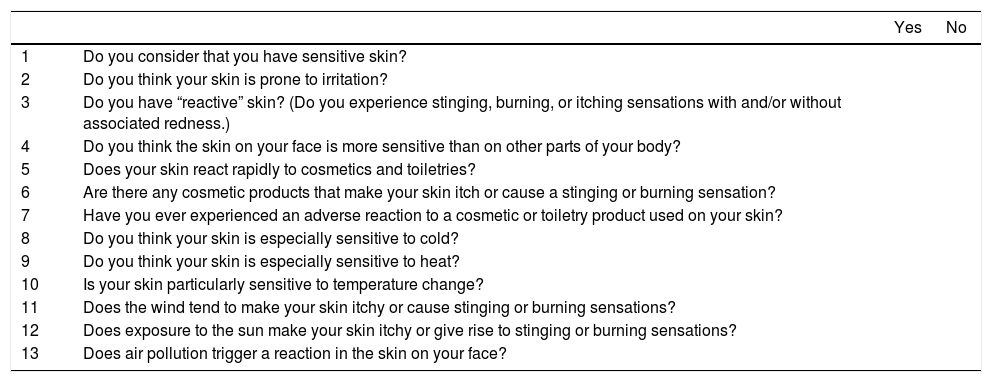
Targeted Medical History: The Use of QuestionnairesAs sensitive skin is a condition with a highly subjective component, diagnosis must be based, fundamentally, on the interpretation of the symptoms reported by the patient and an assessment of the patient's medical history (personal and family), daily habits, and use of cosmetics. Among other aspects, it is important to manage the symptoms reported and investigate other possible causes. Since these patients often do not present any objective physical signs of disease, questionnaires are a useful diagnostic tool in this setting.26
Table 1 lists a series of questions that will help the specialist to reach a correct diagnosis of sensitive skin syndrome. This set of questions can be divided into 3 blocks: the patient's own perception of the sensitivity, irritation, and reactivity of their skin (block I, questions 1-4), the skin's reaction to cosmetic products (block II, questions 5-7), and to environmental factors (block III, questions 8-13). The patient who gives a positive answer to at least 2 questions from block I, 3 questions from block II, or 3 questions from block III is considered to have sensitive skin.
Questionnaire for the Diagnosis of Sensitive Skin.
| Yes | No | ||
|---|---|---|---|
| 1 | Do you consider that you have sensitive skin? | ||
| 2 | Do you think your skin is prone to irritation? | ||
| 3 | Do you have “reactive” skin? (Do you experience stinging, burning, or itching sensations with and/or without associated redness.) | ||
| 4 | Do you think the skin on your face is more sensitive than on other parts of your body? | ||
| 5 | Does your skin react rapidly to cosmetics and toiletries? | ||
| 6 | Are there any cosmetic products that make your skin itch or cause a stinging or burning sensation? | ||
| 7 | Have you ever experienced an adverse reaction to a cosmetic or toiletry product used on your skin? | ||
| 8 | Do you think your skin is especially sensitive to cold? | ||
| 9 | Do you think your skin is especially sensitive to heat? | ||
| 10 | Is your skin particularly sensitive to temperature change? | ||
| 11 | Does the wind tend to make your skin itchy or cause stinging or burning sensations? | ||
| 12 | Does exposure to the sun make your skin itchy or give rise to stinging or burning sensations? | ||
| 13 | Does air pollution trigger a reaction in the skin on your face? |
Block I: questions 1-4; Block II: questions 5-7; Block III: questions 8-13.
In addition to the questionnaire proposed in Table 1, we also recommend the use of the 10-item questionnaire validated by Misery et al.27 On that scale, a score between 20 and 60 points (or more) identifies individuals with sensitive skin.
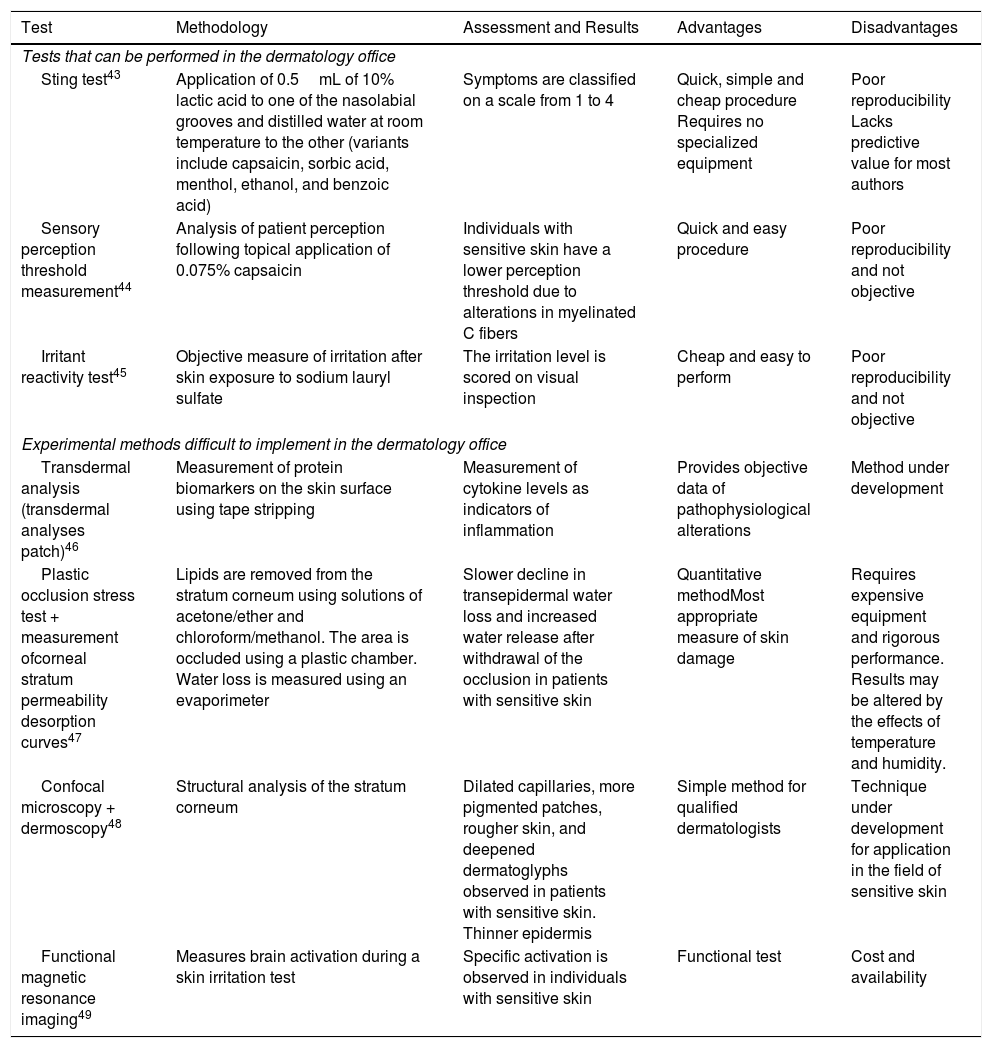
Diagnostic TestsAlthough, as indicated above, questionnaires are still the most reliable method for diagnosing sensitive skin, the results of a number of physical tests can help the specialist make a correct diagnosis. A list of these tests, together with their advantages and disadvantages, is shown in Table 2.
Diagnostic Tests Described in the Literature for the Identification of Sensitive Skin.
| Test | Methodology | Assessment and Results | Advantages | Disadvantages |
|---|---|---|---|---|
| Tests that can be performed in the dermatology office | ||||
| Sting test43 | Application of 0.5mL of 10% lactic acid to one of the nasolabial grooves and distilled water at room temperature to the other (variants include capsaicin, sorbic acid, menthol, ethanol, and benzoic acid) | Symptoms are classified on a scale from 1 to 4 | Quick, simple and cheap procedure Requires no specialized equipment | Poor reproducibility Lacks predictive value for most authors |
| Sensory perception threshold measurement44 | Analysis of patient perception following topical application of 0.075% capsaicin | Individuals with sensitive skin have a lower perception threshold due to alterations in myelinated C fibers | Quick and easy procedure | Poor reproducibility and not objective |
| Irritant reactivity test45 | Objective measure of irritation after skin exposure to sodium lauryl sulfate | The irritation level is scored on visual inspection | Cheap and easy to perform | Poor reproducibility and not objective |
| Experimental methods difficult to implement in the dermatology office | ||||
| Transdermal analysis (transdermal analyses patch)46 | Measurement of protein biomarkers on the skin surface using tape stripping | Measurement of cytokine levels as indicators of inflammation | Provides objective data of pathophysiological alterations | Method under development |
| Plastic occlusion stress test + measurement ofcorneal stratum permeability desorption curves47 | Lipids are removed from the stratum corneum using solutions of acetone/ether and chloroform/methanol. The area is occluded using a plastic chamber. Water loss is measured using an evaporimeter | Slower decline in transepidermal water loss and increased water release after withdrawal of the occlusion in patients with sensitive skin | Quantitative methodMost appropriate measure of skin damage | Requires expensive equipment and rigorous performance. Results may be altered by the effects of temperature and humidity. |
| Confocal microscopy + dermoscopy48 | Structural analysis of the stratum corneum | Dilated capillaries, more pigmented patches, rougher skin, and deepened dermatoglyphs observed in patients with sensitive skin. Thinner epidermis | Simple method for qualified dermatologists | Technique under development for application in the field of sensitive skin |
| Functional magnetic resonance imaging49 | Measures brain activation during a skin irritation test | Specific activation is observed in individuals with sensitive skin | Functional test | Cost and availability |
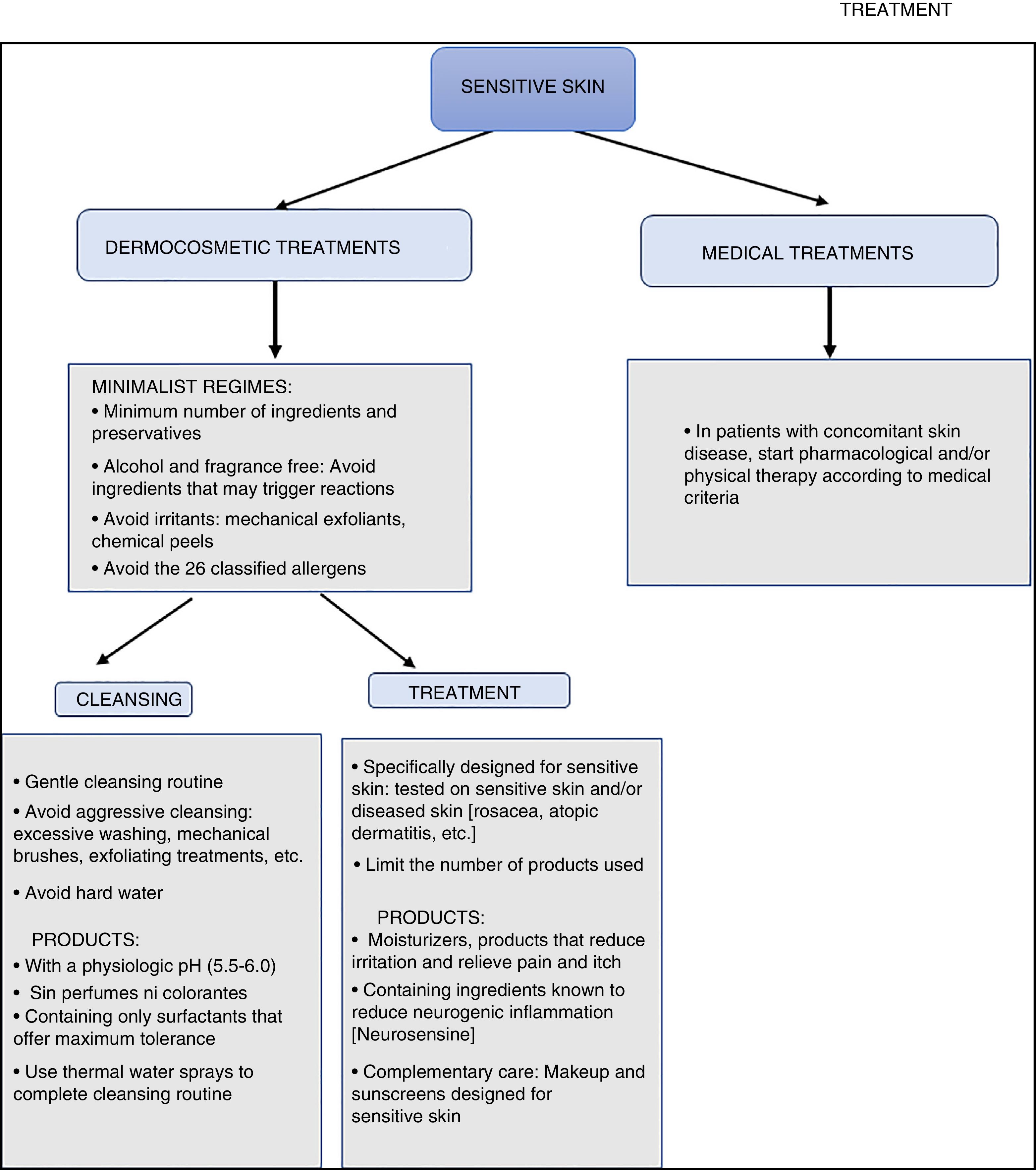
The care and treatment of sensitive skin remains challenging and requires the use of gentle topical products containing non-irritating ingredients.28 Based on the evidence we have reviewed, it would appear that these products should fulfil the following 3 criteria:
- 1.
Restore barrier function. Repairing weakened barrier function should increase the tolerance threshold and restore the protection provided by the epidermal barrier against all types of insults: physical, chemical, mechanical, immunological, and microbiological.
- 2.
Reduce reactivity.Blocking inflammatory mediators and sensory neuropeptides will help to alleviate the symptoms associated with sensitive skin.
- 3.
Be safe for sensitive skin. The use of formulas with few ingredients is recommended in products designed for the care and treatment of sensitive skin. To obviate the need for preservatives, it will be necessary to design containers that preserve and protect the product, preventing contamination or degradation that could lead to chemical mediators or unwanted characteristics (for example a change in pH) that could aggravate the symptoms or destroy active ingredients beneficial to sensitive skin.
Appropriate cleaning and treatment regimens are essential for the care of sensitive skin because the use of inappropriate products could exacerbate symptoms. It is therefore important for these patients to use products with a pH in the physiological range (5.5-6.0) and avoid products that have a high pH or contain harsh surfactants that could damage the skin or mucous membranes. Skin cleansers should be fragrance-free and contain only mild amphoteric or anionic surfactants. Appropriate products may also contain hydrating elements of proven biocompatibility, such as glycerin, hyaluronic acid, in addition to relipidization components, such as vegetable oils or ceramides. Patients with sensitive skin should use a gentle cleansing routine, avoid scrubbing the skin with mechanical devices or exfoliating products. It is recommended that they should dry drying their skin by gently dabbing it with paper tissues (never cotton pads).10
These patients should use cosmetic products that have been shown to improve skin barrier function, with minimal concentrations of preservatives and no surfactants.29 Some authors recommend the use of products with simple formulas containing very few ingredients to avoid as far as possible common sensitizing agents, sensory stimulants, and cutaneous vasodilators and to minimize the content of irritants, such as benzoic acid, cinnamic acid, sodium lauryl sulfate, bronopol, lactic acid, propylene glycol, urea, and sorbic acid.10,30–32
It is also recommended that these patients should maintain their skin highly hydrated to reduce their susceptibility to irritation and to restore the integrity of the stratum corneum.33 Their regimen should include passive moisturizers (vegetable oils, silicones) to reduce transepidermal water loss and balance the skin's acid mantle, active moisturizing or hydrating products that retain water in the stratum corneum (glycerol, hyaluronic acid, filaggrin derivatives, all natural moisturizing factors), and finally relipidizing agents (vegetable oils, ceramides, and pseudoceramides).25,34,35 The formulation of the products used is also important: products containing active ingredients that are non-occlusive and favor a lightweight texture will facilitate the application of the product, reducing the need to rub or massage the skin.36,37
TreatmentCertain substances can be used to relieve the symptoms of sensitive skin. For instance, the efficacy of TRPV1 antagonists has been demonstrated.38 Specifically, pimecrolimus, a calcineurin inhibitor that acts on TRPV1, was shown to improve the symptoms of sensitive skin in a study of Chinese women.39 Efficacy has also been achieved with neurosensine, a molecule derived from a neurosensorial dipeptide naturally present in the skin. Neurosensine stimulates the production of endorphins and enkephalins in keratinocytes and contributes to the creation of a barrier that protects group C nerve fibers, thereby reducing stimulation of the nociceptive signaling pathways, including the TRPV1 and proinflammatory mediators (substance P). In a clinical study, a product containing neurosensine inhibited neurogenic inflammation, helping to reduce the most specific symptoms of sensitive skin, including burning, heat, itching, and stinging sensations.40
Another active ingredient of interest for the treatment of sensitive skin is nicotinamide, which helps to restore barrier function by increasing the synthesis of epidermal lipids and ceramides. This improvement in barrier function helps to reduce water loss. Nicotinamide also reduces the release of proinflammatory mediators and regulates the release of histamine, thereby reducing inflammation and itching. It has also been observed to have probiotic properties.41,42
Algorithm for the Diagnosis and Treatment of Sensitive SkinAs mentioned above, the diagnosis and treatment of sensitive skin in routine clinical practice continues to present a complex challenge. To address this problem, we propose simple algorithms based on current scientific evidence, the recommendations made in the present review, and the expert opinion of the authors of this article (Figs. 1 and 2). The aim of these algorithms is to facilitate the diagnosis of sensitive skin syndrome and offer practical guidelines for the treatment and care of the condition.
ConclusionsSensitive skin affects millions of people worldwide, causing numerous disagreeable sensations that have a negative impact on quality of life. These symptoms may lead those affected to consult a dermatologist. As dermatologists, we must be aware that sensitive skin is a syndrome, a concept validated by the evidence relating to its etiology and pathogenesis. We now have adequate tools to properly identify the syndrome and we can offer these patients recommendations on the most appropriate skin cleansing and care regimen.
Modern dermocosmetic brands are developing products that go beyond hydration and the reduction of certain skin components and are now incorporating ingredients capable of improving barrier function, decreasing neurogenic inflammation and sensory reactivity, while maintaining safety and tolerability.
An algorithm for the diagnosis and treatment of sensitive skin, such as the one presented here, can be an important aid for dermatologists and greatly benefit their patients.
FundingL‘Oréal financed the work undertaken by Medical Statistics Consulting SL to support the writing of this article and facilitated author meetings.
Conflicts of InterestLeonor Prieto is an employee of L’Oréal España-División Cosmética Activa.
The authors would like to thank Almudena Fuster and Blanca Piedrafita of Medical Statistics Consulting S.L. (Valencia, Spain) for their collaboration in the preparation of this article.
Please cite this article as: Guerra-Tapia A, Serra-Baldrich E, Prieto Cabezas L, González-Guerra E, López-Estebaranz JL. Diagnóstico y tratamiento del síndrome de piel sensible: un algoritmo para la práctica clínica habitual. Actas Dermo-Sifiliográficas. 2019;110:800–808.