Doxycycline is a synthetic tetracycline that was approved in 1967. This wide-spectrum antibiotic has been shown to also have useful anti-inflammatory properties that make it suitable for the treatment of a number of noninfectious conditions. Tetracyclines are probably the most commonly prescribed antibiotics in dermatology, where they are usually used at doses lower than those effective against infections. They also have an excellent efficacy and safety profile. Because of doxycycline’s ability to inhibit the molecular pathways associated with certain processes, this antibiotic can be used to treat hair follicle diseases, granulomatous diseases, and vascular proliferation, among other conditions. The main properties of doxycycline and its many applications in dermatology make this drug one that specialists should become familiar with.
La doxiciclina es una tetraciclina sintética aprobada por primera vez en 1967. Además de las propiedades antibacterianas de amplio espectro que posee esta molécula, se han ido descubriendo propiedades antiinflamatorias interesantes que le han ofrecido la oportunidad de ser una opción terapéutica en múltiples enfermedades no infecciosas. En el campo de la dermatología, las tetraciclinas son probablemente el antibiótico oral más frecuentemente prescrito, con dosis habitualmente inferiores a las indicadas para procesos infecciosos, con un perfil de eficacia y seguridad óptimo. Enfermedades relacionadas con la unidad foliculosebácea, procesos granulomatosos y proliferaciones vasculares, entre otros, pueden ser tratadas con doxiciclina gracias a la inhibición de vías moleculares relacionadas con estos procesos. Las principales características de la doxiciclina, y su amplio uso en dermatología, obligan al dermatólogo a estar familiarizado con este fármaco.
Benjamin Duggar, an American plant physiologist and mycologist, discovered chlortetracycline by examining a natural product obtained through the process of fermentation of the bacterium Streptomyces aureofaciens.1 The first tetracycline was developed in 1953, and the antimicrobial properties of this family ushered in a new chapter in the antibiotic era. Subsequent structural modification of these compounds gave rise to 2 synthetic tetracyclines: doxycycline (in 1967) and minocycline (in 1972). In addition to their antimicrobial properties, these compounds exhibited anti-inflammatory properties and became widely used in several specialties, including the field of dermatology, in which they are among the most commonly prescribed oral antibiotics.
Chemical propertiesTetracyclines contain a naphthalene ring consisting of 4 atoms with a tetracyclic nucleus, which is chemically derived from polycyclic naphthalene carboxamide and after which this group of antibiotics is named. The amphoteric behavior of the molecule allows it to form salts with both acids and bases. Tetracyclines are capable of chelating divalent or trivalent metals such as calcium, manganese, and magnesium.
Synthetic modification of tetracycline, which produces doxycycline and minocycline, has enhanced the biological functionality of these molecules, retaining the antimicrobial properties of the dimethylamino group and increasing lipophilic capacity. This results in better tissue penetration and higher drug concentrations in multiple organs, including the skin. The fact that tetracyclines can act as ionophores (bound to ferrous iron or calcium) confers these compounds intracellular activity, including effects on cell division.
PharmacokineticsDoxycycline2 absorption in the duodenum can reach 95%. The proportion of the drug bound to proteins is in the range of 82–93%. Its half-life is 12–25 h, and it is primarily distributed in excretory organs such as the liver, kidney, and digestive tract. After passage through these organs no secondary metabolites appear to be produced. Excretion occurs mainly via urine (33–60%) and feces (40–65%).
Nonantibiotic properties of doxycyclineMatrix metalloproteinasesMetalloproteinases (MMPs) participate in multiple biological processes via zinc-dependent multidomain endopeptidases. MMPs are not detected in the skin under normal conditions, but their presence increases considerably in inflammatory and oncological processes.
Doxycycline can inhibit MMP-2, MMP-3, MMP-8, MMP-9, and MMP-13. Breast cancer cell cultures express MMP-2, also known as gelatinase A, which is implicated in cell division and is noncompetitively inhibited by doxycycline.3 Doxycycline also inhibits MMP-3 synthesis in fibroblasts, neurons, and endothelial cells.4 These observations suggest that doxycycline could be used to treat some diseases that cause pruritus or dermal fibrosis. MMP-8 (or neutrophil collagenase) is also inhibited by doxycycline, especially in endothelial cells and in patients with periodontitis.5 MMP-9 participates in the degradation of basement membrane components, promoting the migration of immune cells through the basement membrane during inflammatory processes. Doxycycline has been shown to reduce MMP-9 synthesis in vitro.6
Protease activated receptor 2Protease activated receptor 2 (PAR2) is expressed in epidermal basal keratinocytes and in inflammatory cells, stimulating the synthesis of interleukin (IL) 1β and tumor necrosis factor α (TNF-α). It is activated by endogenous and exogenous serine proteases (e.g. bacterial products, allergens). A role of PAR2 in keratinocytic differentiation, skin hydration, neurogenic inflammation, and the sensation of pruritus has recently been described. PAR2 stimulation results in a loss of permeability of the skin barrier. Doxycycline inhibits PAR2 activation in vitro through the action of SLIGKV-NH(2).7 Other studies have demonstrated doxycycline -mediated inhibition of trypsin-like serine protease in the skin through the inhibition of kallikrein 5, which is also involved in skin inflammation.
Leukocyte chemotaxis and inflammatory cytokinesDoxycycline can inhibit MCP-1, thereby decreasing neutrophil migration in the pulmonary and aortic epithelium.8 It exerts a synergistic effect by decreasing levels of IL-8, which in turn participates in neutrophil chemotaxis in the epidermis.
Doxycycline decreases levels of TNF-α, IL-1β, IL-6, and IL-8 by suppressing activation of the NF-kB pathway and of TNF-α converting enzyme (TACE).9
Nitric oxide synthaseIn models of osteoarthritis, doxycycline inhibits nitric oxide synthase (NOS) through destabilization of the enzyme and post-transcriptional modification of inducible NOS, the degradation of which is consequently increased.
Other treatmentsIn vitro studies have shown that doxycycline lowers immunoglobulin E (IgE) levels in asthmatic patients. In mice with induced allergic conjunctivitis, doxycycline decreased IgE release and reduced histamine release by mast cells by modulating the phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) pathway.10 Moreover, in mice with induced periodontitis, doxycycline can eliminate free radicals and reduce oxidative stress by protecting against peroxynitrite-dependent inactivation of alpha1-antiproteinase.11 In other in vitro models doxycycline can inhibit protein kinase C, which is a key participant in granuloma formation. Phospholipase A2, which plays a central role in inflammatory processes through the release of arachidonic acid and the production of eicosanoids, is also inhibited by doxycycline.
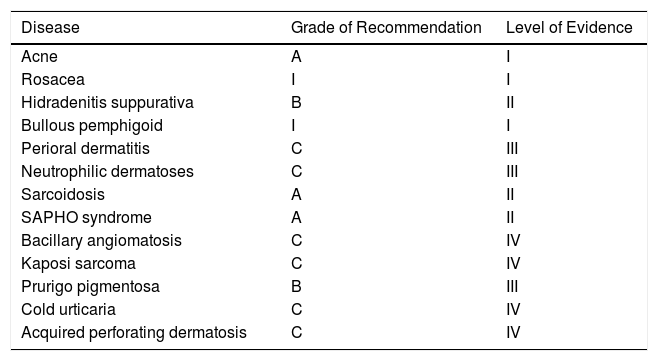
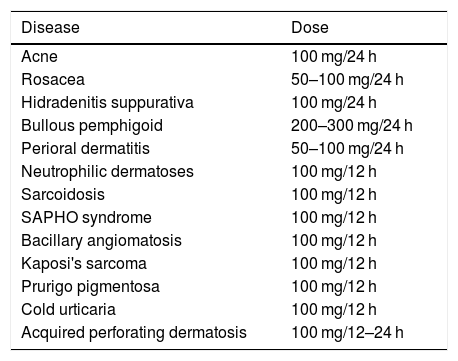
Indications for doxycycline in dermatologyTable 1 shows the main dermatological diseases in which doxycycline shows demonstrated efficacy. Table 2 shows the recommended dosage for each of the diseases described.
Main Indications of Doxycycline in Dermatology According to Grade of Recommendation and Level of Evidence.
| Disease | Grade of Recommendation | Level of Evidence |
|---|---|---|
| Acne | A | I |
| Rosacea | I | I |
| Hidradenitis suppurativa | B | II |
| Bullous pemphigoid | I | I |
| Perioral dermatitis | C | III |
| Neutrophilic dermatoses | C | III |
| Sarcoidosis | A | II |
| SAPHO syndrome | A | II |
| Bacillary angiomatosis | C | IV |
| Kaposi sarcoma | C | IV |
| Prurigo pigmentosa | B | III |
| Cold urticaria | C | IV |
| Acquired perforating dermatosis | C | IV |
Main Indications of Doxycycline in Dermatology and Recommended Doses.
| Disease | Dose |
|---|---|
| Acne | 100 mg/24 h |
| Rosacea | 50–100 mg/24 h |
| Hidradenitis suppurativa | 100 mg/24 h |
| Bullous pemphigoid | 200–300 mg/24 h |
| Perioral dermatitis | 50–100 mg/24 h |
| Neutrophilic dermatoses | 100 mg/12 h |
| Sarcoidosis | 100 mg/12 h |
| SAPHO syndrome | 100 mg/12 h |
| Bacillary angiomatosis | 100 mg/12 h |
| Kaposi's sarcoma | 100 mg/12 h |
| Prurigo pigmentosa | 100 mg/12 h |
| Cold urticaria | 100 mg/12 h |
| Acquired perforating dermatosis | 100 mg/12–24 h |
Abbreviation: SAPHO, synovitis, acne, pustulosis, hyperostosis, and osteitis.
Doxycycline is used to treat both acne (100 mg/24 h)12 and rosacea (50 and 100 mg/24 h).13 According to the most recent guidelines treatment cycles should be limited to between 3 and 6 months. This use is included in the summary of product characteristics for doxycycline, and supported by level Ia evidence. Doxycycline is also useful for the treatment of acneiform eruptions.
Hidradenitis suppurativaCombination antibiotic therapy is typically prescribed to ensure remission of moderate-to-severe hidradenitis.14 Tetracyclines are most often used for secondary prophylaxis to prevent relapse. Treatment with doses of 100 mg/24 h is supported by level IIb evidence,15 although this use is not included in the summary of product characteristics.
Autoimmune blistering diseases. Bullous pemphigoidDoxycycline is used to treat patients with bullous pemphigoid, often in combination with nicotinamide, which acts at distinct points within the inflammatory cascade. Doxycycline is usually administered when corticosteroids are contraindicated or not tolerated by the patient. Treatment at doses of 200–300 mg/24 h is supported by level 1a evidence.16 This use is not included in the summary of product characteristics.
Perioral dermatitisDoxycycline has been used at initial doses of 100 mg/24 h during the first weeks, subsequently reducing the dose to 50 mg/24 h.17 Some authors argue that a dose of 40–50 mg/d is sufficient given the lack of bacterial involvement in the pathogenesis of perioral dermatitis.18 This use is support by level IIIc evidence and is not included in the summary of product characteristics.
Neutrophilic diseases: sweet syndrome and folliculitis decalvansDoxycycline (200 mg/24 h) is used to treat this group of diseases owing to its immunomodulatory effects.19 It is a second-line treatment, supported by level IIIc evidence.20 In cases of folliculitis decalvans remission is usually less prolonged than that achieved using the combination of clindamycin and rifampicin. This use is not indicated in the summary of product characteristics.
Granulomatous diseases: sarcoidosis, granuloma due to dermal fillers, and granuloma annulareDoxycycline (200 mg/24 h) is also effective for the treatment of these conditions.21 It is especially useful in cases in which long-term treatment is required.22 It remains to be determined whether its efficacy is due to its antimicrobial action or its anti-inflammatory effect, although the available evidence appears to better support the latter hypothesis. It is used as a second-line drug, supported by level IIa evidence.23
Synovitis, acne, pustulosis, hyperostosis, and osteitis syndromeSynovitis, acne, pustulosis, hyperostosis, and osteitis syndrome (SAPHO) syndrome is a rare inflammatory disorder that affects the bones, joints, and skin. As in the case of isolated acne vulgaris, tetracyclines are the first-line treatment. Common regimens include doxycycline (100 mg twice per day) and minocycline (100 mg twice per day). Improvements in acne are observed from the first weeks of treatment and osteoarticular symptoms may also improve. This full dose is administered for 1–3 months, depending on the response, and is subsequently reduced to once per day in patients that respond to treatment.24 This use of doxycycline is supported by level IV evidence, and is not included in the summary of product characteristics.
Bacillary angiomatosisBacillary angiomatosis is a multisystemic infection that gives rise to a proliferative vascular disorder caused by Bartonella henselae and Bartonella quintana. It is mainly described in individuals with human immunodeficiency virus (HIV) infection and a CD4 count < 200 lymphocytes/mL. It can affect any organ, although the skin is most commonly affected.25 It manifests clinically as erythematous papules and nodules with scaling collarettes that bleed profusely in response to minimal trauma. Treatment consists of the administration of doxycycline (100 mg/12 h) for 8–12 weeks, after which the dose is reevaluated. This use of doxycycline is supported by level III evidence, and is indicated in the summary of product characteristics.
Kaposi sarcomaKaposi sarcoma is a vascular tumor of which 4 subtypes are described, one of which is associated with HIV infection. Human herpesvirus-8 (HHV-8) has been implicated in the etiology and pathogenesis of this entity. Inhibition of MMP metabolism appears to play an important role in its progression, and therefore doxycycline has been proposed as a possible therapeutic option. In their phase II trial of chemically modified tetracycline-3 (CMT-3) (inhibitor of secreted phospholipase A2 and some MMPs) Dezube et al. reported promising findings similar to those described for other conventional treatments.26 The use of doxycycline for this indication is supported by level IV evidence, and is not included in the summary of product characteristics.
Prurigo pigmentosaPrurigo pigmentosa is a rare entity described in Japan in 1971 and characterized clinically by the appearance of erythematous papules on the trunk and neck that coalesce to form plaques and patches with a reticulated, mottled appearance. Some cases involve blistering lesions that resolve over several weeks and leave marked residual hyperpigmentation. In many patients, prurigo pigmentosa is characterized by frequent flare ups. In the majority of published case series patients received a dose of 200 mg/24 h for 1–5 weeks, and achieved a good response.27–32 The use of doxycycline for this indication, which is not indicated in the summary of product characteristics, is supported by level IV evidence.
Cold urticariaChronic cold urticaria is a rare but serious, life-threatening form of inducible chronic urticaria, characterized by the development of wheals or angioedema after exposure of the skin to cold. The pathophysiology is unknown, although a role of histamine is fairly well established. According to Gorczyza,32 the therapeutic action of doxycycline may be explained by its effects on underlying chronic subclinical bacterial infections that cause and maintain the cold. However, there is little evidence in the literature to support a causative role of bacterial infections in cold urticaria. The effects of doxycycline may also be due to its immunoregulatory activity and its impact on cytokine production. Tetracyclines, and particularly doxycycline, suppress TNF-α, IL-1β, and IL-6, which are involved in different inflammatory skin disorders. Furthermore, doxycycline inhibits IgE-mediated degranulation and histamine-induced vascular permeability. The most consistent study published to date reported promising outcomes with a dose of 200 mg/d for 4 weeks, either in monotherapy or combined with a histamine H1 receptor antagonist. The use of doxycycline for this indication, which is not indicated in the summary of product characteristics, is supported by level IV evidence.
Acquired perforating dermatosisAcquired perforating dermatosis is a rare entity associated with other systemic diseases, in particular diabetes mellitus and/or renal failure. Its treatment poses a therapeutic challenge, and only 2 cases have been published to date, describing a moderate response to doxycycline (100 mg/12 h or 100 mg/24 h for 14–28 days).33,34 The use of doxycycline for this indication, which is not indicated in the summary of product characteristics, is supported by level IV evidence.
Oral aphthosisTopical doxycycline may be a therapeutic option for patients with oral aphthosis, given its combined antibiotic and anti-inflammatory properties. Doxycycline has been used to treat oral aphthosis either in crushed form or as a 0.15% hydrogel, applied until resolution of the ulcers (10–14 days). The use of doxycycline for this indication, which is not indicated in the summary of product characteristics, is supported by level I evidence.35
Pharmacological interactionsThe main pharmacological interactions of doxycycline are detailed below.
- -
Decrease absorption of doxycycline: antacids that contain aluminum, calcium, or magnesium.
- -
Decrease effect of doxycycline: co-administration with penicillin-derived bactericidal antibiotics.
- -
Increase nephrotoxic effects of doxycycline: methoxyflurane and diuretic drugs.
- -
Risk of benign intracranial hypertension: co-administration with systemic retinoids.
- -
Increased plasma concentration of lithium, digoxin, and theophylline.
- -
Increased metabolism of antiepileptics and rifampicin.
- -
Reduced effectiveness of oral contraceptives.
- -
Decreased warfarin metabolism.
Doxycycline is an oral antibiotic. It should ideally be taken during a meal, accompanied by a large glass of water. Dairy products decrease its absorption, and should be avoided. Most importantly, doxycycline should be taken at least 1 h before lying down or going to sleep in order to avoid gastroesophageal reflux and prevent the formation of ulcers in the upper digestive tract.
Precautions and contraindicationsUse of doxycycline is not recommended during tooth formation (i.e. during the 2nd half of pregnancy, during lactation, and in children under 8 years of age), as this can cause permanent discoloration of the teeth and delay bone development. According to the Food and Drug Administration, doxycycline is absolutely contraindicated in patients with lupus erythematosus and myasthenia gravis, and relatively contraindicated during pregnancy and lactation.
ConclusionsThe use of tetracyclines has evolved with the synthesis of molecules such as doxycycline. Doxycycline has become the most prescribed oral antibiotic in the field of dermatology, mainly owing to its anti-inflammatory properties. Given the broad spectrum of diseases that present with involvement of the folliculosebaceous unit, granulomatous processes, or vascular proliferations, doxycycline has a wide range of potential therapeutic applications. More studies are needed to support its use for the treatment of diseases other than acne, including those described in this article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
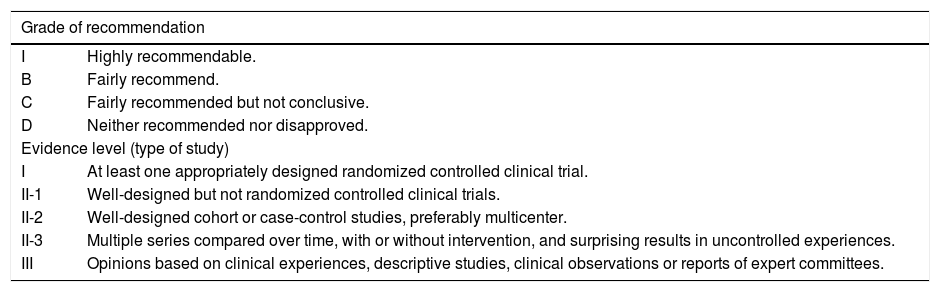
| Grade of recommendation | |
|---|---|
| I | Highly recommendable. |
| B | Fairly recommend. |
| C | Fairly recommended but not conclusive. |
| D | Neither recommended nor disapproved. |
| Evidence level (type of study) | |
| I | At least one appropriately designed randomized controlled clinical trial. |
| II-1 | Well-designed but not randomized controlled clinical trials. |
| II-2 | Well-designed cohort or case-control studies, preferably multicenter. |
| II-3 | Multiple series compared over time, with or without intervention, and surprising results in uncontrolled experiences. |
| III | Opinions based on clinical experiences, descriptive studies, clinical observations or reports of expert committees. |
Please cite this article as: Navarro-Triviño FJ, Pérez-López I, Ruíz-Villaverde R. Doxiciclina, ¿antibiótico o antiinflamatorio? Usos más frecuentes en dermatología. Actas Dermosifiliogr. 2020;111:561–566.