The influx of a large number of immigrants has altered the sociodemographic profile in Spain. To date, few studies of the skin diseases of immigrants to Spain have been done.
ObjectiveTo determine the frequency of visits by immigrants to our dermatology clinic, to describe their skin complaints, and to compare them to those of the autochthonous Spanish population.
Patients and methodsProspective, descriptive, analytic study, with an observational substudy of cases and controls from a cross-section of the population. We included all immigrant patients seen at the dermatology clinic between February 2005 and February 2006.
ResultsVisits by immigrants to the dermatology clinic accounted for 4.1% of the caseload. Their most frequent complaints were eczematous dermatitis (18.4%), viral warts (6.4%), and acne (6.3%). Comparison between the immigrant and autochthonous patient populations showed that eczematous dermatitis, alopecia, melasma, ringworm, scabies, Herpes simplex infection, keratosis pilaris, and xerosis were significantly more frequent among immigrant patients, whereas viral warts, actinic keratosis, hidradenitis suppurativa, lupus, melanoma, and squamous cell carcinoma were significantly less frequent (P<.05).
ConclusionsThe immigrant population consults the dermatologist about skin conditions that are already well represented in our routine practice. As the infectious skin diseases of immigrants are also common in our environment, these patients are unlikely to transmit serious tropical skin diseases to the local population.
España presenta una nueva realidad sociodemográfica condicionada por la llegada de gran número de personas inmigrantes. Debido a la escasez de estudios en nuestro país sobre población inmigrante (PI) en el campo de la Dermatología nos planteamos realizar este trabajo.
ObjetivoConocer la frecuencia de consultas de la PI de nuestro ámbito, documentar sus dermatosis y compararlas con las de la población autóctona (PA).
Pacientes y métodosEstudio prospectivo, descriptivo y analítico y subestudio observacional transversal de casos y controles. Se incluyó a todos los pacientes inmigrantes que fueron atendidos en la Sección de Dermatología entre febrero de 2005 y febrero de 2006.
ResultadosLa PI generó el 4,1% del total de consultas en Dermatología. Las patologías más frecuentes por las que consultaron fueron: dermatitis eccematosa (18,4%), verruga vírica (6,4%) y acné (6,3%). Al comparar las dermatosis entre PI y PA, la dermatitis eccematosa, la alopecia, el melasma, la tiña, la escabiosis, el herpes simple, la queratosis pilar y la xerosis fueron significativamente más frecuentes en la PI, mientras que los nevus melanocíticos, la verruga vírica, la queratosis actínica, la hidrosadenitis supurativa, el lupus, el melanoma y el carcinoma espinocelular lo fueron menos (p<0,05).
ConclusionesLas dermatosis por las que la población inmigrante suele consultar son las patologías habituales en nuestra práctica clínica diaria. Además sus dermatosis infecciosas son cosmopolitas, por lo que el paciente inmigrante probablemente no supone un riesgo real de transmisión de enfermedades importadas tropicales en el campo de la Dermatología.
The considerable inequality between countries as a result of wars and large percentages of some populations living below the poverty line has led to increases in migratory flows across borders. European countries have received large numbers of immigrants in recent years and Spain is no exception. As a result, the composition of our population has changed considerably with the arrival of immigrants from Africa, Asia, Latin America, and Eastern Europe.
The resulting sociodemographic changes call for a reanalysis of needs and priorities in all health care areas.1 Several studies have analyzed the sociodemographic characteristics and specific and general health care needs of the immigrant population in Spain.2,3
Few studies, however, have been conducted in dermatology,4 although there have been isolated reports of skin diseases in immigrant patients.5–7 A number of Spanish studies have also analyzed the peculiarities of skin disorders in dark-skinned individuals and shown that certain conditions are difficult to diagnose in these patients.8,9
In view of the growth of the immigrant population in Spain and the lack of studies on skin disorders in this population from the perspective of the health care system, we decided to analyze and compare the frequency of dermatology consultations and the prevalence of skin disorders in immigrant and nonimmigrant patients in Spain.
Patients and MethodsWe conducted a prospective, descriptive, and analytical study of immigrant patients treated at any of the dermatology units in health care district number 19 in Alicante, Spain between February 1, 2005 and February 1, 2006. We analyzed the frequency of and reasons for consultation in this group and also designed a cross-sectional substudy of skin complaints diagnosed in Spanish patients to compare the prevalence of skin disorders in immigrant and nonimmigrant patients.
For the purpose of this study, we considered an economic immigrant to be someone who had been born outside the European Union (EU-25) or in a country that had a lower per capita gross domestic product than Spain in January 2005. This excluded immigrants from the United States, Switzerland, Norway, Canada, Japan, Iceland, Kuwait, and Israel. We also included children of immigrants, even if they had been born in Spain, and adopted children if they had been in Spain for fewer than 6 years.
Data CollectionAll consultations made by immigrant patients at any of the dermatology units in the district under study between February 1, 2005 and February 1, 2006 were recorded prospectively. Each visit was considered to be a separate consultation. Data were collected by dermatologists or residents in training at the units.
To compare the prevalence of skin disorders in immigrants and nonimmigrants, we took a sample of Spanish patients treated on a given day each month for the duration of the study. All the visits made at any of the dermatology units in the health care district analyzed were recorded.
Main variable: prevalence of skin disordersThe skin disorders diagnosed were classified in accordance with the International Coding Index for Dermatology compatible with the ninth revision of the International Disease Classification.10 Each disorder was further classified into the following disease categories: infectious diseases, inflammatory diseases, tumors (benign and malignant), toxic skin reactions, mucosal disorders, nail disorders, pigmentation disorders, vascular disorders, hair disorders, and other.
Descriptive VariablesThe following data were collected for each of the patients studied:
- 1.
Epidemiological variables: age; sex; time in Spain; type of patient (adult immigrant, child immigrant, adopted child), skin type (white, black, Latin American, Asian Indian, Arab, or Asian oriental).
- 2.
Sociodemographic variables: profession and country of origin, subsequently classified into the following geographic regions: Latin America, North Africa, the Middle East, sub-Saharan Africa, Eastern Europe, and Asia.
- 3.
Care-related variables: unit where the patient was seen (dermatology clinic at a national health service outpatient facility, hospital outpatient visit, hospital bedside visit, emergency department, and surgery), type of visit (first visit or follow-up), and month in which the visit was made.
- 4.
Skin disorder variables: duration of disorder, tests ordered, type of treatment, type of prescription (corresponding to active worker, pensioner, or patient not entitled to reimbursement).
We determined the prevalence of skin disorders in the immigrant population by condition and the 10 disease categories described in the previous section.
We then compared the prevalence of disorders in the 2 populations and compared the distribution of disease categories between populations. To adjust for the fact that the mean age of the patients in the Spanish group was higher than that of the patients in the immigrant group, we limited our comparative analysis to consultations made by patients under 60 years of age. We also performed sex- and age-adjusted comparisons.
Statistical AnalysisQuantitative variables were expressed as means (SD) and qualitative variables as absolute and relative frequencies for the different variables analyzed. Qualitative variables were compared using the χ2 test with Yates correction or, where appropriate, the Fisher exact test. Quantitative variables were compared using analysis of variance or the nonparametric Kruskal–Wallis test for abnormally distributed data (heterogeneity of variance). The association between consultations made by immigrant and Spanish patients was measured by calculating odds ratios and their 95% CIs.
The association between skin disorders in immigrant and Spanish patients under 60 years of age was calculated using logistic regression with odds ratios and 95% CIs adjusted for age and sex. Statistical significance was set at a P value of less than .05, and all analyses were performed using the SPSS software package version 12.0 for Windows (SPSS Inc.).
ResultsEpidemiological Characteristics of Immigrant PatientsIn total, 39160 consultations were made between February 1, 2005 and February 1, 2006. Of these, 37535 (95.9%) were made by Spanish patients and 1625 (4.1%) were made by immigrant patients (n=1085), whose characteristics are summarized in Table 1.
Epidemiological Characteristics of Immigrant Patients.
| Age, y (n=1071) | |
| Mean (SD) | 29.07 (16.17) |
| Median (IQR) | 30 (17-40) |
| Age group (n=1071) | No. (%) |
| 0-14 y | 229 (21.4) |
| 15-29 y | 303 (28.3) |
| 30-44 y | 359 (33.5) |
| >44 y | 180 (16.8) |
| Sex (n=1081) | |
| Male | 459 (42.3) |
| Female | 626 (57.7) |
| Time in Spain, months (n=1071) | |
| Mean (SD) | 56.1 (56.3) |
| Median (IQR) | 48 (24–60) |
| Months in Spain (n=1071) | No. (%) |
| 0-24 | 289 (28.1) |
| 25-48 | 375 (36.5) |
| >48 | 364 (35.4) |
| Type of patient (n=1085) | No. (%) |
| Immigrant | 978 (90.1) |
| Child of immigrant | 100 (9.2) |
| Adopted child | 7 (0.6) |
| Skin type (n=1075) | No. (%) |
| Latin American | 459 (42.7) |
| White | 353 (32.8) |
| North African | 135 (12.6) |
| Black | 97 (9) |
| Asian oriental | 16 (1.5) |
| Asian Indian | 9 (0.8) |
| Mixed white-black | 6 (0.6) |
| Geographic area (n=1076) | No. (%) |
| Latin America | 706 (65.6) |
| North Africa and the Middle East | 157 (14.6) |
| Eastern Europe | 123 (11.4) |
| Sub-Saharan Africa | 64 (5.9) |
| Asia | 25 (2.3) |
Abbreviation: IQR, interquartile range.
A total of 1846 episodes were recorded during the 1625 visits made by immigrant patients during the study period; 1326 of the consultations were first visits. The most common diagnoses were eczema (18.4%), nongenital warts (6.4%), acne (6.3%), and melanocytic nevi (5.4%). Table 2 shows the frequency of the most common diagnoses in the immigrant population, the total number of follow-up visits per diagnosis, and the mean number of visits per diagnosis.
Skin Disorders Diagnosed on More Than 10 Occasions in the Immigrant Population.
| Skin Disorder | No. (%) of Diagnoses (n=1326) | No. of Follow-up Visits per Diagnosis | Mean (SD) No. of Visits per Diagnosis |
| Eczema | 244 (18.4) | 127 | 1.53 (1.07) |
| Nongenital warts | 85 (6.4) | 25 | 1.29 (.70) |
| Acne | 83 (6.3) | 41 | 1.49 (.89) |
| Melanocytic nevus | 71 (5.4) | 17 | 1.24 (.49) |
| Psoriasis | 45 (3.4) | 34 | 1.76 (1.15) |
| Soft fibroma | 45 (3.4) | 6 | 1.13±0.34 |
| Alopecia | 35 (2.6) | 9 | 1.29±0.62 |
| Epidermal cyst | 33 (2.5) | 14 | 1.42 (0.61) |
| Ingrown nail | 28 (2.1) | 16 | 1.57 (1.34) |
| Melasma | 27 (2) | 5 | 1.19 (0.48) |
| Molluscum contagiosum | 25 (1.9) | 13 | 1.52 (0.65) |
| Onychomycosis | 25 (1.9) | 12 | 1.48 (0.65) |
| Seborrheic keratosis | 25 (1.9) | 3 | 1.12 (0.64) |
| Scabies | 23 (1.7) | 6 | 1.22 (0.51) |
| Pruritus | 23 (1.7) | 13 | 1.57 (1.03) |
| Tinea | 22 (1.7) | 5 | 1.23 (0.52) |
| Angioma and other vascular abnormalities | 21 (1.6) | 8 | 1.33 (0.79) |
| Seborrheic dermatitis | 21 (1.6) | 1 | 1.05 (0.21) |
| Pityriasis versicolor | 18 (1.4) | 0 | 1 (0) |
| Urticaria | 18 (1.4) | 3 | 1.17 (0.38) |
| Vitiligo | 18 (1.4) | 14 | 1.75 (0.80) |
| Alopecia areata | 16 (1.2) | 12 | 1.75 (0.68) |
| Genital warts | 14 (1.1) | 17 | 2.21 (1.47) |
| Herpes simplex | 14 (1.1) | 3 | 1.14 (0.36) |
| Dermatofibroma | 13 (1) | 1 | 1.08 (0.27) |
| Postinflammatory hyperpigmentation | 13 (1) | 4 | 1.31 (0.63) |
| Acne rosacea | 12 (0.9) | 5 | 1.50 (0.79) |
| Scar | 12 (0.9) | 10 | 1.83 (2.03) |
| Keratosis pilaris | 12 (0.9) | 2 | 1.17 (0.57) |
| Callus | 11 (0.8) | 3 | 1.27 (0.64) |
| Folliculitis | 11 (0.8) | 7 | 1.55 (0.82) |
| Insect/arachnid bites | 11 (0.8) | 3 | 1.27 (0.46) |
| Xerosis | 11 (0.8) | 1 | 1.09 (0.30) |
Conditions that had been present for more than 3 years at the time of consultation generated the largest percentage of visits (25.5%).
The most common disease categories were inflammatory diseases (42.3%), benign tumors (19.8%), and infectious diseases (19.1%). Table 3 shows the frequency of the most common diagnostic categories in the immigrant population, as well as the total number of follow-up visits per category, and the mean number of visits per category.
Skin Disorders in Immigrant Patients by Category.
| Categorya | No. (%) of Diagnoses (n=1326) | No. of Follow-up Visits per Category | Mean (SD) No. of Visits per Category |
| Inflammatory disease | 561 (42.3) | 280 | 1.50 (0.98) |
| Benign tumor | 263 (19.8) | 76 | 1.29 (0.72) |
| Infectious disease | 253 (19.1) | 89 | 1.34 (0.71) |
| Pigmentation disorders | 79 (6) | 23 | 1.29 (0.60) |
| Hair disorders | 44 (3.3) | 10 | 1.23 (0.56) |
| Nail disorders | 36 (2.7) | 17 | 1.47 (1.20) |
| Other skin disorders | 29 (2.2) | 15 | 1.52 (1.09) |
| Malignant tumors | 18 (1.4) | 6 | 1.33 (0.59) |
| Vascular disorders | 8 (0.6) | 2 | 1.13 (0.35) |
| Toxic skin reactions | 6 (0.5) | 16 | 3.67 (4.36) |
| Mucosal disorders | 5 (0.4) | 1 | 1.20 (0.44) |
The following disorders were significantly more common (P<.05) in immigrant patients than in Spanish patients under 60 years of age: eczema, alopecia, melasma, tinea, scabies, herpes simplex infection, ingrown nails, keratosis pilaris, and xerosis. By contrast, melanocytic nevi, seborrheic keratosis, actinic keratosis, basal cell carcinoma, hidradenitis suppurativa, lupus, melanoma, and squamous cell carcinoma were significantly more common in Spanish patients (P<.05). There were no cases of melanoma or squamous cell carcinoma in the immigrant group.
Following adjustment for age and sex, nongenital warts proved more common in the Spanish patients, and the differences in prevalences of seborrheic keratosis, ingrown nails, and basal cell carcinoma were no longer statistically significance; otherwise, results were similar (Table 4).
Comparison of Skin Disorders Between Immigrant and Spanish Patients Younger Than 60 Years Old, Including Odds Ratio Adjusted for Age and Sex.
| Skin Disorder | Population <60 y | P Value | Adjusted OR | Adjusted P Value | |
| No. (%) of Immigrants (n=1267) | No. (%) of Spanish Patients (n=1107) | ||||
| Eczema | 239 (18.9) | 94 (8.5) | <.001 | 2.27 (1.76–2.94) | < .001 |
| Melanocytic nevus | 68 (5.4) | 144 (13) | <.001 | 0.35 (0.26–0.47) | < .001 |
| Nongenital warts | 82 (6.5) | 91 (8.2) | NS | 0.71 (0.52–0.97) | .035 |
| Acne | 82 (6.5) | 78 (7) | NS | 0.73 (0.52–1.01) | NS |
| Soft fibroma | 41 (3.2) | 48 (4.3) | NS | 0.92(0.59–1.43) | NS |
| Psoriasis | 41 (3.2) | 47 (4.2) | NS | 0.9 (0.58–1.41) | NS |
| Epidermal cyst | 33 (2.6) | 45 (4.1) | NS | 0.72 (0.45–1.15) | NS |
| Seborrheic keratosis | 19 (1.5) | 44 (4) | <.001 | 0.57 (0.32–1.01) | NS |
| Seborrheic dermatitis | 20 (1.6) | 29 (2.6) | NS | 0.62 (0.43–1.12) | NS |
| Alopecia | 35 (2.8) | 12 (1.1) | .005 | 2.8 (1.43–5.49) | .003 |
| Ingrown nail | 28 (2.2) | 17 (1.5) | .005 | 1.21 (0.65–2.24) | NS |
| Angioma and other vascular abnormalities | 19 (1.5) | 21 (1.9) | NS | 0.73 (0.38–1.37) | NS |
| Molluscum contagiosum | 25 (2) | 13 (1.2) | NS | 1.23 (0.61–2.45) | NS |
| Onychomycosis | 22 (1.7) | 14 (1.3) | NS | 1.94 (0.96–3.93) | NS |
| Pruritus | 22 (1.7) | 13 (1.2) | NS | 1.71 (0.84–3.48) | NS |
| Melasma | 27 (2.1) | 6 (0.5) | .002 | 4.7 (1.91–11.70) | .001 |
| Actinic keratosis | 4 (0.3) | 28 (2.5) | <.001 | 0.25 (0.08–0.75) | .013 |
| Alopecia areata | 15 (1.2) | 16 (1.4) | NS | 0.90 (0.43–1.85) | NS |
| Basal cell carcinoma | 6 (0.5) | 22 (2) | .001 | 0.47 (0.18–1.22) | NS |
| Pityriasis versicolor | 18 (1.4) | 8 (0.7) | NS | 1.95 (0.83–4.56) | NS |
| Dermatofibroma | 12 (0.9) | 13 (1.2) | NS | 0.87(0.39–1.95) | NS |
| Tinea | 21 (1.7) | 4 (0.4) | .004 | 5.16 (1.74 –15.3) | .003 |
| Scar | 12 (0.9) | 12 (1.1) | NS | 0.75 (0.33–1.71) | NS |
| Urticaria | 17 (1.3) | 6 (0.7) | NS | 1.79 (0.76–4.21) | NS |
| Vitiligo | 17 (1.3) | 6 (0.5) | NS | 2.42 (0.94–6.23) | NS |
| Genital warts | 14 (1.1) | 8 (0.7) | NS | 1.43 (0.59–3.47) | NS |
| Scabies | 22 (1.7) | 0 | <.001 | – | NA |
| Acne rosacea | 12 (0.9) | 9 (0.8) | NS | 1.41 (0.57–3.44) | NS |
| Androgenetic alopecia | 6 (0.5) | 12 (1.1) | NS | 0.4 (0.14–1.1) | NS |
| Lichen planus | 8 (0.6) | 9 (0.8) | NS | 0.83 (0.31–2.2) | NS |
| Postinflammatory hyperpigmentation | 13 (1) | 4 (0.4) | NS | 2.59 (0.83–8.08) | NS |
| Insect/arachnid bites | 11 (0.9) | 6 (0.5) | NS | 1.24 (0.45–3.42) | NS |
| Herpes simplex | 14 (1.1) | 2 (0.2) | .013 | 6.58 (1.47–29.45) | .014 |
| Age spots | 5 (0.4) | 11 (1) | NS | 0.67 (0.22–2.03) | NS |
| Folliculitis | 11 (0.9) | 4 (0.4) | NS | 2.7 (0.84–8.68) | NS |
| Nail dystrophy | 7 (0.6) | 8 (0.7) | NS | 0.83 (0.29–2.36) | NS |
| Callus | 10 (0.8) | 3 (0.3) | NS | 3.74 (0.99–14.04) | NS |
| Keratosis pilaris | 12 (0.9) | 1 (0.1) | .01 | 8.19 (1.05–63.51) | 0.04 |
| Melanoma | 0 | 13 (1.2) | .001 | – | NA |
| Hidradenitis suppurativa | 2 (0.2) | 10 (0.9) | .02 | 0.19 (0.04–0.91) | .03 |
| Lupus | 2 (0.2) | 10 (0.9) | .02 | 0.17 (0.038–0.81) | .02 |
| Xerosis | 11 (0.9) | 0 | .005 | – | NA |
| Hypopigmentation | 7 (0.6) | 2 (0.2) | NS | 3.03 (0.61–14.91) | NS |
| Lipoma | 3 (0.2) | 6 (0.5) | NS | 0.40 (0.1–1.66) | NS |
| Lichen sclerosus | 2 (0.2) | 6 (0.5) | NS | 0.28 (0.05–1.43) | NS |
| Toxic skin reactions | 5 (0.4) | 2 (0.2) | NS | 2.82 (0.52–15.21) | NS |
| Candidiasis | 4 (0.3) | 2 (0.2) | NS | 1.54 (0.27–8.61) | NS |
| Herpes zoster | 4 (0.3) | 2 (0.2) | NS | 2.09 (0.36–11.91) | NS |
| Skin ulcer | 4 (0.3) | 2 (0.2) | NS | 2.62 (0.45–15.27) | NS |
| Squamous cell carcinoma | 0 | 4 (0.4) | .047 | – | NA |
| Keratoacanthoma | 1 (0.1) | 0 | NS | – | NA |
Abbreviations: OR, odds ratio; NA, not applicable; NS, not significant.
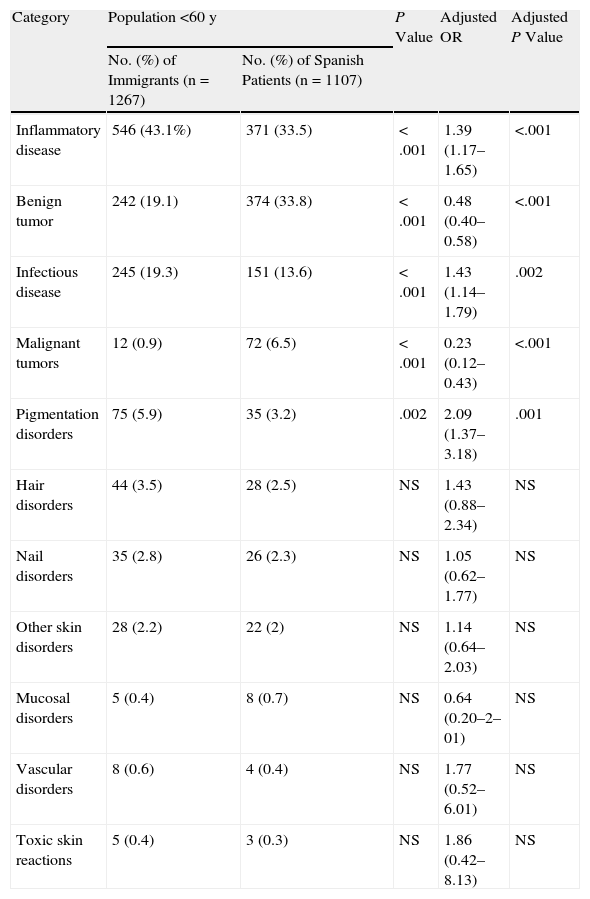
On comparing the groups by disease category, we found that inflammatory and infectious diseases and pigmentation disorders were significantly more common (P≤.002) in the immigrant group and that malignant and benign tumors were significantly less common (P<.001) (Table 5). Adjustment for age and sex did not change these results.
Comparison of Skin Disease Categories Between Immigrant and Spanish Patients Younger Than 60 Years Old, Including Odds Ratio Adjusted for Age and Sex.
| Category | Population <60 y | P Value | Adjusted OR | Adjusted P Value | |
| No. (%) of Immigrants (n=1267) | No. (%) of Spanish Patients (n=1107) | ||||
| Inflammatory disease | 546 (43.1%) | 371 (33.5) | <.001 | 1.39 (1.17–1.65) | <.001 |
| Benign tumor | 242 (19.1) | 374 (33.8) | <.001 | 0.48 (0.40–0.58) | <.001 |
| Infectious disease | 245 (19.3) | 151 (13.6) | <.001 | 1.43 (1.14–1.79) | .002 |
| Malignant tumors | 12 (0.9) | 72 (6.5) | <.001 | 0.23 (0.12–0.43) | <.001 |
| Pigmentation disorders | 75 (5.9) | 35 (3.2) | .002 | 2.09 (1.37–3.18) | .001 |
| Hair disorders | 44 (3.5) | 28 (2.5) | NS | 1.43 (0.88–2.34) | NS |
| Nail disorders | 35 (2.8) | 26 (2.3) | NS | 1.05 (0.62–1.77) | NS |
| Other skin disorders | 28 (2.2) | 22 (2) | NS | 1.14 (0.64–2.03) | NS |
| Mucosal disorders | 5 (0.4) | 8 (0.7) | NS | 0.64 (0.20–2–01) | NS |
| Vascular disorders | 8 (0.6) | 4 (0.4) | NS | 1.77 (0.52–6.01) | NS |
| Toxic skin reactions | 5 (0.4) | 3 (0.3) | NS | 1.86 (0.42–8.13) | NS |
Abbreviations: OR, odds ratio; NA, not applicable; NS, nonsignificant.
The growing influx of immigrants in Spain has increased demands on the Spanish health care system. According to a study conducted in Zaragoza in 2004, immigrants accounted for 4% of all dermatology patients, while studies of demand for specialist outpatient care in the autonomous community of Madrid reported that immigrants accounted for 3.2% of all patients requiring nonurgent psychiatric care2 and 4.1% of those requiring neurological care.3 The Madrid studies were conducted in 2001 and 2002, a time when the immigrant population in the area accounted for 10% of the total population of the community. In our health district, consultations by immigrant patients accounted for 4.1% of all dermatology consultations in the study period, at a time when the immigrant population accounted for 11% of the population in Alicante and 8.2% of the overall Spanish population.
Like other authors, we found that immigrant patients are young (mean age, 29 years) and mostly female. National statistics for 2006, however, show that there were slightly more immigrant men than women in the country.11 The fact that we detected more women than men in our group might be because the majority of patients were from Latin America, and women outnumbered men in this subpopulation.11
It is important to study the characteristics of dermatology patients from other countries because, among other reasons, some patients in this population have skin types that are different from those of Spanish patients. Accordingly the frequency and form of presentation of certain diseases may vary. Furthermore, immigrants constitute a heterogeneous group of individuals from different geographic regions with specific sociodemographic characteristics that may also influence the prevalence of certain skin disorders.
The most common skin disorders detected in our study were eczema, nongenital warts, and acne. Only 1 other Spanish study to date has analyzed skin disorders in the immigrant population.4 In that study, the authors reported that infections in general, and fungal infections in particular, were the most common skin conditions in immigrant patients in Zaragoza. Our results are not directly comparable to theirs, however, as the Zaragoza study treated eczema and atopic dermatitis as separate entities. If the authors had considered atopic dermatitis to be a form of eczema, this would have been the most prevalent skin disorder among the immigrant patients they studied. Viral infections, including warts, made up the second most common group of skin diseases. Finally, the third most prevalent skin condition, acne, was also the third most frequent in our immigrant population.
In studies of immigrant populations outside Spain, Halder and Nootheti12 (Washington DC, USA), Taylor13 (New York, USA), and Child et al.14 (London, UK) have reported that acne and eczema, in that order, were the most common skin disorders in immigrants. In a study of Latin American immigrants in New York, the results of Sánchez15 coincided with ours in that the most common skin disorders were eczema, warts, and acne.
Eczema, which was the most frequent reason for consultation by immigrants in our study, encompasses a range of conditions, but the most prevalent ones were atopic dermatitis and chronic eczema. We think that skin type might favor the development of atopic dermatitis. The presentation of this condition is different in individuals with more highly pigmented skin, in which it takes on a color that is more violaceous than red, possibly making it more difficult to diagnose in primary care and leading to more referrals to the dermatologist. Occupation, as well as skin type, might play a role in the persistence of the condition as immigrants are often domestic workers or employed in building or hotel and restaurant trades.
Significant differences were found between immigrant and Spanish patients in the prevalence of certain skin disorders. These differences can be attributed to various factors. As mentioned, eczema is probably more common in immigrants because of their skin type and occupation. Skin type might also favor the development of xerosis in darker-skinned individuals, as might a lower use of moisturizing products, which might not be considered an essential item by immigrants, who tend to have fewer resources.Certain types of alopecia are common in black patients16 and this might partly explain why we observed more cases in immigrants than in Spanish patients. On the other hand, no cases of alopecia were observed in sub-Saharan immigrants, most of whom were black. The difference thus might be due to the fact that Latin American women consult more about hair loss. The lower prevalence of melanocytic nevi detected in the immigrant group can probably be explained by the fact that most of the patients analyzed had highly pigmented skin as melanocytic nevi are reported to be less common in individuals with a dark complexion.17–20
Similarly, the lower frequency of squamous cell carcinoma, actinic keratosis, and melanoma in the immigrant group would be attributable to skin type and younger age. Skin cancer is less common in individuals with darkly pigmented skin13,16,21,22 as melanin content and melanosome dispersion exert a protective effect.16 Furthermore, even though we only considered Spanish patients younger than 60 years in the comparison of skin disorder prevalence, the mean age of the Spanish patients was still higher than that of the immigrants and both squamous cell carcinoma and actinic keratosis are more common in older patients.23,24
A higher prevalence of lupus has been reported in black individuals than white individuals, although similar rates have been described in Latin Americans and whites.25 Because our immigrant group mostly consisted of Latin Americans, we expected to find a similar frequency of lupus in immigrant and nonimmigrant patients. However, this disease was actually more common in the Spanish group, possibly because this chronic condition requires many follow-up visits, increasing the number of consultations related to this diagnosis in the Spanish group.
We detected a higher frequency of pigmentation disorders in the immigrant group; this was to be expected as these disorders are more common in black, Latin American, and Asian individuals.12,13,15
The significantly higher frequency of infectious diseases we detected in immigrants coincides with the findings of Porta et al.,4 who reported higher rates of onychomycosis, tinea, genital warts, syphilis, and scabies in this population. In our study, only tinea, scabies, and herpes simplex infection were significantly more common in immigrants than in nonimmigrants; the higher percentages of molluscum contagiosum, onychomycosis, and pityriasis versicolor in immigrants, however, were not significantly different. In our study, immigrants had a higher frequency of scabies and tinea than Spanish patients, possibly because they live in more crowded living conditions with worse hygiene and sanitation.26 The higher prevalence of herpes simplex infection in the immigrant group might also be due to crowded living conditions, which facilitate the spread of disease, or indeed to stress, which is common among immigrants and can contribute to viral reactivation. Nongenital warts are very common in both immigrants and nonimmigrants. We believe that the higher frequency of warts detected in the Spanish patients in our series can be attributed to immigrants’ lower rate of consultation about this disease (due to greater health care access difficulties) rather than to a truly lower incidence in the immigrant population.
We would like to stress that we observed no cases of leprosy in any of the immigrant patients seen by the dermatology units during the study period (1 year). Even though leprosy is now typically associated with immigration, our findings indicate that this disease is not common in immigrants, and indeed, very few cases have been reported in Spain.27,28 Dermatologists should, nonetheless, remain alert to the possibility of leprosy in the immigrant population as an early diagnosis can prevent disabilities and the spread of disease.
The immigrant population in Spain is highly heterogeneous and includes individuals from countries with a very high prevalence of sexually transmitted diseases (STDs). Immigrants are considered to be at high risk of acquiring STDs for numerous reasons, including conditions associated with immigration, such as human trafficking, in addition to precarious social and economic conditions, and less stable partnerships.29,30 Nonetheless, we observed very few cases of STD in our immigrant population; there were just 14 cases of genital warts, which accounted for 1.1% of all the diagnoses in this group. This finding can be attributed to the fact that most STDs are treated at a specialist clinic in our area; this clinic guarantees anonymity and is easily accessible for immigrants as a national health service access card is not required.
Clinical research may have limitations related to study design, procedures, and data analysis. Our study has a number of limitations that may have influenced results. The cross-sectional design meant that we were unable to follow patients over time. Consequently, changes in disease activity were not recorded, and we might have missed certain diagnoses. For example, we observed no cases of rare tropical diseases such as onchocerciasis or leprosy. Additionally, because the data were collected by different dermatologists, our results might also have been influenced by interobserver variability; however, considering the organization of the Spanish health care system, it would have been practically impossible to have had all the immigrants seen by a single dermatologist. Finally, differences in the prevalence of certain disorders between immigrant and Spanish patients may have failed to reach statistical significance because of the small numbers of immigrants from certain geographic regions and the low frequency of certain disorders.
In conclusion, the most common reasons for consultation by immigrants in our health care district are eczema, nongenital warts, and acne. Furthermore, because the infections diagnosed most frequently in the immigrant group (nongenital warts, molluscum contagiosum, onychomycosis, scabies, and tinea) are common in many countries, it can be concluded that immigration in Spain does not pose a significant risk for the spread of imported skin diseases from tropical countries.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Albares MP, et al. Estudio epidemiológico de la patología cutánea en la población inmigrante de Alicante. Actas Dermosifiliogr. 2012;103:214–222.