Lupus erythematosus is a chronic autoimmune inflammatory disease with a wide clinical spectrum and variable clinical course. Few studies have analyzed the characteristics of patients with only cutaneous lupus erythematosus (CLE). The aim of this study was to describe the epidemiological, clinical, and immunological characteristics of a series of patients diagnosed with CLE.
Patients and methodsAn analysis was performed of the data from all patients over 18 years of age with a diagnosis of CLE and seen between January 1, 2007 and December 31, 2011 in a tertiary hospital.
Results and conclusionsOne hundred one patients were included in the study. The mean age at diagnosis was 40 years and 84% were women. Subacute forms of presentation were observed in 94% of patients. The chronic discoid forms were localized to the head and neck in 79% of cases, whereas the subacute forms were on the trunk in 97% of cases. Patients with acute forms were positive for antinuclear, anti-DNA, anti-smooth muscle, and anti-RNP (ribonucleoprotein) antibodies, whereas anti-Ro and anti-La antibodies predominated in patients with subacute forms. Seventeen patients presented more than 1 subtype of CLE. Fifteen (88%) of these patients received immunosuppressor treatment versus 44 (52%) of the other 84 patients with only 1 subtype of CLE. Patients with distinct subtypes of CLE present different clinical and immunological characteristics. Oral immunosuppressants are often needed to control the disease in a large proportion of patients with different subtypes of CLE.
El lupus eritematoso es una enfermedad inflamatoria crónica autoinmune con un amplio espectro clínico y evolutivo. Existen pocos estudios sobre las características de los enfermos de lupus eritematoso exclusivamente cutáneo. El presente estudio pretende describir las características epidemiológicas, clínicas e inmunológicas de una serie de pacientes diagnosticados de lupus eritematoso cutáneo.
Pacientes y métodoSe analizaron los datos referentes a todos los pacientes mayores de edad diagnosticados de lupus eritematoso cutáneo que fueron atendidos por este motivo entre el 1 de enero de 2007 y el 31 de diciembre de 2011 en un hospital de tercer nivel.
Resultados y conclusionesUn total de 101 pacientes fueron incluidos en el estudio. La edad media al diagnóstico fue de 40 años. El 84% fueron mujeres, representando el 94% en las formas subagudas. El 79% de las formas crónicas discoides se localizaron exclusivamente en la cabeza y el cuello, mientras que el 97% de las formas subagudas se localizaron en el tronco. Las formas agudas presentaron positividad en los títulos de ANA, anti-ADN, anti-Sm y anti-RNP. Los anticuerpos anti-Ro y anti-La predominaron en las formas subagudas. Diecisiete pacientes presentaron más de un subtipo de lupus eritematoso cutáneo; 15 de estos 17 (88%) pacientes recibieron tratamiento con inmunosupresores frente a 44 de 84 (52%) de los que presentaron un solo subtipo de lupus eritematoso cutáneo.
Los pacientes pertenecientes a los distintos subtipos de lupus eritematoso cutáneo presentan unas características clínicas e inmunológicas diferenciadoras. Existe una importante proporción de pacientes con distintos subtipos de lupus eritematoso cutáneo que suelen necesitar tratamientos con inmunosupresores orales para el control de su enfermedad.
Lupus erythematosus (LE) is a chronic, relapsing autoimmune inflammatory disease. It has a wide clinical spectrum and the clinical course can vary considerably, ranging from serious systemic disease to chronic, indolent forms.1,2 The organs most frequently affected by LE are the skin, joints, and kidneys. Cutaneous lesions are often the first sign of the disease. The cutaneous manifestations of LE are classified as specific or nonspecific according to their clinical and histologic features.3 LE-specific lesions—that is, cutaneous lupus erythematosus (CLE)—are classified as acute (associated with systemic lupus erythematosus [SLE]), subacute, or chronic. Chronic discoid LE is the most common cutaneous form of LE.
Nearly all epidemiologic studies of patients with LE have involved patients with SLE. Few authors have investigated the characteristics of patients with CLE.
In this study, we describe the epidemiologic, clinical, and immunologic characteristics of a series of patients diagnosed with CLE who were treated in a specialized unit of a tertiary hospital and analyze the variation in these variables as a function of CLE subtype. We also consider the number of patients who had more than 1 distinct subtype of CLE and whether or not the presence of multiple CLE subtypes in a single patient is relevant to prognosis or therapeutic management.
Patients and MethodWe analyzed the patient data of all adults diagnosed with CLE who were seen for this disease between 1 January 2007 and 31 December 2011 in the specialized connective tissue disease unit of the dermatology department of Hospital General Universitario Gregorio Marañón, a hospital serving a catchment population of approximately 600 000 people in the Autonomous Community of Madrid. The diagnosis of CLE was histologically confirmed in all cases. Patients were classified according to clinical and histologic characteristics into 3 CLE subtypes: acute cutaneous LE (ACLE), subacute cutaneous LE (SCLE), or chronic discoid LE (CDLE).
Patients who had cutaneous manifestations associated with more than 1 CLE subtype were considered to have the subtype that appeared first or, if more than 1 subtype had appeared simultaneously, the subtype with the greatest extent and duration.
The study protocol excluded patients who met the criteria for SLE but did not have LE-specific cutaneous manifestations, patients who had one of the less common forms of CLE (LE tumidus [n=6], LE panniculitis [n=2], chilblain LE [n=2], bullous LE [n=1]), and patients who had clinical findings consistent with CLE but whose diagnosis was not confirmed on follow-up.
The following variables were included in the descriptive analysis: age at diagnosis, sex, site of lesions, the presence of antinuclear antibody (ANA) titers greater than 1:160, and the presence of LE-specific antibodies (anti-double-stranded-DNA antibody [anti-dsDNA], anti-Smith antibody [anti-Sm], anti-ribonucleoprotein antibody [anti-RNP], anti-Ro antibody, and anti-La antibody). Complement levels (C3, C4) were not included in the analysis because these tests were only requested for patients in whom SLE was suspected.
We also noted the systemic treatments received by the patients. The antimalarial agent initially prescribed was hydroxychloroquine in all cases. Chloroquine was prescribed for patients who did not show significant improvement after 4 months of treatment with hydroxychloroquine. When the patient did not improve after treatment with antimalarial agents, immunosuppressants (corticosteroids, methotrexate, azathioprine) or thalidomide were prescribed; the need for these treatments was only recorded for patients who received them for more than 3 consecutive weeks. The adverse effects associated with treatment with antimalarial agents (hydroxychloroquine, chloroquine) and thalidomide were also noted.
The statistical analysis was a retrospective, descriptive study. Univariate analysis of qualitative variables was performed using the Pearson χ2 test and the Fisher exact test. Qualitative and quantitative variables were analyzed using the t test. When necessary, the homogeneity of variance test and the Bonferroni test were applied. A P value of<.05 was considered statistically significant. The descriptive study and the analytic study of the variables were performed using the SPSS statistical package version 15 (SPSS, Chicago, Illinois, USA).
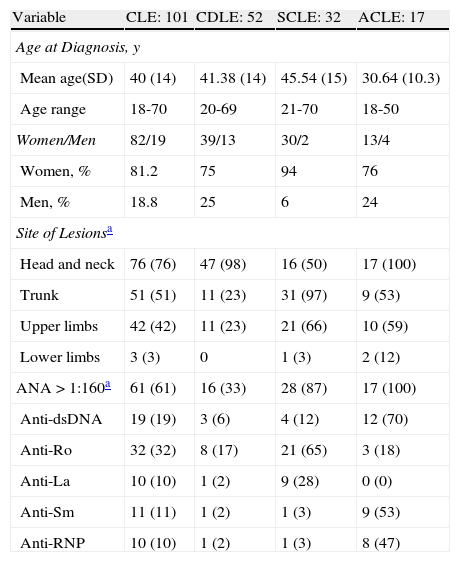
ResultsA total of 101 patients with a biopsy-confirmed diagnosis of CLE were included in the study. Table 1 shows the main epidemiologic, clinical, and immunologic characteristics of the patients. Patients with ACLE had a younger mean age at diagnosis than patients with any other subtype of CLE and were more likely to be positive for ANAs, anti-dsDNA, anti-Sm, and anti-RNP. All patients presented the characteristic facial rash. In 41 patients with CDLE (41%), the lesions were located only on the head and neck. Only 33% of patients with CDLE were positive for ANAs (titers ≥ 1:160).
Epidemiologic, Clinical, and Immunologic Characteristics of Patients with Cutaneous Lupus Erythematosus.
| Variable | CLE: 101 | CDLE: 52 | SCLE: 32 | ACLE: 17 |
| Age at Diagnosis, y | ||||
| Mean age(SD) | 40 (14) | 41.38 (14) | 45.54 (15) | 30.64 (10.3) |
| Age range | 18-70 | 20-69 | 21-70 | 18-50 |
| Women/Men | 82/19 | 39/13 | 30/2 | 13/4 |
| Women, % | 81.2 | 75 | 94 | 76 |
| Men, % | 18.8 | 25 | 6 | 24 |
| Site of Lesionsa | ||||
| Head and neck | 76 (76) | 47 (98) | 16 (50) | 17 (100) |
| Trunk | 51 (51) | 11 (23) | 31 (97) | 9 (53) |
| Upper limbs | 42 (42) | 11 (23) | 21 (66) | 10 (59) |
| Lower limbs | 3 (3) | 0 | 1 (3) | 2 (12) |
| ANA>1:160a | 61 (61) | 16 (33) | 28 (87) | 17 (100) |
| Anti-dsDNA | 19 (19) | 3 (6) | 4 (12) | 12 (70) |
| Anti-Ro | 32 (32) | 8 (17) | 21 (65) | 3 (18) |
| Anti-La | 10 (10) | 1 (2) | 9 (28) | 0 (0) |
| Anti-Sm | 11 (11) | 1 (2) | 1 (3) | 9 (53) |
| Anti-RNP | 10 (10) | 1 (2) | 1 (3) | 8 (47) |
Abbreviations: ACLE, acute cutaneous lupus erythematosus; ANA, antinuclear antibodies; anti-dsDNA, anti-double-stranded-DNA antibody; anti-La, anti-La antibody; anti-RNP, anti-ribonucleoprotein antibody; anti-Ro, anti-Ro antibody; anti-Sm, anti-Smith antibody; CDLE, chronic discoid lupus erythematosus; CLE, cutaneous lupus erythematosus; SCLE, subacute cutaneous lupus erythematosus.
Although women accounted for a majority of patients in all CLE subtypes, the highest percentage of female patients (94%) was in the SCLE group. Some 97% of patients in the SCLE group had lesions on the trunk, in most cases of the annular polycyclic type. The antibodies associated with photosensitivity (anti-Ro and anti-La) predominated in this group.
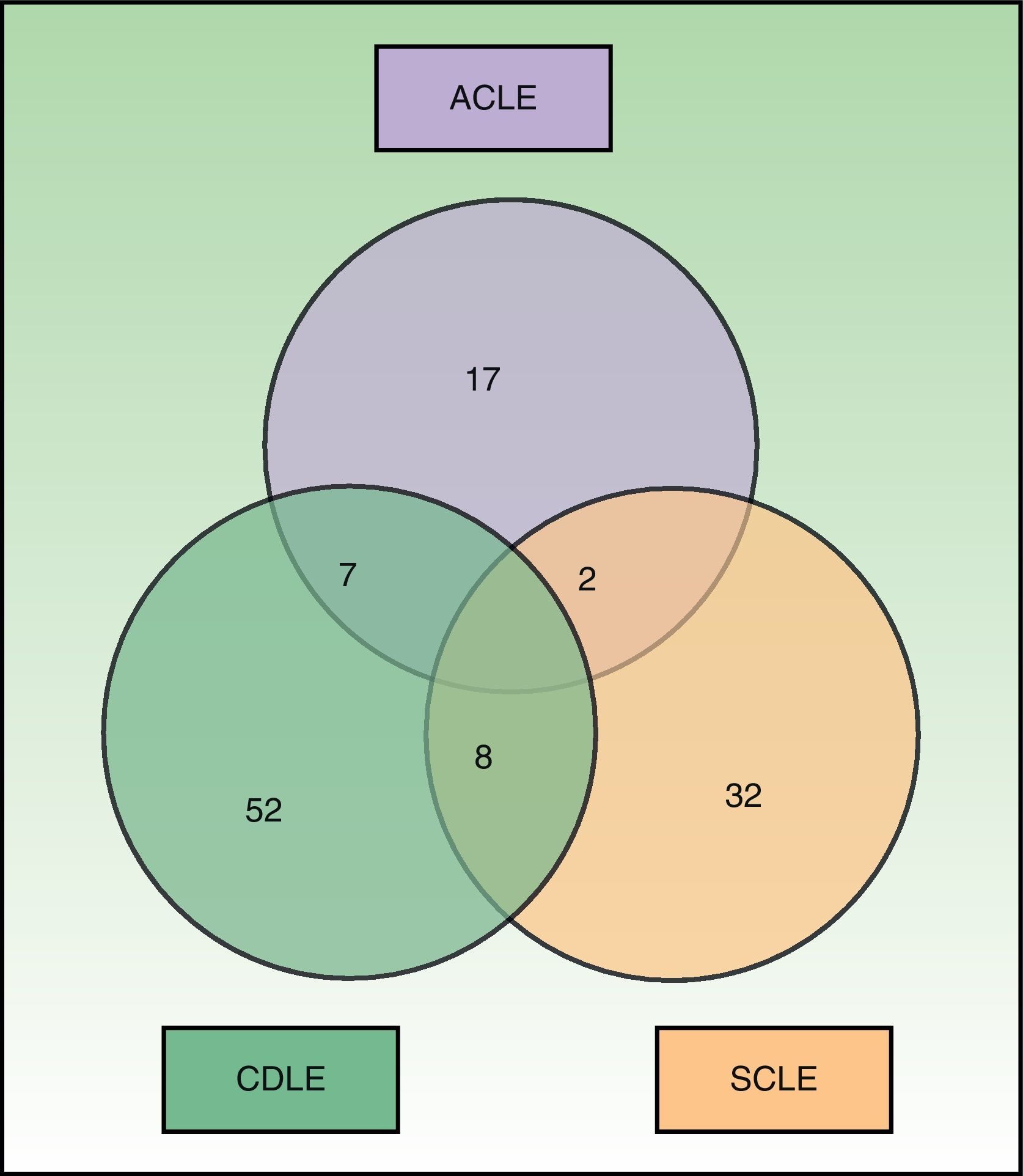
Fig. 1 shows the distribution of the patients by CLE subtype. A total of 17 patients had more than 1 subtype of CLE; the most common combination was CDLE and SCLE (8), followed by ACLE and CDLE (7) and ACLE and SCLE (2). Treatment with immunosuppressants was prescribed to 15 of the 17 patients with more than 1 CLE subtype (88%), compared with 44 of the 84 patients with just 1 CLE subtype (52%) (P=.006). Moreover, patients with more than 1 form of CLE were significantly more likely to be positive for antibodies associated with SLE, such as anti-dsDNA, anti-Sm, and anti-RNP (P=.034).
A total of 96 patients (96%) received systemic treatment with synthetic antimalarial agents (hydroxychloroquine or chloroquine). The main adverse effects associated with these drugs were reversible visual disturbances (6 patients), intolerance and/or gastritis (6 patients), tremors (2 patients), noncicatricial diffuse alopecia (3 patients), and pigmentation of the nail plate (1 patient). Thalidomide was prescribed to 13 patients, 4 of whom (31%) developed a peripheral neuropathy that necessitated discontinuation of the treatment. A total of 56 patients received treatment with immunosuppressants.
DiscussionMost epidemiologic studies of patients with LE have focused on patients with SLE, and very few studies have been carried out on the various subtypes of CLE.4–8 While systemic involvement tends to be mild in most patients with CLE, the disease has a major impact on quality of life because the lesions are usually located on the face and the chronic forms can cause irreversible scarring. Moreover, up to 28% of patients with CDLE are susceptible to developing SLE.9
There is no consensus in the literature regarding the definition of CLE. The term is used interchangeably to refer to the independent primary cutaneous disease or to describe a series of specific manifestations that occur in patients with SLE. Sontheimer6 was the first author to propose the classification of skin lesions as either LE-specific or LE-nonspecific. Additionally, in 1979 he proposed the term subacute CLE to refer to a CLE subtype, distinct from the chronic cicatricial forms of the disease, characterized by annular or psoriasiform lesions in sun-exposed areas, the absence of systemic symptoms, and the presence of circulating anti-Ro antibodies.5,6 This subacute form of the disease appeared to occur more frequently in young women, with peak incidence rates in the fourth decade of life.7 Since SCLE was first described, only 1 new CLE subtype—LE tumidus—has been proposed10; however, this entity is still being defined and has not been unanimously accepted in the international literature.11
Very few epidemiologic studies on CLE have been carried out in Spain. Table 2 compares the most important epidemiologic characteristics of our patients with those reported in similar studies.12–14 However, there are important differences between our patients and those included in other studies. Our study does not include less common forms of CLE such as LE tumidus and LE panniculitis. Biazar et al.14 included patients from 13 European countries, and this could account for some of the differences between the results of their study and ours. Although Vera-Recabarren et al.12,13 studied Spanish patients, their analysis compared the clinical and immunologic characteristics of patients with CDLE with those of patients with SCLE12 but did not consider patients with ACLE. Despite these differences, our results are very similar to those of the other studies, especially with regard to epidemiologic characteristics. However, some significant differences did emerge, including the fact that our patients were diagnosed at a younger age and were more likely to be positive for anti-dsDNA than the patients studied by Biazar et al.14
Comparison of Epidemiologic and Immunologic Characteristics of Our Patients With Those Reported in Similar Studies.
| Vera-Recabarren et al.12 (n=270) | Biazar et al.14 (n=1002) | Avilés et al. (n=101) | ||||||
| Subtype of CLE | SCLE (n=112) | CCLE (n=158) | ACLE (n=304) | SCLE (n=236) | CCLE (n=397) | ACLE (n=17) | SCLE (n=32) | CDLE (n=52) |
| Mean Age at Diagnosis, y (SD) | 43.6 (18) | 43.6 (15) | 46.6 (15.6) | 57.2 (15.5) | 49.7 (14.3) | 30.6 (10.3) | 45.5 (15) | 41.4 (14) |
| Women/Men | 77/35 | 98/60 | 250/54 | 178/58 | 301/96 | 13/4 | 30/2 | 39/13 |
| Immunologic Markersa | ||||||||
| ANA | 52.5 | 17 | 80.6 | 73.6 | 53.6 | 100 | 87 | 33 |
| Anti-dsDNA | 17.2 | 3.9 | 32.4 | 11.6 | 18.2 | 70 | 12 | 6 |
| Anti-Ro | 42.2 | 3.7 | 47.4 | 72.1 | 22 | 18 | 65 | 17 |
| Anti-La | 15.4 | 0 | 27.5 | 36.2 | 7 | 0 | 28 | 2 |
| Anti-Sm | 6.7 | 0.8 | 18.7 | 3.8 | 7.2 | 53 | 3 | 2 |
| Anti-RNP | 7.8 | 1.6 | 24.1 | 10.4 | 11.3 | 47 | 3 | 2 |
Abbreviations: ACLE, acute cutaneous lupus erythematosus; ANA, antinuclear antibodies; anti-dsDNA, anti-double-stranded DNA antibody; anti-La, anti-La antibody; anti-RNP, anti-ribonucleoprotein antibody; anti-Ro, anti-Ro antibody; anti-Sm, anti-Smith antibody; CCLE, chronic cutaneous lupus erythematosus; CDLE, cutaneous discoid lupus erythematosus; CLE, cutaneous lupus erythematosus; SCLE, subacute cutaneous lupus erythematosus.
In our study, 25 patients (17 with ACLE and 8 with SCLE) met at least 4 of the criteria for SLE established by the American Rheumatism Association (ARA). However, like other authors, we believe that these criteria should not be applied to patients with CLE because they are perhaps too sensitive but not very specific.15 Consequently, we believe that SLE is frequently diagnosed in patients who will never develop systemic manifestations associated with LE. Moreover, in such cases, any nonspecific symptoms reported by the patient—such as joint pain, headache, and fatigue—tend to be erroneously attributed to LE.
With this problem in mind, the European Academy of Dermatology (EADV) compared the 11 ARA criteria with a series of 13 additional criteria in a group of 140 patients who had LE with or without systemic involvement.16 The 13 additional criteria included the presence of histologic features such as the lupus band, complement and immunoglobulin G levels, and the presence of annular or papulosquamous lesions characteristic of SCLE. These additional criteria were later analyzed by other authors, who found them to be more specific but less sensitive.15,17 Since then, however, these criteria have not been used and they seem to have been forgotten by the international scientific community.
In conclusion, patients with different subtypes of CLE have distinct clinical and immunologic characteristics. In the absence of consensus on a definition that makes it possible to differentiate cutaneous forms of LE from SLE, the dermatologist's role in the correct diagnosis and classification of such patients is fundamental. Moreover, some patients with CLE present skin lesions that belong to different CLE subtypes. Systemic immunosuppressants are usually required to properly manage the disease in these patients.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Data confidentialityThe authors declare that they have followed the protocols of their hospitals concerning the publication of patient data and that all patients included in this study were appropriately informed and gave their written informed consent.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Avilés Izquierdo J, Cano Martinez N, Lázaro Ochaita P. Características epidemiológicas de los pacientes con lupus eritematoso cutáneo. Actas Dermosifiliogr. 2014;105:69–73.