An 81-year-old man with a past history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, and chronic bronchitis presented with an asymptomatic lesion on the left popliteal fossa that had grown steadily in size since appearing 1 year earlier.
Physical ExaminationPhysical examination revealed a 6-mm-long erythematous pedunculated papule on the left popliteal fossa that was firm in consistency, showed no erosion or ulceration, and was not adherent to deeper tissues (Fig. 1). The patient had no palpable locoregional lymph nodes.
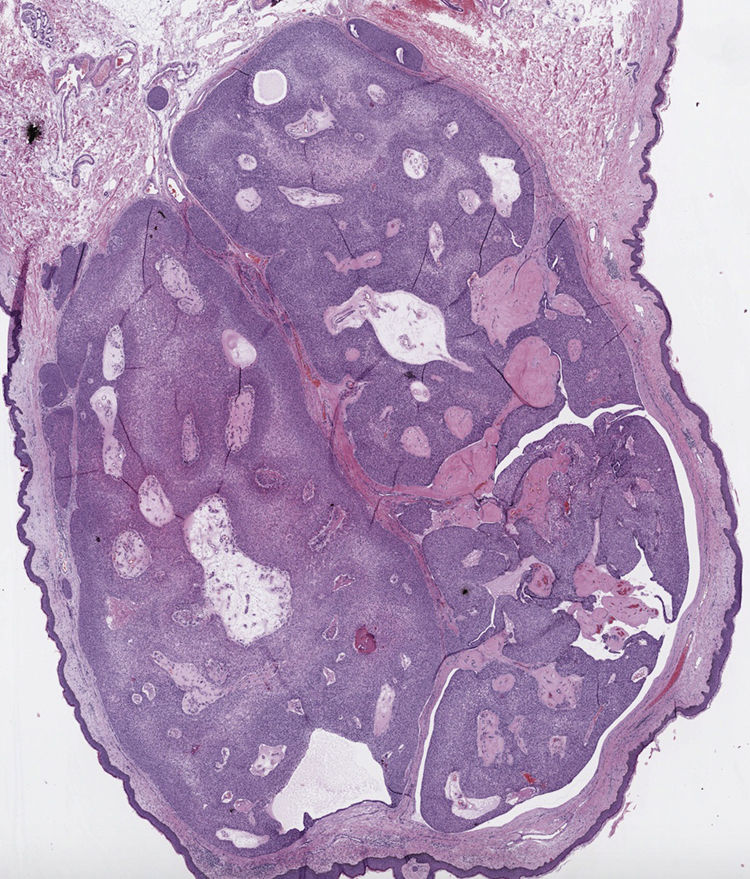
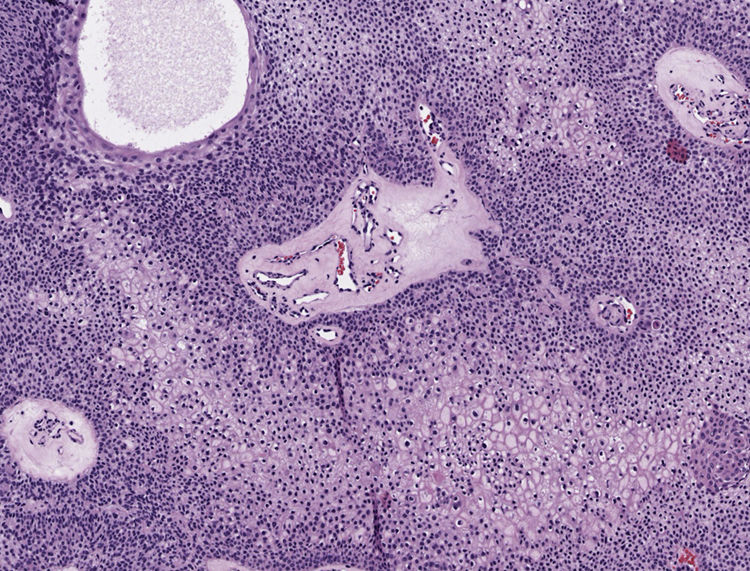
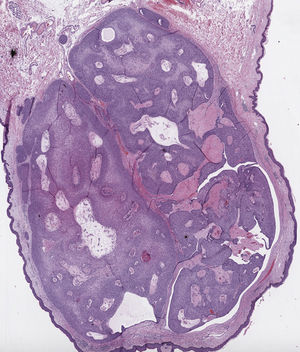
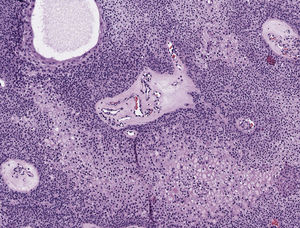
HistopathologyComplete excision of the lesion was performed. Pathologic examination revealed a nonencapsulated polypoid neoformation (Fig. 2) composed of dermal tumor nodules separated by fibrous tracts. The nodules consisted of 2 types of cells: round cells with clear cytoplasm showing a positive periodic acid-Schiff reaction (Fig. 3) and polyhedral cells with round nuclei and slightly basophilic cytoplasm. No mitotic figures or angiolymphatic or perineural invasion were observed. Also present were cysts containing homogeneous eosinophilic material, surrounded by a layer of cuboidal epithelial cells, with no evidence of decapitation secretion.
What Is Your Diagnosis?
DiagnosisNodular hidradenoma.
Clinical CourseFollow-up at 1 year showed no recurrence of the lesion.
CommentNodular hidradenoma (also known as apocrine hidradenoma, clear cell hidradenoma, solid-cystic hidradenoma, eccrine acrospiroma, and clear cell acrospiroma) is a benign tumor. The apocrine or eccrine differentiation of this entity has been the subject of debate. Some authors have reported decapitation secretion, which suggests an apocrine origin; others have noted the absence of apocrine secretion and the existence of ultrastructural features of immature eccrine glands.1 This entity is more common in women and tends to appear between the fourth and sixth decades of life, but cases in children have also been reported.2,3 The lesion tends to present as a single, slow-growing, skin-colored or erythematous-brownish nodule measuring less than 2-3cm in diameter, either firm in consistency or fluctuant if the cystic component is predominant. The tumors are generally asymptomatic but erosion or ulceration can be present and, in cystic lesions, serous discharge can be present.2 Pedunculated lesions—like that of our patient—have been reported but are very rare.4 The lesion can appear on any part of the body, although the head and neck, trunk, and upper limbs are the most common sites. Dermoscopy shows homogeneous reddish, bluish, bluish-red, or brown areas comprising all or part of the lesion, whitish vascular structures such as arborizing telangiectasias, and polymorphous atypical vessels, making these lesions difficult to distinguish from basal cell carcinomas and melanomas.5 Immunohistochemical analysis shows positivity for anticytokeratin CAM 5.2 in most tumors. Carcinoembryonic antigen, epithelial membrane antigen, S-100 protein, smooth muscle actin, and vimentin are also expressed in some cases. Staining with antibodies targeting various cytokeratin subtypes is variable in different parts of the tumor.2 However, immunohistochemical analysis is not usually necessary because this entity can be diagnosed easily with conventional techniques such as hematoxylin-eosin staining. Malignant transformation into hidradenocarcinoma is very rare and should be suspected when histologic examination reveals a pattern of infiltrative growth, necrosis, nuclear pleomorphism, abundant mitotic figures, and angiolymphatic or perineural invasion.6
Surgical resection is curative; however, the rate of recurrence—due to incomplete resection—is approximately 10%.2
In this article, we describe a case of nodular hidradenoma with a rare pedunculated presentation. This unusual variety of the lesion must be differentiated from entities of similar morphology, such as fibroepithelioma of Pinkus, fibrolipoma, and angioma. The histologic differential diagnosis includes other clear cell malignancies such as metastatic cancer (usually of renal cell carcinoma) and primary cutaneous tumors with follicular, sebaceous, and sweat gland differentiation.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García del Pozo MC, Martín de Hijas C, Iñíguez L. Pápula eritematosa pediculada en la rodilla. Actas Dermosifiliogr. 2018;109:543–544.