A 32-year-old man, under investigation for a 15-day history of fever and a painful cervical lymphadenopathy, was referred to the dermatology department for facial lesions of recent onset.
Physical ExaminationThe patient presented well-defined, slightly scaly, infiltrated erythematous-violaceous plaques on the face. They measured several centimeters in diameter and were not tender (Fig. 1).
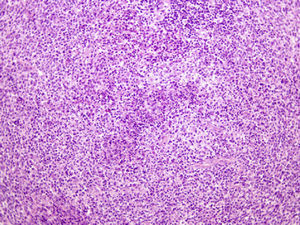
HistopathologyPunch biopsy of a lesion showed a superficial and deep perivascular lymphocytic infiltrate, with slight vacuolization of the basal layer of the epidermis (Fig. 2).
Additional TestsLaboratory tests including complete blood count, biochemistry, and coagulation studies gave normal results. The erythrocyte sedimentation rate was 30mm. Antinuclear antibodies, rheumatoid factor, and serological tests for cytomegalovirus, herpes simplex virus types 1 and 2, hepatitis B and C viruses, human immunodeficiency virus (HIV), Toxoplasma gondii, Bartonella henselae, Salmonella typhi, Brucella, Leptospira, and Francisella tularensis were negative. Serological tests were positive for Epstein-Barr virus (EBV) and parvovirus B19 immunoglobulin [Ig] G. The Mantoux test and chest radiograph were negative.
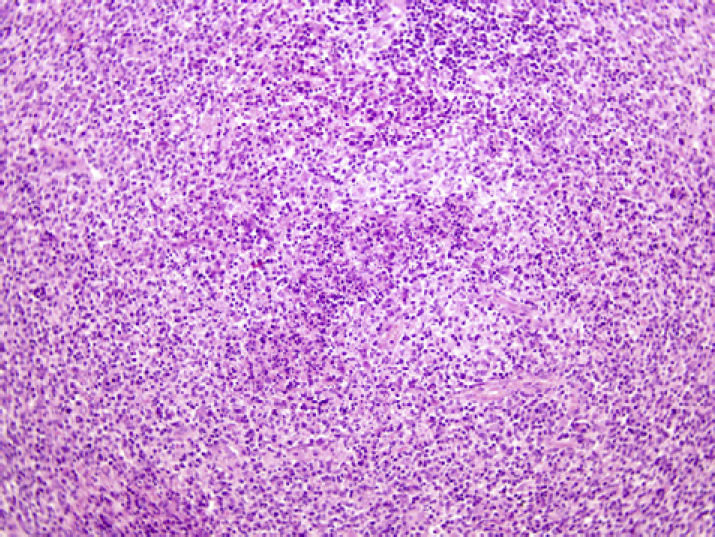
Ultrasound of the cervical region confirmed lymphadenopathies. Biopsy of a node revealed paracortical areas of apoptotic cell death without abscess formation, abundant karyorrhexis, and a proliferation of histiocytes and plasmacytoid monocytes, with an absence of neutrophils (Fig. 3).
What Is Your Diagnosis?
DiagnosisKikuchi-Fujimoto disease with skin involvement.
Clinical CourseTreatment was started with low-dose oral and topical corticosteroids. After 8 weeks, the fever and lymphadenopathies had resolved. However, the skin lesions persisted, and treatment was therefore started with hydroxychloroquine (400mg/d). There have been no repeat episodes of fever or lymphadenopathies, and only residual skin lesions remain after 2 years’ treatment.
DiscussionFirst described in 1972,1,2 Kikuchi-Fujimoto disease or histiocytic necrotizing lymphadenitis is a rare condition, which invariably resolves in a few weeks.1,2 The etiology is uncertain, although apoptosis plays a significant role. It could represent an exaggerated T-cell mediated response to certain antigens in genetically predisposed individuals. It has been suggested that Kikuchi-Fujimoto disease is triggered by autoimmune disease or infection by certain viruses such as Epstein-Barr virus, human herpesvirus 6, human herpesvirus 8, HIV, herpes simplex virus, hepatitis B virus, human T-cell leukemia virus type 1, parvovirus B19, paramyxovirus, and parainfluenza virus, in addition to other microorganisms such as Yersinia enterocolitica and Toxoplasma. It has also been reported with Still disease, antiphospholipid syndrome, hemophagocytic syndrome in children, brachial plexus neuritis, mononeuritis multiplex, bilateral panuveitis, aseptic meningitis, brucellosis, and Wells syndrome. Kikuchi-Fujimoto disease mainly affects young women and is clinically identified by painful cervical lymphadenopathy associated with fever, myalgia, neutropenia, and rarely (less than 40% of cases) skin rash.
From a dermatological perspective, lesions have been described as macules, papules, plaques, nodules, and ulcers, on the upper part of the body (face, arms, and trunk).3,4 Skin biopsy usually shows a superficial and deep perivascular infiltrate, edema of the papillary dermis, vacuolization, and necrotic keratinocytes in the basal layer of the epidermis. Patchy infiltrates of lymphoid cells and histiocytes and nuclear remnants similar to those found in the lymph node are also typical.5
Diagnosis requires histopathological study of a lymph node biopsy and the differential diagnosis must be made with Hodgkin disease, high-grade lymphoma, and lymphadenitis associated with systemic lupus erythematosus. Infectious lymphadenitis (EBV, herpes virus, Bartonella henselae, or Toxoplasma) should also be excluded.
Treatment requires supportive measures and occasionally the administration of low-dose oral corticosteroids. Although the disease is self-limiting and resolves in a few weeks, skin manifestations are more persistent and must be managed in a similar way to those of cutaneous lupus erythematosus.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to our pathology department, without whose help it would not be possible to establish many diagnoses.
Please cite this article as: Fueyo-Casado A, et al. Fiebre, linfadenopatías cervicales y placas eritematovioláceas faciales. Actas Dermosifiliogr. 2011;102:629-30.