Bacterial superinfection associated with epidermal growth factor receptor (EGFR) inhibitors is a recognizable clinical and histopathological entity that can be differentiated from the classic papulopustular rash. The different location and distribution of the lesions, together with an onset that is typically later than that of papulopustular rash, enable it to be distinguished based on clinical findings. Correct diagnosis is essential, since treatment must be selected carefully if we are to prevent severe comorbidities in cancer patients, including the potential risk of sepsis.1
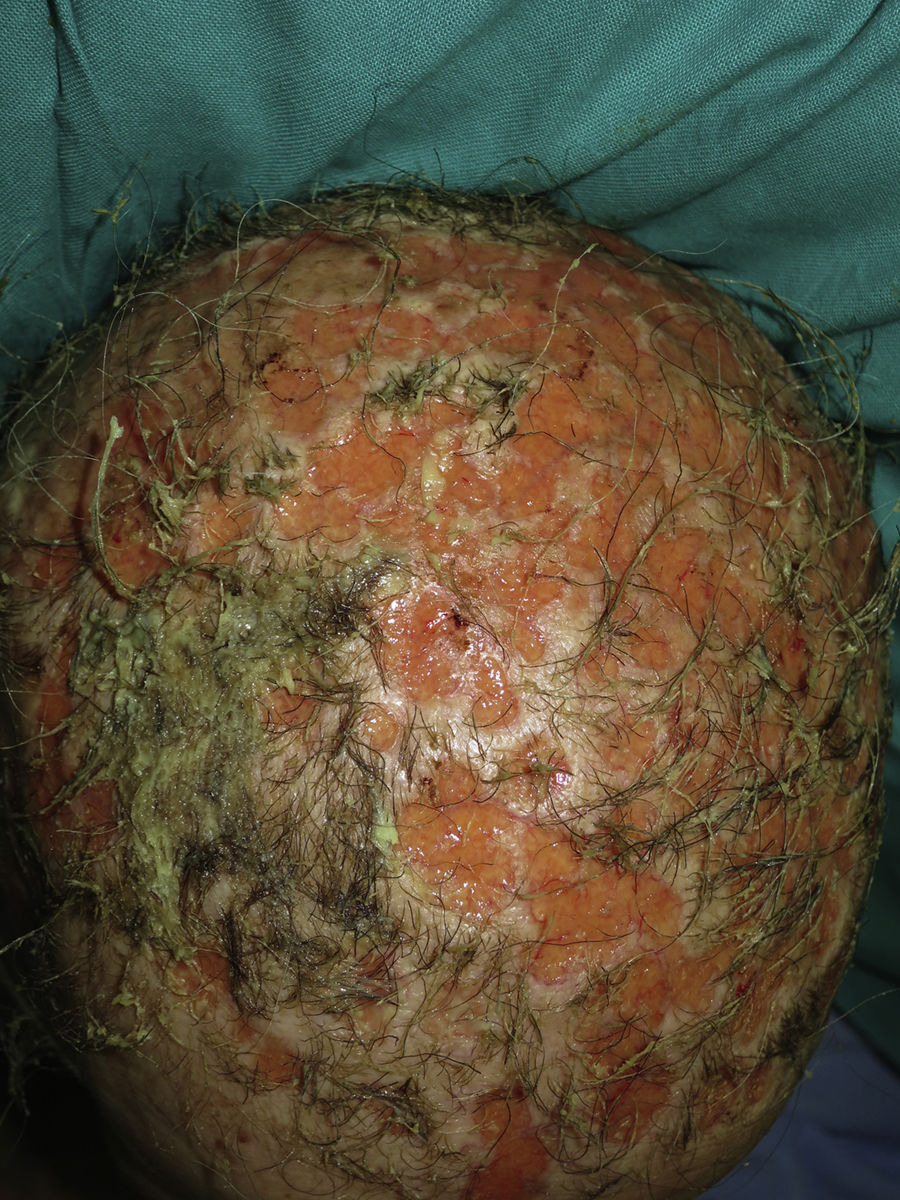
A 66-year-old woman diagnosed with metastatic pulmonary adenocarcinoma who was receiving treatment with erlotinib at an initial dose of 150mg/d presented with grade 1 papulopustular rash that progressed to grade 2 rash during the following 3 weeks. The response to topical corticosteroids combined with doxycycline was poor. Therefore, we decided to reduce the dose of erlotinib to 100mg/d, with good control of the papulopustular lesions. Six months later, the patient was referred to the dermatology outpatient clinic for evaluation of crusted lesions on the scalp that had first appeared 3 months previously. Physical examination revealed generalized swelling throughout the scalp over a confluent and malodorous pustular base. Given the diagnosis of bacterial superinfection associated with erlotinib, we took a sample of the exudate for culture and started doxycycline 100mg every 12hours. Methicillin-sensitive Staphylococcus aureus was isolated in culture, and treatment was adjusted according to the antibiogram. However, the patient's condition progressed over the following days, with rapid loss of tufts of hair, leaving de-epithelialized alopecic plaques with a scar-like appearance alternating with pustular areas throughout the scalp (Fig. 1). We made a diagnosis of folliculitis decalvans due to bacterial superinfection associated with erlotinib. The patient died of acute pulmonary thromboembolism a week later.
Bacterial superinfection of papulopustular rash secondary to EGFR inhibitors is not an uncommon complication. According to a study performed in 2010 on a series of 221 patients, the complication affected 29% of those treated with these EGFR inhibitors.2 As for pathophysiology, inhibition of EGFR in keratinocytes leads to epidermal thinning. Furthermore, in vitro evaluation has shown that there is a reduction in the production of antimicrobial peptides and ß-defensins by keratinocytes, as well as inhibition of the activation and proliferation of T lymphocytes.3,4
Braden and Anadkat5 correctly defined this condition in a study published in 2016 that included 157 patients treated with EGFR inhibitors who had developed classic papulopustular lesions or infections resulting from bacterial superinfection. The authors concluded that up to 23% of patients treated with these inhibitors develop symptoms compatible with bacterial superinfection, especially in the form of folliculitis caused by S aureus. In most cases, bacterial superinfection can be differentiated from papulopustular rash based on 2 criteria: distribution of lesions and time to onset after initiation of cancer treatment. Bacterial superinfection progresses with folliculitis lesions mainly on the abdomen, buttocks, arms, and legs. In contrast, classic papulopustular rash is predominantly cephalic, affecting the upper part of the back and chest, and more intense in seborrheic areas of the center of the face and sternum. As for time to onset after initiation of treatment, the papulopustular rash has a mean latency period of 1.5 weeks, compared with a mean of more than 28 weeks in the case of bacterial superinfection. Therefore, the authors state that we should suspect bacterial superinfection, regardless of the location of the lesions, provided that onset is at least 12 weeks after initiation of cancer treatment. Pruritus and pain may be present in both cases, although pain is much more common in cases of bacterial superinfection.
The treatment of bacterial superinfection requires empirical systemic antibiotics after culture of samples and subsequent adjustment based on the antibiogram. As S aureus is generally the pathogen involved, the recommended empirical treatment is clindamycin or trimethoprim-sulfamethoxazole, thus covering the possibility of community-acquired methicillin-resistant S aureus. Systemic involvement should be ruled out based on the clinical history. If there are good grounds for suspicion of systemic involvement, then a workup based on a laboratory analysis and complete blood count should be performed. It may even be necessary to consider admission to hospital and intravenous antibiotic therapy. Nevertheless, most cases respond to oral therapy at home with close monitoring.5
In conclusion, we present a case of bacterial superinfection associated with erlotinib that manifested as folliculitis decalvans, a complication that has received little attention in the literature.6–8 Knowledge of this entity enables the early management necessary to prevent severe local or systemic complications. The disease should be correctly differentiated from the classic papulopustular rash.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sahuquillo-Torralba A, Escutia-Muñoz B, Rodríguez-Serna M, Botella-Estrada R. Foliculitis decalvante por sobreinfección bacteriana secundaria a erlotinib. Actas Dermosifiliogr. 2018;109:363–364.