Granulomatous cheilitis (Miescher cheilitis), a condition characterized by recurrent swelling of the lips, is the most common monosymptomatic form of the Melkersson-Rosenthal syndrome. The aim of this study was to study the characteristics of patients diagnosed with granulomatous cheilitis at the dermatology department of our hospital over a period of 17 years.
Material and methodsWe performed a descriptive study of patients diagnosed with granulomatous cheilitis at our hospital between January 1993 and January 2010.
ResultsThe condition was diagnosed in 6 patients (4 women and 2 men), with a mean age of 49 years at the time of diagnosis. All the patients had recurrent swelling of the upper lip and 2 also had swelling in other parts of the face. The mean time from the onset of symptoms to the initial visit was approximately 16 months. There were no cases of facial palsy, and just 1 patient had a fissured tongue. None of the patients developed Crohn disease or any other granulomatous disorders during follow-up.
ConclusionsGranulomatous cheilitis is a rare disease. None of the patients in our series had gastrointestinal or neurologic symptoms. Accordingly, we believe that granulomatous cheilitis is an independent orofacial granulomatous disease which most often presents without accompanying signs or symptoms
La queilitis granulomatosa (QG) de Miescher representa la forma monosintomática más frecuente del síndrome de Melkersson-Rosenthal, que se caracteriza por una tumefacción labial recurrente. El objetivo de nuestro estudio fue describir las características de los pacientes con QG atendidos en nuestro servicio durante un periodo de 17 años.
Material y métodosEstudio descriptivo de los pacientes diagnosticados de QG atendidos en el Departamento de Dermatología desde enero de 1993 hasta enero de 2010.
ResultadosSe recogieron un total de 6 pacientes, con un ligero predominio femenino (4 mujeres y 2 hombres), y una media de edad al diagnóstico de 49 años. Todos presentaban una tumefacción en el labio superior, persistente y recurrente, junto con afectación de otras regiones faciales en 2 casos. La media de tiempo desde la aparición de los síntomas a la consulta inicial fue de aproximadamente 16 meses. En ningún paciente se observó la presencia de parálisis facial y únicamente se objetivó lengua fisurada en un caso. Durante los años de seguimiento ningún paciente fue diagnosticado de enfermedad de Crohn ni de otra enfermedad granulomatosa.
ConclusiónLa QG es una entidad infrecuente. Ninguno de los pacientes evaluados ha presentado sintomatología gastrointestinal o neurológica asociada, por lo que consideramos la QG de Miescher una patología independiente dentro del grupo de las granulomatosis orofaciales, no asociada a otros síntomas o signos como forma de presentación más frecuente.
Granulomatous cheilitis (Miescher cheilitis) is a rare condition that presents with recurrent swelling of the lips. It is the most common monosymptomatic form of Melkersson-Rosenthal syndrome, which is characterized by edema of the lips, facial palsy, and fissured tongue. In 1985, Wiesenfeld et al.1 coined the term orofacial granulomatosis to describe a series of noninfectious, nonnecrotizing granulomatous disorders of the lips, face, and oral cavity that included granulomatous cheilitis, Crohn disease, and sarcoidosis. Orofacial granulomatosis is therefore an umbrella term that encompasses a number of entities of diverse etiology, pathogenesis, and clinical features.
The aim of this study was to describe the characteristics of patients treated for granulomatous cheilitis in our department over a 17-year period.
Material and MethodsWe created a register of patients diagnosed with granulomatous cheilitis at the dermatology department of Hospital General Universitario de Albacete between January 1993 and January 2010. Only cases with both clinical and histologic confirmation were included. A list of patients who satisfied these criteria was obtained from the diagnostic database of the hospital's pathology department. Once the patients had been identified, we reviewed their medical histories and recorded their clinical data and course. Patients with a clinical diagnosis not confirmed by histology were excluded. The variables analyzed included sex, age at diagnosis, past history, family history, site of the lesions, associated signs and symptoms, time from onset to diagnosis, histopathology findings, additional tests (complete blood count; erythrocyte sedimentation rate; C-reactive protein levels; biochemistry; thyroid stimulating hormone levels; autoimmunity studies; immunoglobulin [Ig] levels; angiotensin-converting enzyme levels; serology for hepatitis B and C viruses and human immunodeficiency virus; chest radiography; and Mantoux test), treatment prescribed, clinical course, and duration of follow-up.
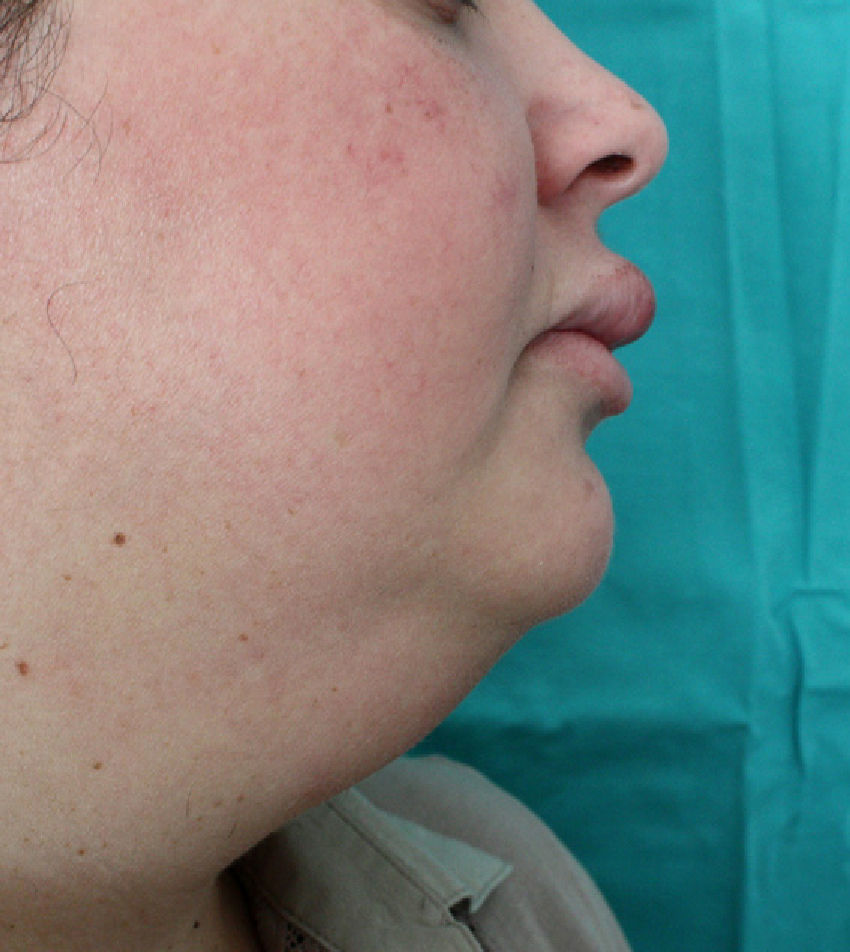
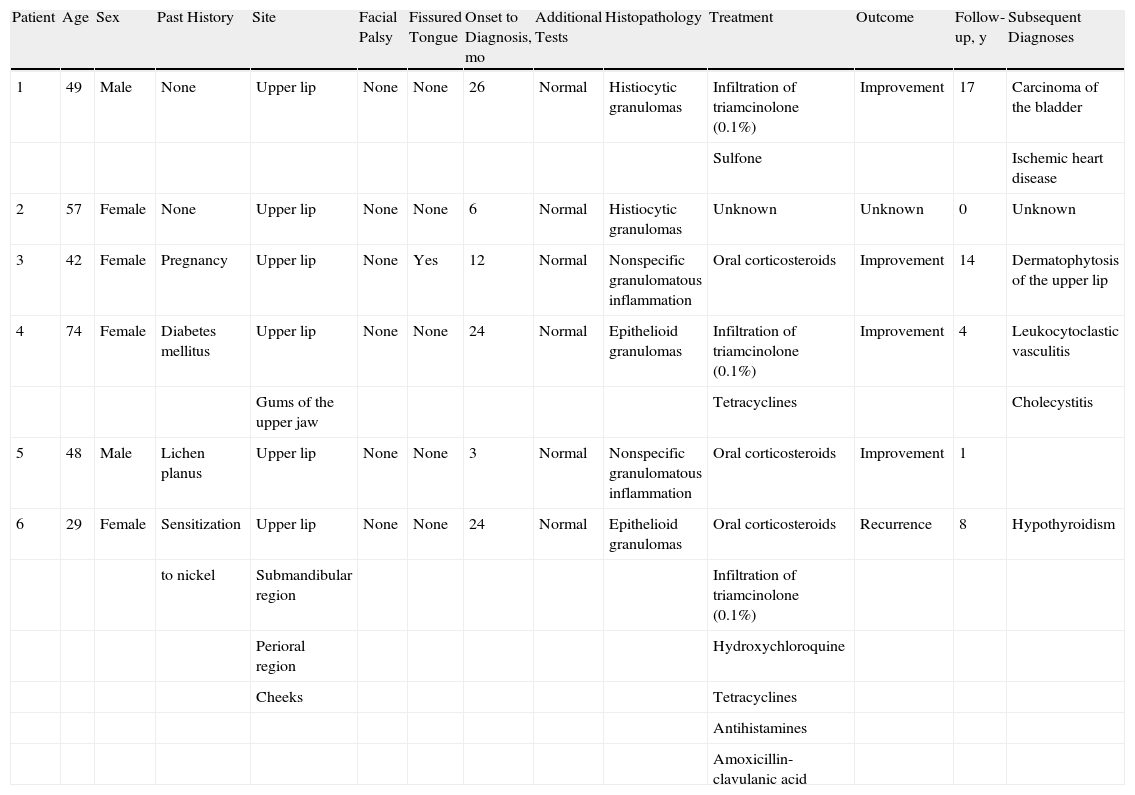
ResultsSix patients (4 women and 2 men) were included in the study (Table 1). The mean (SD) age at the time of diagnosis was 49.8 (15.1) years (range, 29-74 years). The mean time from symptom onset to hospital arrival was 15.83 (10.13) months (range, 3-26 months). All of the patients had persistent, recurrent swelling of the upper lip (Figs. 1-3). Two patients (33.33%) also had swelling in other parts of the face: patient 4 had swelling of the gums as well as the upper lip and patient 6 had lesions in the perioral region, cheeks, and submandibular region in addition to the upper lip (Fig. 4). In patient 6, a submandibular ultrasound imaging study showed enlarged cervical lymph nodes greater than 1 cm in diameter but was otherwise normal. A biopsy of 1 of the enlarged nodes was histologically consistent with granulomatous lymphadenitis; all other possible etiologies were ruled out.
Data on Patients Included in the Study.
| Patient | Age | Sex | Past History | Site | Facial Palsy | Fissured Tongue | Onset to Diagnosis, mo | Additional Tests | Histopathology | Treatment | Outcome | Follow-up, y | Subsequent Diagnoses |
| 1 | 49 | Male | None | Upper lip | None | None | 26 | Normal | Histiocytic granulomas | Infiltration of triamcinolone (0.1%) | Improvement | 17 | Carcinoma of the bladder |
| Sulfone | Ischemic heart disease | ||||||||||||
| 2 | 57 | Female | None | Upper lip | None | None | 6 | Normal | Histiocytic granulomas | Unknown | Unknown | 0 | Unknown |
| 3 | 42 | Female | Pregnancy | Upper lip | None | Yes | 12 | Normal | Nonspecific granulomatous inflammation | Oral corticosteroids | Improvement | 14 | Dermatophytosis of the upper lip |
| 4 | 74 | Female | Diabetes mellitus | Upper lip | None | None | 24 | Normal | Epithelioid granulomas | Infiltration of triamcinolone (0.1%) | Improvement | 4 | Leukocytoclastic vasculitis |
| Gums of the upper jaw | Tetracyclines | Cholecystitis | |||||||||||
| 5 | 48 | Male | Lichen planus | Upper lip | None | None | 3 | Normal | Nonspecific granulomatous inflammation | Oral corticosteroids | Improvement | 1 | |
| 6 | 29 | Female | Sensitization | Upper lip | None | None | 24 | Normal | Epithelioid granulomas | Oral corticosteroids | Recurrence | 8 | Hypothyroidism |
| to nickel | Submandibular region | Infiltration of triamcinolone (0.1%) | |||||||||||
| Perioral region | Hydroxychloroquine | ||||||||||||
| Cheeks | Tetracyclines | ||||||||||||
| Antihistamines | |||||||||||||
| Amoxicillin-clavulanic acid |
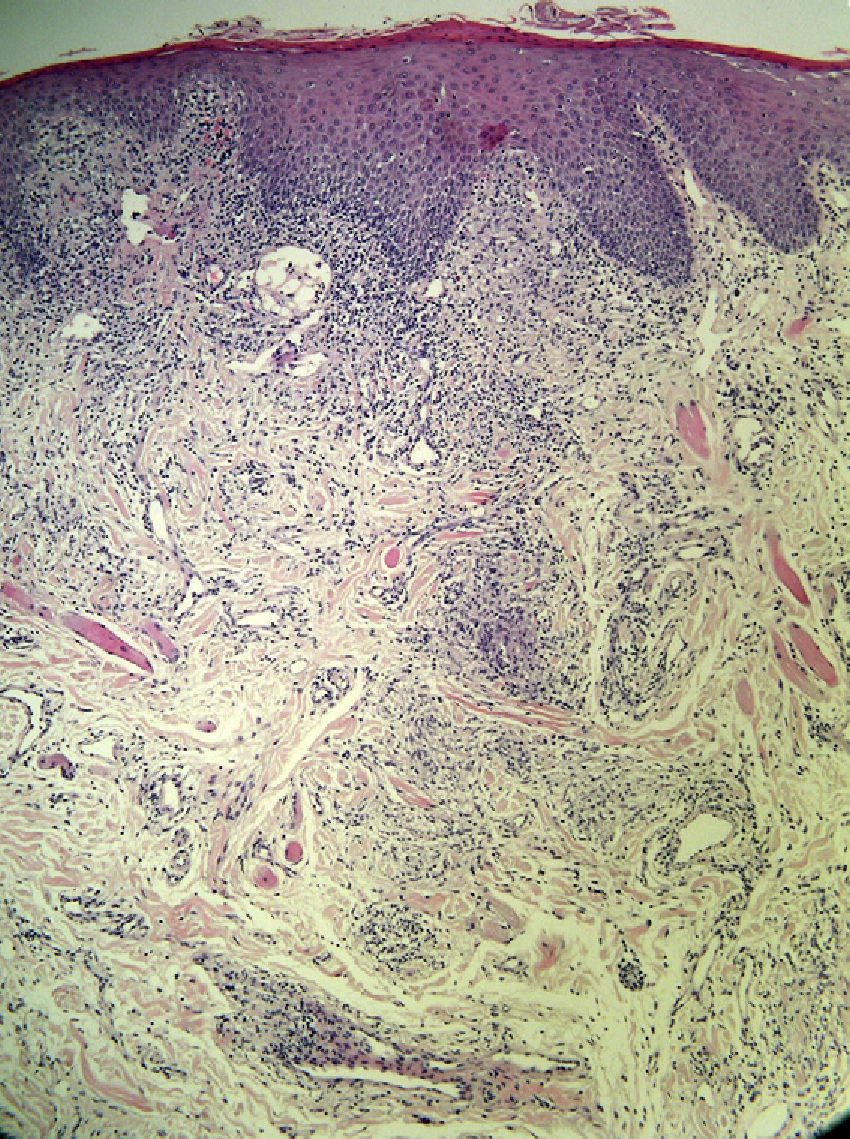
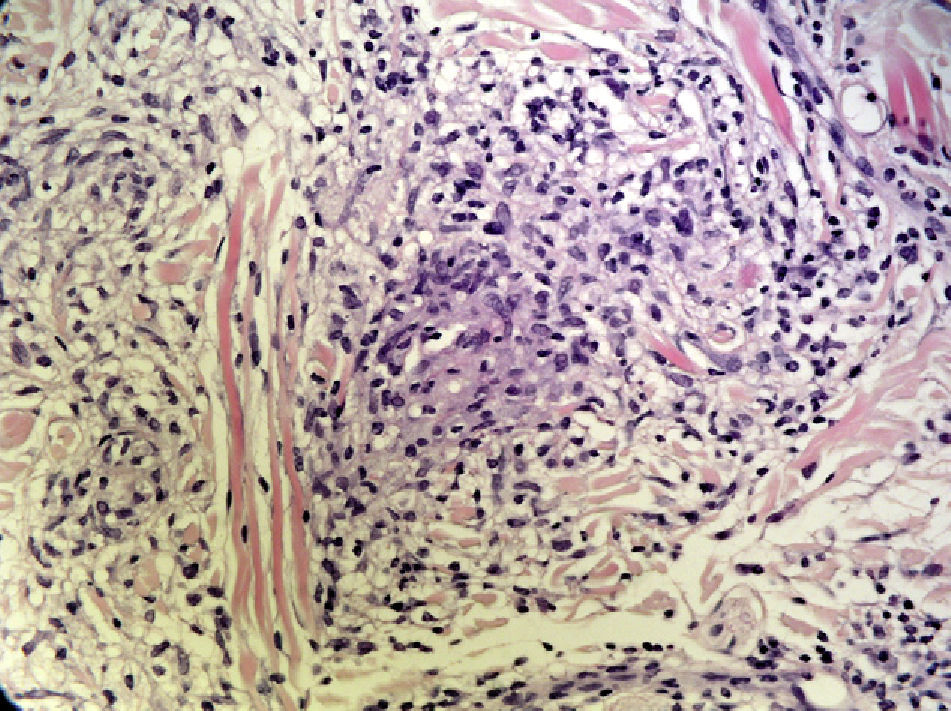
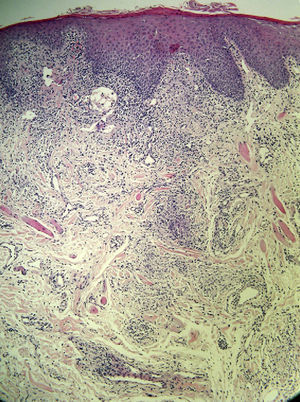
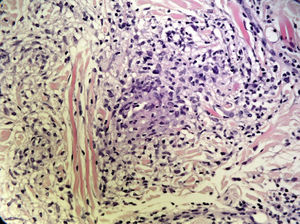
None of the patients had facial palsy, and just 1 (16.66%) had a fissured tongue. In all cases, the clinical diagnosis was followed by a biopsy of the lip; the findings were consistent with granulomatous cheilitis and staining was negative for acid-fast bacilli, fungi, and spirochetes. Granulomatous inflammation (Fig. 5) was observed in 4 patients (66.66%) and nonspecific chronic inflammation (Fig. 6) was observed in 2 patients (33.33%). The patients underwent a chest radiograph, a Mantoux test, serology for hepatitis B and C viruses and human immunodeficiency virus, and laboratory tests including angiotensin-converting enzyme levels, erythrocyte sedimentation rate, and IgA levels; all tests were normal or negative. None of the patients had a family history of labial swelling, a personal history of neurologic, digestive, or respiratory symptoms, or a previous diagnosis of a granulomatous disease. One patient had lichen planus with good symptom control and no oral involvement. Another patient had been diagnosed as a child with allergic contact dermatitis due to nickel salts; however, she denied having had contact with nickel, had no dental implants, and presented no skin lesions. The same patient reported having had recurrent episodes of periodontitis that were treated with antibiotics, were not associated with the exacerbation of granulomatous cheilitis, and did not coincide with flare-ups of the disease. No foci of infection associated with a worsening of the lesions were detected in any of the other cases.
The patients were prescribed different treatments—including infiltration of triamcinolone (0.1%), sulfone, oral corticosteroids, tetracyclines, hydroxychloroquine, and amoxicillin-clavulanic acid—depending on the severity of the manifestations. Improvement was achieved in most of the patients; the manifestations recurred in 1 patient and another patient was lost to follow-up. Excluding the latter patient, the mean follow-up period was 8.8 (6.68) years (range, 1-17 years). None of the patients was diagnosed with Crohn disease or any other granulomatous disease during the follow-up period.
DiscussionMelkersson-Rosenthal syndrome is a systemic granulomatous disease of unknown etiology characterized by the triad of orofacial edema, facial palsy, and fissured (or scrotal) tongue. The complete triad is present in 8% to 25% of patients diagnosed with Melkersson-Rosenthal syndrome, while oligosymptomatic forms of the condition account for 47% of cases. In 28% of cases, orofacial swelling or granulomatous cheilitis is the sole manifestation of the disease. Granulomatous cheilitis is the most common form of presentation of Melkersson-Rosenthal syndrome, observed in 80% of cases.2–5 Five of our patients (83.33%) had a monosymptomatic form of Melkersson-Rosenthal syndrome (granulomatous cheilitis), whereas just 1 patient (16.66%) had an oligosymptomatic form of the condition (swelling of the lips with fissured tongue). None of our patients had the complete form of the syndrome, nor did any of them present evidence of facial palsy or other neurologic signs or symptoms.
The etiology of granulomatous cheilitis is poorly understood but has been associated with genetic,6 allergic,7–12 and infectious13 factors. There are several reports in the literature that associate the pathogenesis of granulomatous cheilitis with odontogenic infection and that describe remission or improvement after treatment of the infection.14–16 In our study, patient 6 was diagnosed with recurrent episodes of odontogenic infection. Although these infections resolved with antibiotic treatment, the patient continued to have acute episodes of granulomatous cheilitis. The same patient showed sensitization to nickel salts, although she had no dental implants and had had no contact with any instruments containing this substance. Both odontogenic infection and nickel sensitization are possible etiologies of the patient's granulomatous cheilitis; however, no temporal or causal relationship supporting either of these hypotheses has yet been established. Various substances including chocolate,11 food additives, cinnamon compounds, and benzoates have been implicated as possible etiologic agents of granulomatous cheilitis; elimination diets have led to improvement in some patients.7,8 Sensitization to metals such as gold and mercury has also been linked to the pathogenesis of the disease.10
Granulomatous cheilitis is a rare disease. Although it can appear at any age, including in childhood,17 it occurs most frequently in the second or third decade of life.18 In our study, the patients were aged between 29 and 74 years. As in previous studies,19–21 there were no childhood cases and a majority of the patients (66.66%) were women. We identified a total of 6 patients with granulomatous cheilitis over a period of 17 years.
Granulomatous cheilitis usually affects the upper lip and, less frequently, the lower lip. However, as was the case in 2 of our patients (33.33%), the disease can also affect other oral and facial regions, including the face, oral mucosa, gums, tongue, pharynx, and larynx.18 The most common presentation is acute, asymptomatic swelling of the lips lasting hours to days. Initially, the episodes of swelling are self-limiting and resolve completely; after several recurring episodes, however, the lips retain some degree of firm, indurated edema. Patients may report pain or a burning sensation, especially if the oral involvement is associated with erythema, fissures, erosions, or scaling of the lips. When other areas of the face are involved, there may be enlarged regional lymph nodes, as occurred in one of our patients.22 None of the patients in our study presented systemic symptoms, although flare-ups of granulomatous cheilitis can be associated with fever and general malaise.18,22
Diagnosis of granulomatous cheilitis is based on clinical findings confirmed by histology. Histopathology reveals nonnecrotizing granulomas, edema, lymphangiectasia, and perivascular lymphocytic infiltration. Noncaseating granulomas are not always present in the dermis, especially in the early stages of granulomatous cheilitis, so their absence does not rule out the condition. Therefore, granulomatous cheilitis is not always associated with specific histological changes.20 The differential diagnosis should include diseases that involve facial edema, conditions caused by granulomas, and, generally, all chronic forms of macrocheilia.
Several studies have linked granulomatous cheilitis to Crohn disease.23,24 In a series of 14 patients with granulomatous cheilitis, an association with Crohn disease was found in 30% of the patients and minor gastrointestinal symptoms without detectable signs of inflammatory bowel disease were found in 43%.23 None of the patients in our study presented gastrointestinal disorders or were diagnosed with Crohn disease during the follow-up period. None of our patients underwent an endoscopic examination because there were no clinical findings to justify such a procedure; the decision not to perform endoscopy was consistent with the recommendations of previous studies.20
The difficulty of managing granulomatous cheilitis is reflected in the variety of treatments that have been used and the lack of consensus regarding the preferred treatment. Moreover, because granulomatous cheilitis is a rare disease, there have been no placebo-controlled studies to evaluate the effectiveness of the various treatments. Combination therapy with intralesional triamcinolone and clofazimine or dapsone is one of the most commonly used treatment options.25,26 Other reported treatments include prednisone, hydroxychloroquine, sulfasalazine,20 antihistamines, tetracyclines,27 metronidazole,28 macrolides,29 thalidomide,30 and infliximab.31 Cheiloplasty is reserved for treatment-resistant cases in which major deformity develops. However, the clinical course and therapeutic response of patients with granulomatous cheilitis are often unpredictable, and spontaneous remissions and recurrences are common. In our series, 4 of the 6 patients (66.66%) responded to medical treatment, 1 patient did not attend subsequent appointments and was lost to follow-up, and the final patient developed recurrence despite the use of various treatment regimens. The most common treatment was intralesional corticosteroids; in cases that required prolonged therapy, however, this treatment was accompanied by other drugs in order to lower the corticosteroid dosage.
Our study has several limitations. The sample of patients was small and the clinical data were reviewed retrospectively; both of these facts may have influenced our results to some extent. Additionally, granulomatous cheilitis may have been underdiagnosed in our study because we only included cases with a clinical and histological diagnosis and excluded patients in whom histologic confirmation was not obtained.
In conclusion, our findings in this study support previous reports that granulomatous cheilitis is an independent entity within the group of orofacial granulomatoses, that it is rare and difficult to diagnose and treat, and that it usually does not present with accompanying signs or symptoms or as part of Melkersson-Rosenthal syndrome. Further research on the pathogenesis of granulomatous cheilitis and clinical trials evaluating the efficacy of the various treatments are needed in order to enhance our understanding of this disease.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez Martínez ML, Azaña-Defez JM, Pérez-García LJ, López-Villaescusa MT, Rodríguez Vázquez M, Faura Berruga C. Queilitis granulomatosa. Presentación de 6 casos y revisión de la literatura. Actas Dermosifiliogr.2012;103:718-724.