Alopecia areata universalis (AAU) is a chronic disease that, not only involves a physical discomfort, but it can also entail a mental health problem due to its relapsing nature and a great impact in self-image. In fact, some studies showed that the likelihood of being attended in mental health services is higher in these patients.1 Moreover, a recent meta-analysis2 found that alexithymia, anxiety and depression are common in patients with AAU, and authors encourage to refer these patients to specialist attention for a better management. Regarding psychological impact, new studies addressed consequences of living with AAU at different levels, such as cognitive (e.g. negative thoughts related to their hair and appearance, hopelessness), emotional (e.g. sadness), and behaviour (e.g. a restricted life as part of social withdrawal).3
Within other countries like UK, collaboration between psychology and dermatology professionals is growing, considering that psychological assessment and treatment should be part of the healthcare of dermatology patients.4 However, despite being the medical assistance of these patients a prevalent phenomenon that greatly impacts our daily clinical practice, very little information is available regarding psychological treatment of these issues. That is, literature is scarce regarding psychological treatments for AAU patients. To our knowledge, this is the first study that have addressed how a cognitive-behavioural therapy, in a psychoeducative group setting, can help in the clinical care of women with AAU.
In order to assess if the usefulness of this psychological intervention in these patients, and to identify key elements that may allow us to improve our quality of assistance in this area, we conducted a pilot study with a group of AAU patients that were followed-up at the Trichology Unit in the Hospital Ramón y Cajal, Madrid. The intervention consisted of nine fortnightly sessions in a psychoeducative group setting. Cognitive-behavioural techniques were used, such as problem-solving, cognitive restructuring, relaxation and social skills. The impact on QoL, sleep, anxiety and alexithymia were measured using validated scales. All statistical analyses were performed using a statistical software package (IBM SPSS Statistics for Macintosh, Version 21.0, released 2012; IBM Corp., Armonk, NY, USA). To study significant difference between after and before intervention t-test and Pearson correlation coefficient were used. All tests were 2-sided and statistical significance was considered with p < 0.05.
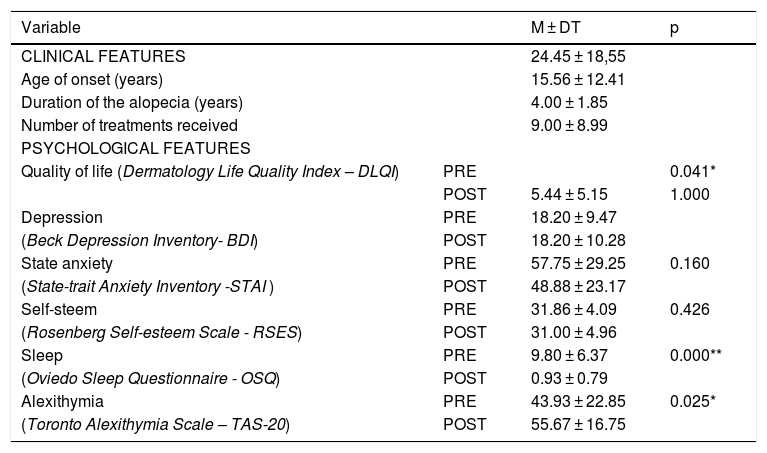
A total of 16 women diagnosed with AAU were included. Their mean age was 45.1 years (range 24-64). Pre-post treatment comparisons are given in Table 1 in more detail. Results showed an improvement in the QoL (p = 0.041) and sleep (p < 0.01), while a paradoxical increase was found in alexithymia (p = 0.025). No other significant differences were found between the beginning and the end of the treatment. Furthermore, correlation tests were conducted between variables. At the beginning, the quality of sleep seemed to be related with anxiety (r = 0.660), depression (r = 0.621) and self-steem (r = 0.580). At the end of treatment, depression was also significantly related with QoL (r = 0.519), whereas anxiety was associated with alexithymia (0.532), as well as with depression (r = 0.599) and self-steem (r= -0.567).
Clinical features and pre-post comparisons in psychological outcome.
| Variable | M ± DT | p | |
|---|---|---|---|
| CLINICAL FEATURES | 24.45 ± 18,55 | ||
| Age of onset (years) | 15.56 ± 12.41 | ||
| Duration of the alopecia (years) | 4.00 ± 1.85 | ||
| Number of treatments received | 9.00 ± 8.99 | ||
| PSYCHOLOGICAL FEATURES | |||
| Quality of life (Dermatology Life Quality Index – DLQI) | PRE | 0.041* | |
| POST | 5.44 ± 5.15 | 1.000 | |
| Depression | PRE | 18.20 ± 9.47 | |
| (Beck Depression Inventory- BDI) | POST | 18.20 ± 10.28 | |
| State anxiety | PRE | 57.75 ± 29.25 | 0.160 |
| (State-trait Anxiety Inventory -STAI ) | POST | 48.88 ± 23.17 | |
| Self-steem | PRE | 31.86 ± 4.09 | 0.426 |
| (Rosenberg Self-esteem Scale - RSES) | POST | 31.00 ± 4.96 | |
| Sleep | PRE | 9.80 ± 6.37 | 0.000** |
| (Oviedo Sleep Questionnaire - OSQ) | POST | 0.93 ± 0.79 | |
| Alexithymia | PRE | 43.93 ± 22.85 | 0.025* |
| (Toronto Alexithymia Scale – TAS-20) | POST | 55.67 ± 16.75 |
*p < 0.05; **p < 0.01.
These results have several implications. Firstly, the psychological intervention seems to be effective to improve QoL and sleep in women with AA, which are basic for the well-being of our patients. Some authors stated that patients with AAU have multiple risk factors for mental health disorders,5 such as psychological distress and a significant degree of impairment in quality of life (QoL. Despite more research is needed to thoroughly study the association between QoL, sleep quality and well-being in AAU patients, it suggests that it is strongly encouraged to bear these variables in mind when treating patients with AAU.The psychologist’s role in AAU patients is to improve the availability and use of personal resources and abilities to cope with their distress, improving their personal, social and family quality of life.6 Furhermore, additional measures such as IPDE might be useful to discriminate personality profiles that are associated with QoL and clinical course in AAU.7
Secondly, a modest improvement was observed in anxiety, despite not being significant, which might be explained for the little sample size and the restricted period of time. Some improvements such as quality of sleep of little details regarding QoL in AA patients are easier to achieve faster than others which are more complex, such as anxiety or depression, which often need more than a few weeks to change.
Finally, regarding the paradoxical increase found in alexithymia, it might be part of the process of starting to recognize self-emotions. Some patients may be still confused about emotions, while others already know how to identify them, how they feel but not how to express it. Future studies may shed light in this issue.
Some limitations must be noted. Our sample is exclusively composed of women, so results cannot be generalized to male AAU patients and the sample size is very limited.
In conclusion, our preliminar results show the positive impact of psychological interventions to improve AAU patients’ QoL. It supports the collaboration between psychologists and dermatologists to improve clinical management of dermatological disease. These data will be useful for future studies regarding the impact of psychological intervention in patients with alopecia areata.
We would like to acknowledge patient’s participation in this study, as well as some professionals from our departments who helped us in the present study.
Please cite this article as: Pascual-Sánchez A, Fernández-Martín P, Saceda-Corralo D, Vañó-Galván S. Impacto de la intervención psicológica en mujeres con alopecia areata universal: un estudio piloto. An Pediatr (Barc).2020. https://doi.org/10.1016/j.anpedi.2020.05.006