We present the case of a 10-month old girl with a painless subcutaneous tumor on the mons veneris and labia majora. The lesion had not been present at birth and had been noticed by the girl's parents several weeks before consultation.
Physical ExaminationClinically, the lesion was a firm, poorly circumscribed subcutaneous nodular tumor localized in the genital region. It was more palpable than visible (Fig. 1). No other lesions, similar or otherwise, were detected elsewhere on the body. The girl was in good health and her development was normal for her age.
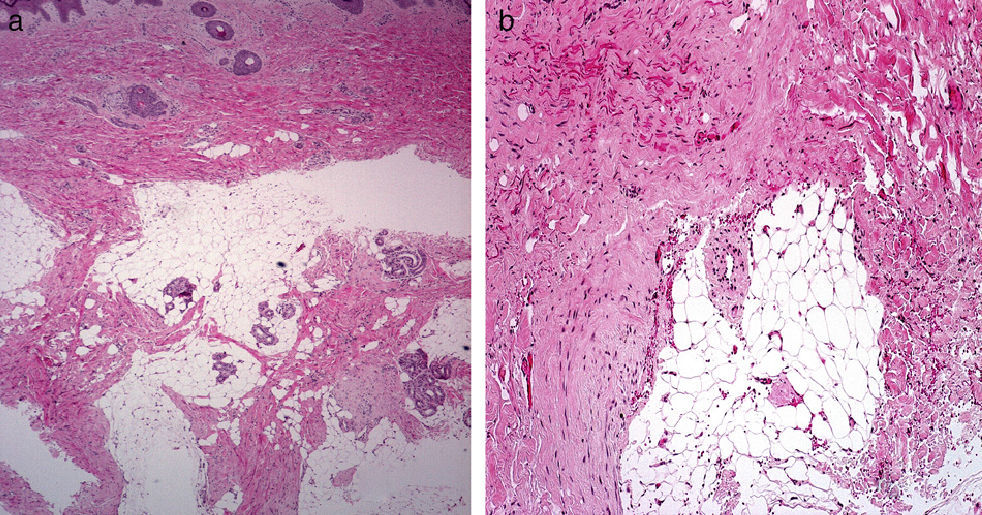
HistopathologyHistologic examination of the lesion showed a proliferation of fibrous tissue in the deep dermis and subcutaneous tissue interspersed with lobules of mature adipose tissue. Examination under higher magnification showed how the fibrous tissue was organized into bands of fibrosis with a moderate number of spindle cells that resembled immature fibroblasts (Figs. 2A and B).
Additional TestsMagnetic resonance imaging of the pelvis showed a tumor on the anterior portion of both labia majora and on the mons veneris, predominantly affecting the subcutaneous tissue; there was no enhancement with the administration of contrast material. The staging study (bone scan, chest radiograph, echocardiogram, and abdominal ultrasound) showed no other alterations.
What Is Your Diagnosis?
DiagnosisLipofibromatosis.
Clinical Course and TreatmentBecause of the size and location of the lesion, it was decided to adopt a watch and wait approach. A year after diagnosis, the lesion was less noticeable and showed signs of spontaneous regression, although a slightly hardened area was still palpable in the area of the mons veneris.
CommentLipofibromatosis is an uncommon benign lesion that was first described by Fetsch et al.1in 2000 and recognized as an independent fibrofatty tumor of childhood in the World Health Organization Classification of Tumours in 2002.2
The tumor is exclusive to children and is sometimes congenital. It presents as a poorly circumscribed subcutaneous mass measuring a few centimeters that grows slowly and painlessly. The hands and feet are the most common sites affected.1,3 Tumors in the genital region, such as that described in our patient, are very rare. Histologically, the lesion consists of a poorly circumscribed mass with alternating streaks of adipose tissue consisting of mature adipocytes, with bands of fibrosis formed by abundant spindle cells resembling immature fibroblasts. These fibrous bands and spindle cells replace the connective tissue septa of the hypodermis. Adipose tissue can account for over 70% of the tumor.2,4 The tumor is similar to fibrous hamartoma of infancy but it lacks the islands of immature oval cells immersed in a myxoid stroma. Mitotic figures are scarce and cellular atypia is not observed. Intermediate cells containing lipid vacuoles in their cytoplasm may be observed in the interface between the fascicles of spindle cells and mature adipocytes.1,5
Spindle cells are focally and variably immunoreactive to CD34, bcl-2, S-100 protein, smooth muscle actin, and epithelial membrane actin. CD99 positivity may be occasionally observed. Immunostains for desmin and cytokeratin are negative.1,2,5,6
The differential diagnosis of lipofibromatosis includes fibrous hamartoma of infancy, calcifying aponeurotic fibroma, lipoblastoma, and fibrolipoma.
The tumor is poorly circumscribed and recurrence is common due to the difficulty of achieving complete surgical resection. However, there have been no reports of metastasis or malignant transformation.
Complete excision is the treatment of choice, particularly if the operation can be performed with minimal morbidity. However, patients with a risk of considerable functional impairment following complete excision should be managed on a case-by-case basis, as there have been reports of patients with incompletely excised tumors not experiencing recurrence during long-term follow-up. Recurrence appears to be more common in boys, congenital tumors, tumors on the hands or feet, incompletely excised tumors, and tumors with mitotic figures in the spindle cell component.1,5
Please cite this article as: Bernat García J, Fuertes Prosper A, Marti Ibor E. Lactante con tumoración subcutánea en el área genital. Actas Dermosifiliogr. 2014;105:619–620.