Renal transplant recipients (RTR), which are an increasing population, frequently suffer from post-transplant dermatological complications. Despite the well-established role of dermatologists in the outpatient care of these patients, no previous studies were found concerning dermatology consultations for hospitalized RTR.
ObjectivesTo investigate the epidemiology of dermatological conditions presented by RTR during hospitalization and assess the impact of dermatology consultations performed in the hospital setting.
MethodsDermatology consultations requested for RTR admitted at a kidney transplantation referral hospital in Brazil over 36 consecutive months were retrospectively included.
Results176 consultations were included. Infectious dermatoses prevailed (52.3%), followed by inflammatory diseases (14.2%), neoplasms (12.5%) and drug reactions (8.5%). Diagnostic agreement between requesting and consulting teams was 38.1%. Most consultations were motivated by common dermatological conditions, unrelated to admission diagnosis. There were some differences in comparison to previous studies including general inpatients, such as: larger proportion of infectious dermatoses and neoplasms, smaller proportion of inflammatory diseases, higher percentage of patients submitted to skin biopsy, smaller proportion of consultations managed with a single visit and higher probability of a systemic treatment being recommended in this population.
ConclusionHospitalized RTR present distinct dermatological epidemiology and higher level of complexity, when compared to studies including general inpatients. Dermatology interventions during hospitalization may be beneficial in the multidisciplinary care of these patients, either contributing to the investigation of systemic conditions or providing relief for cutaneous comorbidities.
El número de pacientes receptores de trasplante renal (RTR) está en aumento, y estos con frecuencia, además presentarán complicaciones dermatológicas derivadas del trasplante. Si bien el rol del dermatólogo a nivel de la consulta ambulatoria está establecido, no encontramos ningún estudio acerca de interconsultas dermatológicas en pacientes RTR hospitalizados.
ObjetivosLa finalidad de este estudio fue determinar las características epidemiológicas de las enfermedades dermatológicas que afectan a los pacientes RTR hospitalizados, así como valorar el impacto que tienen las interconsultas dermatológicas durante el ingreso hospitalario de estos pacientes.
MétodosDurante un periodo de 36 meses consecutivos, se incluyeron de forma retrospectiva las consultas realizadas al servicio de dermatología en pacientes RTR ingresados en un hospital de referencia en trasplantes renales de Brasil.
ResultadosSe incluyeron 176 interconsultas. Las dermatosis infecciosas fueron las más prevalentes (52,3%), seguidas de las enfermedades inflamatorias (14,2%), neoplasias (12,5%) y reacciones medicamentosas (8,5%). La concordancia diagnóstica entre el diagnóstico de derivación y el diagnóstico final fue del 38,1%. La mayoría de las interconsultas se debieron a condiciones dermatológicas comunes que no guardaban relación con el motivo de ingreso. Se evidenciaron algunas diferencias con estudios previos en pacientes ingresados en hopitales generales; por ejemplo, en los pacientes RTR hubo una mayor proporción de dermatosis infecciosas y neoplasias y una menor proporción de enfermedades inflamatorias. Así mismo un mayor porcentaje de biopsias cutáneas fueron realizadas, una mayor proporción de interconsultas requirieron más de una visita y hubo la necesidad de pautar tratamiento sistémico en un mayor número de pacientes.
ConclusiónLos pacientes RTR ingresados presentaron características epidemiológicas diferentes, así como un mayor nivel de complejidad clínica en comparación con con estudios realizados en hospitales generales. Concluimos que la colaboración del servicio de dermatología durante el ingreso será beneficiosa en el manejo multidisciplinario de estos pacientes, ya que ayudará en el estudio de las enfermedades sistémicas, así como a tratar comorbilidades cutáneas.
Brazil coordinates the largest public transplantation program worldwide. Over 8,000 solid organ transplants (SOT) are performed every year, more than 90% of these under government funding.1 The number of kidney transplants has reached 5556 in 2015.2 Considering the rise in number of transplantations performed as well as in long-term survival of SOT recipients, there is an emerging demand for multidisciplinary post-transplant care.
Dermatological problems related to chronic immunosuppression are frequent among renal transplant recipients (RTR). There is a well-established role for dermatologists in the outpatient care of these individuals,3–5 who have a highly-increased risk (65- to 250-fold) of non-melanoma skin cancer (NMSC), when compared to the general population.3 However, we were unable to find studies specifically about cutaneous comorbidities and complications presented by SOT or RTR during hospitalization and requiring inpatient dermatology consultation.
Despite frequently overlooked, dermatological abnormalities are highly prevalent in the hospital setting and may represent cutaneous findings of systemic diseases.6 Economical and practice constraints have pushed dermatologists almost completely out of the hospital, so that the care of hospitalized patients with skin conditions has widely been shifted to non-dermatologist physicians.6–8 Time dedicated to teaching dermatology in medical schools is frequently limited. Not surprisingly, many general practitioners and other specialists feel unprepared to address even common dermatologic complaints.9,10 These facts may increase the need for inpatient dermatology consultations and its potential relevance, especially in units that frequently admit high-complexity patients like SOT recipients.
The aim of this study was to describe dermatological conditions presented by RTR during hospitalization; analyze the epidemiology and level of complexity of the cases in comparison to the literature and assess the impact of the consultations performed by dermatologists.
Materials and MethodsThis is an observational, retrospective and descriptive study. All dermatology consultations requested for RTR at a Brazilian kidney transplantation referral hospital (Hospital do Rim - hrim) over 36 consecutive months were included. Data were retrieved from an electronic database, which had been prospectively loaded during assessments, and complemented by information from patient's charts. Institutional ethics committee approval was obtained.
Hrim is a tertiary hospital located in Sao Paulo where more than 11,000 kidney transplants have been performed over the last 18 years.1 The institution is a partner of Universidade Federal de São Paulo (UNIFESP) and has 146 beds available, sixteen of these in the intensive care unit (ICU). Inpatients at hrim referred to dermatology are evaluated by consultants from UNIFESP Department of Dermatology within 48hours of the request.
Clinical and epidemiological characteristics of the patients, specificities of the dermatological complaints, dermatology-specific procedures, number of visits needed, final diagnoses and treatment recommendations were assessed. Provisional diagnoses provided by requesting team were compared with final dermatology diagnoses. Impact and relevance of the consultations were also analyzed using a previously published model.11 Data were compared with the literature concerning dermatology consultations in general hospitals.
This was an essentially descriptive study. For quantitative variables, mean, median and standard-deviation were calculated. Qualitative variables were analyzed with absolute and relative frequencies (percentage). When applicable, statistical tests (chi-square and non-parametric Mann-Whitney tests) were used. The significance level was established at P <0.05.
ResultsOver the 36-months period reviewed, 28,596 patients were admitted to hrim and 76.7% of these were RTR. Most hospitalizations (80.7%) had government funding. Dermatology consultation was required for 176 RTR, representing 0.62% of the hospital admissions. On average, five new requests were received per month, ranging from one to 14.
Among the 176 RTR included in this study, main reason for hospitalization were infectious diseases (58%), associated or not with graft disfunction, in particular infections of the lower respiratory tract, urinary tract, skin and soft tissues and cytomegalovirus disseminated infection. The dermatological condition which motivated the consultation request was the reason for hospital admission or was related to it in 21.6% and 33.5% of the cases, respectively.
Concerning demographic characteristics of the patients included, deceased donor (68.8%), male gender (64.2%) and young age (46.9 ± 15.6 years) predominated. The proportion of individuals aged 60 years or more was 22.7%. Transplant length was 56.14 ± 57.33 months.
Immunosuppression regimen was heterogeneous. Almost half of the patients (49.4%) were under classical triple-drug therapy (association of calcineurin inhibitor, antiproliferative agent and corticosteroid). The commonest combination was tacrolimus, mycophenolate sodium and prednisone (31.8%), followed by tacrolimus, azathioprine and prednisone (14.2%). A mammalian target of rapamycin inhibitor was part of the prescription in the minority (14.2%). The remaining patients (36.4%) were under reduced regimens, with calcineurin inhibitor and/or antiproliferative agent withdrawn due to side effects or severe infectious/oncologic complications whose treatment was prioritized over graft survival. Considerable heterogeneity concerning immunosuppressive regimen observed in this sample precluded correlations between dermatological diagnoses and drug regimens.
Mean elapsed time between hospital admission and consultation request was 13 ± 19.5 days, ranging from one to 156 days. When the dermatological problem was the cause for hospitalization, this interval was significantly shorter (5.9 ± 6.9 days) (P <0.001).
More frequently, dermatological complaint had arisen before admission (71.6%) and had been present for 30 days or less (59.7%). Chronic conditions, lasting more than 12 months were responsible for 14.2% of the requests.
Dermatological diagnosis was provided solely on clinical basis, without the need for diagnostic tests, in 45.5% of the consultations. A skin biopsy was performed in 40.3%, for histological, microbiological (staining and cultures) and/or molecular analysis. In 78.9% of the biopsied cases, the histopathological and/or microbiological findings from the specimen contributed to the final diagnosis, by confirming main clinical hypothesis or helping to exclude differential diagnoses. In the remaining ones (15/71; 21.1%), the findings were nonspecific, not conclusive or incompatible with clinical presentation. Consultants also performed a Tzanck smear for 7.4% of the patients and skin scrapings for direct mycology for 6.8%.
Tissue cultures resulted positive for bacteria in 50% of 24 skin biopsies, however, 66.7% of these (8/12) were considered false-positive or contaminants, whereas fungi had grown in 9 (31%) cultured fragments and 22.2% (2/9) of these were considered false-positives. No tissue cultures resulted positive for mycobacteria, even in one case of probable cutaneous tuberculosis secondary to hematogenic dissemination presenting acid-alcohol resistant bacilli on Ziehl-Neelsen stain in skin tissue.
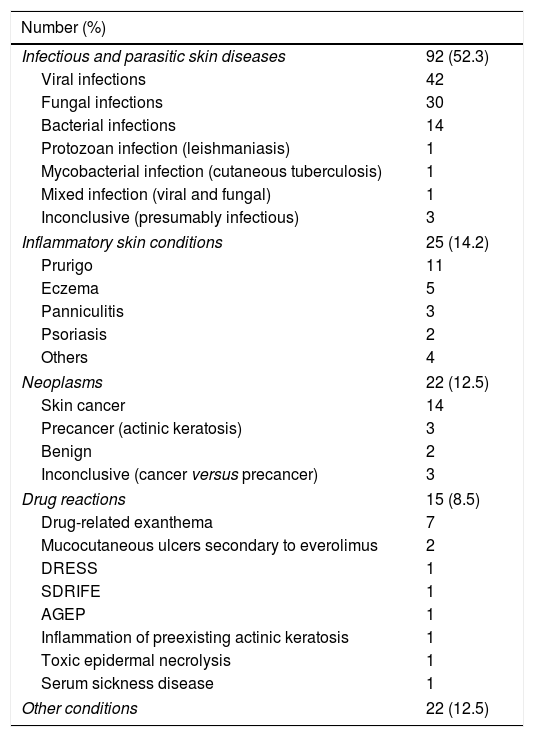
Concerning final dermatological diagnoses, infectious dermatoses predominated (52.3%), followed by inflammatory skin conditions (14.2%), neoplasms (12.5%) and drug reactions (8.5%). Herpes simplex infection, dermatophytosis, prurigo, erysipela/cellulitis, squamous cell carcinoma and drug-related exanthema were the commonest diagnoses, which altogether accounted for 39.8% of the consultations. Table 1 shows the complete distribution of diagnoses.
Dermatological diagnoses.
| Number (%) | |
|---|---|
| Infectious and parasitic skin diseases | 92 (52.3) |
| Viral infections | 42 |
| Fungal infections | 30 |
| Bacterial infections | 14 |
| Protozoan infection (leishmaniasis) | 1 |
| Mycobacterial infection (cutaneous tuberculosis) | 1 |
| Mixed infection (viral and fungal) | 1 |
| Inconclusive (presumably infectious) | 3 |
| Inflammatory skin conditions | 25 (14.2) |
| Prurigo | 11 |
| Eczema | 5 |
| Panniculitis | 3 |
| Psoriasis | 2 |
| Others | 4 |
| Neoplasms | 22 (12.5) |
| Skin cancer | 14 |
| Precancer (actinic keratosis) | 3 |
| Benign | 2 |
| Inconclusive (cancer versus precancer) | 3 |
| Drug reactions | 15 (8.5) |
| Drug-related exanthema | 7 |
| Mucocutaneous ulcers secondary to everolimus | 2 |
| DRESS | 1 |
| SDRIFE | 1 |
| AGEP | 1 |
| Inflammation of preexisting actinic keratosis | 1 |
| Toxic epidermal necrolysis | 1 |
| Serum sickness disease | 1 |
| Other conditions | 22 (12.5) |
DRESS, drug reaction with eosinophilia and systemic symptoms; SDRIFE, symmetrical drug related intertriginous and flexural exanthema; AGEP, acute generalized exanthematous pustulosis.
A single visit was enough for concluding patient assessment in 43.8% of the consultations. On average 2 ± 1.39 visits per patient were needed, ranging from one to 13. A higher number of visits was necessary when the dermatological complaint was the reason for admission (P=0.024) and for patients submitted to skin biopsy (P <0.001).
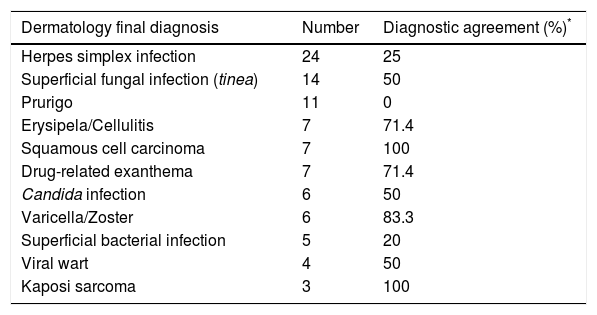
The requesting team provided diagnostic hypothesis for the dermatological condition in 63.1% of the requests and 60.4% of these were compatible with final dermatology diagnosis. When a diagnostic hypothesis was not presented, the diagnosis was presumed to be unknown. Therefore, the diagnostic agreement between requesting and consulting teams was 38.1%, with considerable variation according to specific diseases (Table 2).
Diagnostic agreement according to dermatological diagnosis (only most frequent diagnoses included).
| Dermatology final diagnosis | Number | Diagnostic agreement (%)* |
|---|---|---|
| Herpes simplex infection | 24 | 25 |
| Superficial fungal infection (tinea) | 14 | 50 |
| Prurigo | 11 | 0 |
| Erysipela/Cellulitis | 7 | 71.4 |
| Squamous cell carcinoma | 7 | 100 |
| Drug-related exanthema | 7 | 71.4 |
| Candida infection | 6 | 50 |
| Varicella/Zoster | 6 | 83.3 |
| Superficial bacterial infection | 5 | 20 |
| Viral wart | 4 | 50 |
| Kaposi sarcoma | 3 | 100 |
Consultation changed admission diagnosis in 11.4% of the cases. In 42%, the requesting team had started treatment for the skin condition prior to the consultation. In 40.5% of these and in 52% of the remaining cases, a therapeutic change was suggested by consultants. Hence, in 52.8% of the consultations, dermatologists did not suggest therapeutic measures for the skin condition during hospitalization or the treatment initiated by requesting physicians was unchanged.
A systemic medication, associated or not with topical agents, was necessary for the treatment of the dermatological problem in 45.5% of the cases.
Dermatological outpatient follow-up was recommended in 35.8% of the consultations. Average length of hospital stay was 26.2 ± 27.2 days, ranging from one to 213 days, which was considerably superior than average length of stay for total hospital admissions at hrim (4.96 days). Twelve deaths (6.8%) occurred, none of these directly related to dermatological conditions.
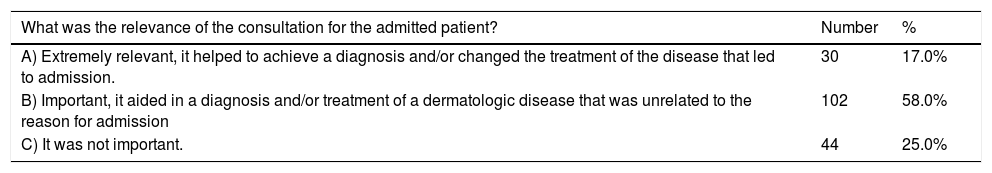
Two multiple-choice questions, extracted from previous publication,16 were used to evaluate the impact of consultations (Table 3).
Assessment of the relevance and impact of dermatology consultations.
| What was the relevance of the consultation for the admitted patient? | Number | % |
|---|---|---|
| A) Extremely relevant, it helped to achieve a diagnosis and/or changed the treatment of the disease that led to admission. | 30 | 17.0% |
| B) Important, it aided in a diagnosis and/or treatment of a dermatologic disease that was unrelated to the reason for admission | 102 | 58.0% |
| C) It was not important. | 44 | 25.0% |
| Would patient treatment be negatively impacted if there was no dermatological consultation available? | Number | % |
|---|---|---|
| A) Yes, a systemic disease would not have been diagnosed or a potentially severe dermatologic disease would not have been treated. | 31 | 17.6% |
| B) Slightly, the patient would have suffered longer with the dermatologic complaint until an outpatient consultation was available. | 80 | 45.5% |
| C) No, there was no need for an emergency dermatologic consultation, or the dermatologic consultation did not modify the treatment. | 65 | 36.9% |
The following variables were statistically associated with consultations of higher relevance (P <0.001): dermatological complaint being the cause of hospital admission or being related to it and dermatological complaint arising prior to hospital admission. Complaints lasting more than 30 days (P=0.023) and localized cutaneous lesions (P=0.014) were significantly more associated with consultations regarded as “not important”, than acute/subacute complaints and disseminates lesions, respectively.
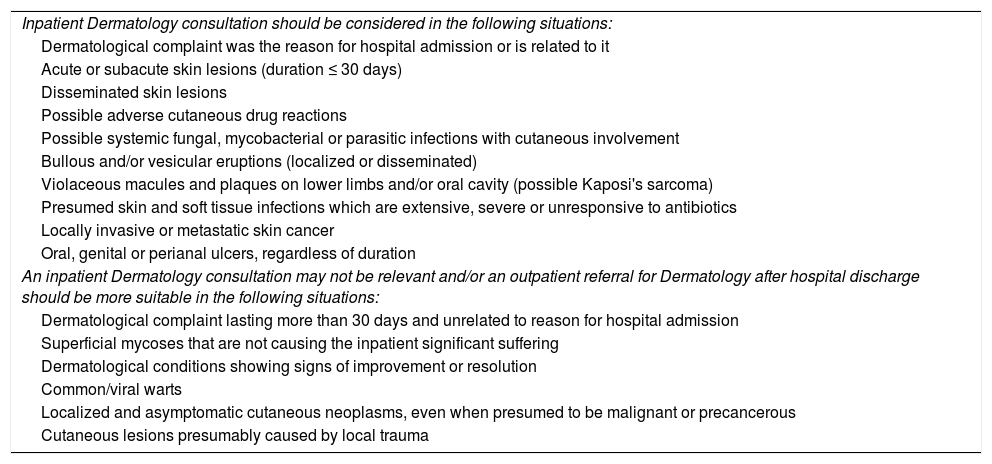
Statistical and subjective analysis of consultations allowed the authors to suggest some criteria that may help non-dermatologist physicians to decide on whether or not a consultation should be requested during hospitalization (Table 4), especially when assisting immunocompromised individuals.
Suggested criteria for helping non-dermatologist physicians deciding whether or not a dermatology inpatient consultation should be requested.
| Inpatient Dermatology consultation should be considered in the following situations: |
| Dermatological complaint was the reason for hospital admission or is related to it |
| Acute or subacute skin lesions (duration ≤ 30 days) |
| Disseminated skin lesions |
| Possible adverse cutaneous drug reactions |
| Possible systemic fungal, mycobacterial or parasitic infections with cutaneous involvement |
| Bullous and/or vesicular eruptions (localized or disseminated) |
| Violaceous macules and plaques on lower limbs and/or oral cavity (possible Kaposi's sarcoma) |
| Presumed skin and soft tissue infections which are extensive, severe or unresponsive to antibiotics |
| Locally invasive or metastatic skin cancer |
| Oral, genital or perianal ulcers, regardless of duration |
| An inpatient Dermatology consultation may not be relevant and/or an outpatient referral for Dermatology after hospital discharge should be more suitable in the following situations: |
| Dermatological complaint lasting more than 30 days and unrelated to reason for hospital admission |
| Superficial mycoses that are not causing the inpatient significant suffering |
| Dermatological conditions showing signs of improvement or resolution |
| Common/viral warts |
| Localized and asymptomatic cutaneous neoplasms, even when presumed to be malignant or precancerous |
| Cutaneous lesions presumably caused by local trauma |
Epidemiology of the consulted patients, such as predominance of male gender, deceased donor and young age, reflects the epidemiology of individuals submitted to kidney transplantation at hrim,15 who represent the majority of inpatients admitted to the hospital.
Average age and proportion of individuals over 60-years old were both inferior than the observed in previous studies concerning dermatology consultations for general inpatients.10,12,13,16,17 The relatively young age of RTR admitted to hrim reflect two facts: the average age at transplantation - 36.1 years for patients with related living donors and 40.5 years for patients with deceased donors15 - and long-term survival of transplant recipients, which, despite significant increase in recent years, is still shorter than general population.1,15
The interval between hospital admission and consultation can be considered long, since most dermatological complaints had arisen prior to hospitalization. Even when the dermatological condition was the reason for admission, the interval, despite shorter, was not ideal. In these cases, when dermatological consultation has a higher potential of leading to relevant diagnostic and therapeutic changes, the request should be made as early as possible, preferably in the first 24-48hours after admission. It is important for dermatologist consultants to examine recent lesions, not yet modified by therapy.
Acute/subacute dermatological complaints prevailed in this sample and were associated with more relevant consultations. It can be proposed, therefore, that a predominance of acute/subacute dermatological conditions can be a suitable parameter for evaluating the quality of dermatology inpatient consultations and the suitability of the requests.
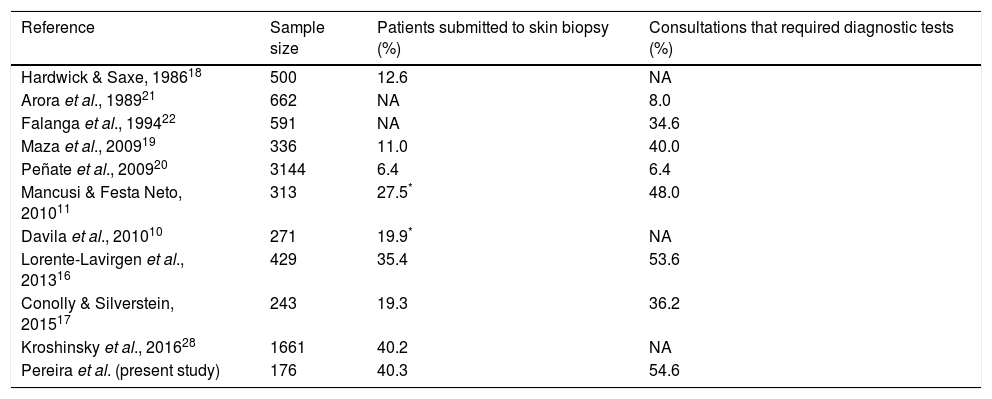
Comparing to other studies including general inpatients (Table 5), there was a higher percentage of patients submitted to skin biopsy11,16–20 and that demanded any diagnostic test11,16,17,19–22 in our population. This finding may suggest that dermatological conditions evaluated at hrim could have a higher level of complexity. However, it should be taken into account that the number of tests requested usually varies among different consultants, even for similar problems, and tend to be higher in teaching hospitals.
Literature review concerning skin biopsies and diagnostic tests needed for inpatient dermatology consultations in general hospitals, comparing to the present study.
| Reference | Sample size | Patients submitted to skin biopsy (%) | Consultations that required diagnostic tests (%) |
|---|---|---|---|
| Hardwick & Saxe, 198618 | 500 | 12.6 | NA |
| Arora et al., 198921 | 662 | NA | 8.0 |
| Falanga et al., 199422 | 591 | NA | 34.6 |
| Maza et al., 200919 | 336 | 11.0 | 40.0 |
| Peñate et al., 200920 | 3144 | 6.4 | 6.4 |
| Mancusi & Festa Neto, 201011 | 313 | 27.5* | 48.0 |
| Davila et al., 201010 | 271 | 19.9* | NA |
| Lorente-Lavirgen et al., 201316 | 429 | 35.4 | 53.6 |
| Conolly & Silverstein, 201517 | 243 | 19.3 | 36.2 |
| Kroshinsky et al., 201628 | 1661 | 40.2 | NA |
| Pereira et al. (present study) | 176 | 40.3 | 54.6 |
NA: not available.
Microbiological accuracy of cultured skin tissue fragments is widely known to be low, with disappointing sensibility and high rates of false-positives.23,24 In spite of that, the Infectious Disease Society of America strongly recommends early biopsy or aspiration of the lesion for histological and microbiological evaluation of skin and soft tissue infections in immunocompromised individuals.25 In such patients, under risk of opportunistic and uncommon infections, clinical-histological-microbiological correlation is crucial for obtaining a more precise etiological diagnosis and appropriate treatment.26
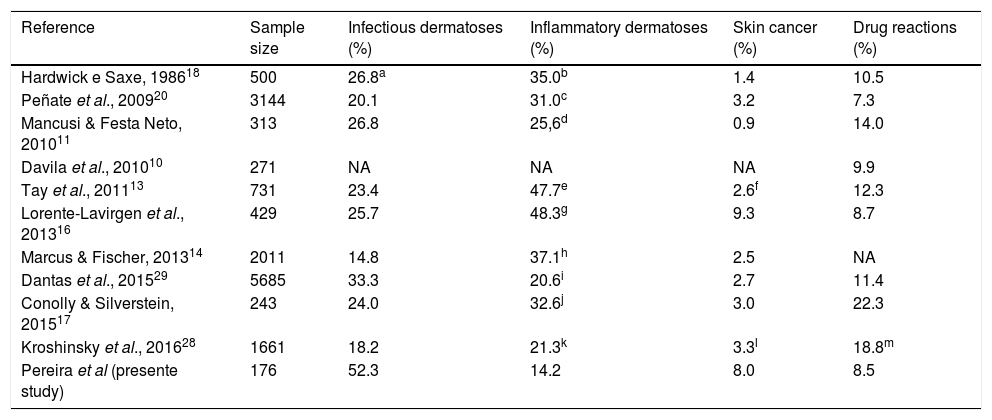
Classification of dermatologic diagnoses was considerably heterogenous among previous studies addressing inpatient dermatology consultations. When enough data were available, diagnoses were regrouped for some of these studies, using the same main categories as ours, what made comparisons feasible (Table 6). In general, a larger proportion of infectious dermatoses and malignancies, and a lower proportion of inflammatory diseases was observed in this sample, when compared to general inpatients. The proportion of requests motivated by cutaneous adverse drug reactions was somewhat similar to other studies.
Literature review concerning dermatological diagnosis categories in general hospitals comparing to the present study.
| Reference | Sample size | Infectious dermatoses (%) | Inflammatory dermatoses (%) | Skin cancer (%) | Drug reactions (%) |
|---|---|---|---|---|---|
| Hardwick e Saxe, 198618 | 500 | 26.8a | 35.0b | 1.4 | 10.5 |
| Peñate et al., 200920 | 3144 | 20.1 | 31.0c | 3.2 | 7.3 |
| Mancusi & Festa Neto, 201011 | 313 | 26.8 | 25,6d | 0.9 | 14.0 |
| Davila et al., 201010 | 271 | NA | NA | NA | 9.9 |
| Tay et al., 201113 | 731 | 23.4 | 47.7e | 2.6f | 12.3 |
| Lorente-Lavirgen et al., 201316 | 429 | 25.7 | 48.3g | 9.3 | 8.7 |
| Marcus & Fischer, 201314 | 2011 | 14.8 | 37.1h | 2.5 | NA |
| Dantas et al., 201529 | 5685 | 33.3 | 20.6i | 2.7 | 11.4 |
| Conolly & Silverstein, 201517 | 243 | 24.0 | 32.6j | 3.0 | 22.3 |
| Kroshinsky et al., 201628 | 1661 | 18.2 | 21.3k | 3.3l | 18.8m |
| Pereira et al (presente study) | 176 | 52.3 | 14.2 | 8.0 | 8.5 |
NA: not available.
Including dermatitis, psoriasis, urticaria (not clearly drug induced) and inflammatory conditions classified as “skin signs of systemic diseases”;
Including urticaria, diseases of musculoskeletal and connective tissue and inflammatory disorders, except drug reactions;
Including eczema/dermatitis, connective tissue disorders/vasculitis; urticaria/angioedema, psoriasis and immunobullous disorders;
Including inflammatory skin conditions, stasis dermatitis, vasculitis, autoimmune and bullous skin conditions, hidradenitis suppurativa and pyoderma gangrenosum;
The proportion of consultations managed with a single visit, was inferior to that observed by the majority of similar studies, involving general inpatients,11,16,17,20,27 what may also suggest a higher level of complexity in our population. However, once again, an academic/pedagogic bias, as well as consultant personality, may influence the decision to follow or not the inpatient.
Previous studies have also found low rates of diagnostic agreement between requesting physicians and dermatology consulting teams, ranging from 23.9% to 48.9%.10,17,22,28 However, the number of misdiagnosis may be inflated by the fact that, when a diagnostic hypothesis is not provided by requesting team, it accounts as diagnostic disagreement. Perhaps, if actively enquired, these physicians may probably provide correct answers for at least some of these presumed “misdiagnoses”.
The proportion of patients that required systemic treatment for the dermatological condition (45.5%) was higher in this study, when compared to the literature (19.1-31.3%),10,16,17,19 what may, once more, be an indicative of higher complexity.
In our sample, patients were more frequently advised to attend a follow-up dermatology visit after discharge, when compared to other studies.11,16,20 Facilitated access of discharged patients to outpatient dermatology follow-up are of major importance for the adequate functioning of an inpatient consultation service.
In conclusion, the findings suggest that consultations for hospitalized RTR may present with distinct epidemiology and, probably, a higher level of complexity of dermatological conditions, when compared to general inpatients. Most consultations were motivated by common dermatologic conditions, unrelated to admission diagnosis. However, the specificities and complexity of the inpatients, as well as the low proportion of diagnostic agreement between requesting and consulting teams, justify the need for dermatology consultants in high-complexity hospitals, such as hrim.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Coordination for the Improvement of Higher Education Personnel (CAPES), Brazil, for providing a scholarship for the first author.
Please cite this article as: Pereira AR, Porro AM, Seque CA, Pasin VP, Tomimori J. Interconsulta hospitalaria en dermatología en una unidad de transplante renal. Actas Dermosifiliogr. 2018;109:900–907.