While graft-vs-host disease (GVHD) is a common complication in bone marrow transplantation, it is rare in liver transplantation, with an estimated incidence of around 1% or 2%.1 Since GVHD was first described in a liver-transplant recipient in 1988,2 approximately 80 cases have been reported and the vast majority of these have been acute cases. We present a case of chronic lichenoid GVHD in a liver-transplant recipient that presented with exclusively cutaneous involvement and mixed chimerism observed in skin but not peripheral blood samples.
The patient, a 70-year-old man, had undergone a cadaveric liver transplant for cirrhosis due to hepatitis C virus infection. The crossmatch results were negative. The HLA of the donor was *1 A*68 B*39 B*39 DRB1*17 DRB1 *17 while that of the recipient was A*1 A*1 B*35 B*78 DRB1*13 DRB1*13. The patient was started on immunosuppressive treatment with tacrolimus and prednisone and was also prescribed ranitidine for gastric protection. On day 16 posttransplant, he developed an asymptomatic centrifugal maculopapular rash. The blood test results were normal and serology for cytomegalovirus, Epstein-Barr virus, and parvovirus B19 were negative for acute infection. A drug-induced reaction was therefore suspected and the skin biopsy findings were consistent with this hypothesis. Ranitidine was identified as the most probable cause and withdrawn; prednisone doses were increased to 1mg/kg/d, but no improvement was observed. A liver biopsy showed nonspecific inflammation and there was no evidence of rejection or GVHD. The patient's condition continued to worsen over the weeks. On day 122, multiple lichenoid plaques with a necrotic component covered a large area of his body (Fig. 1A and B) and there were also whitish papules in a cobblestone pattern on the oral mucosa (Fig. 1C). Repeated skin biopsies showed interface dermatitis, a perivascular infiltrate in the dermis, and necrosis of keratinocytes in the epidermis and hair follicle (Fig. 2). Analysis of peripheral blood was negative for chimerism, but mixed chimerism (90% donor cells) was detected in the affected skin. Following the diagnosis of GVHD, immunosuppressive therapy was intensified; the patient was administered prednisone 1.5mg/kg/d and tacrolimus to maintain blood levels at 10-12ng/mL, but lesions continue to appear. The patient did not develop diarrhea, cytopenia, or any other systemic symptoms during the course of the disease, and we therefore did not test for GVHD in other organs. On day 180, the patient died of disseminated invasive aspergillosis.
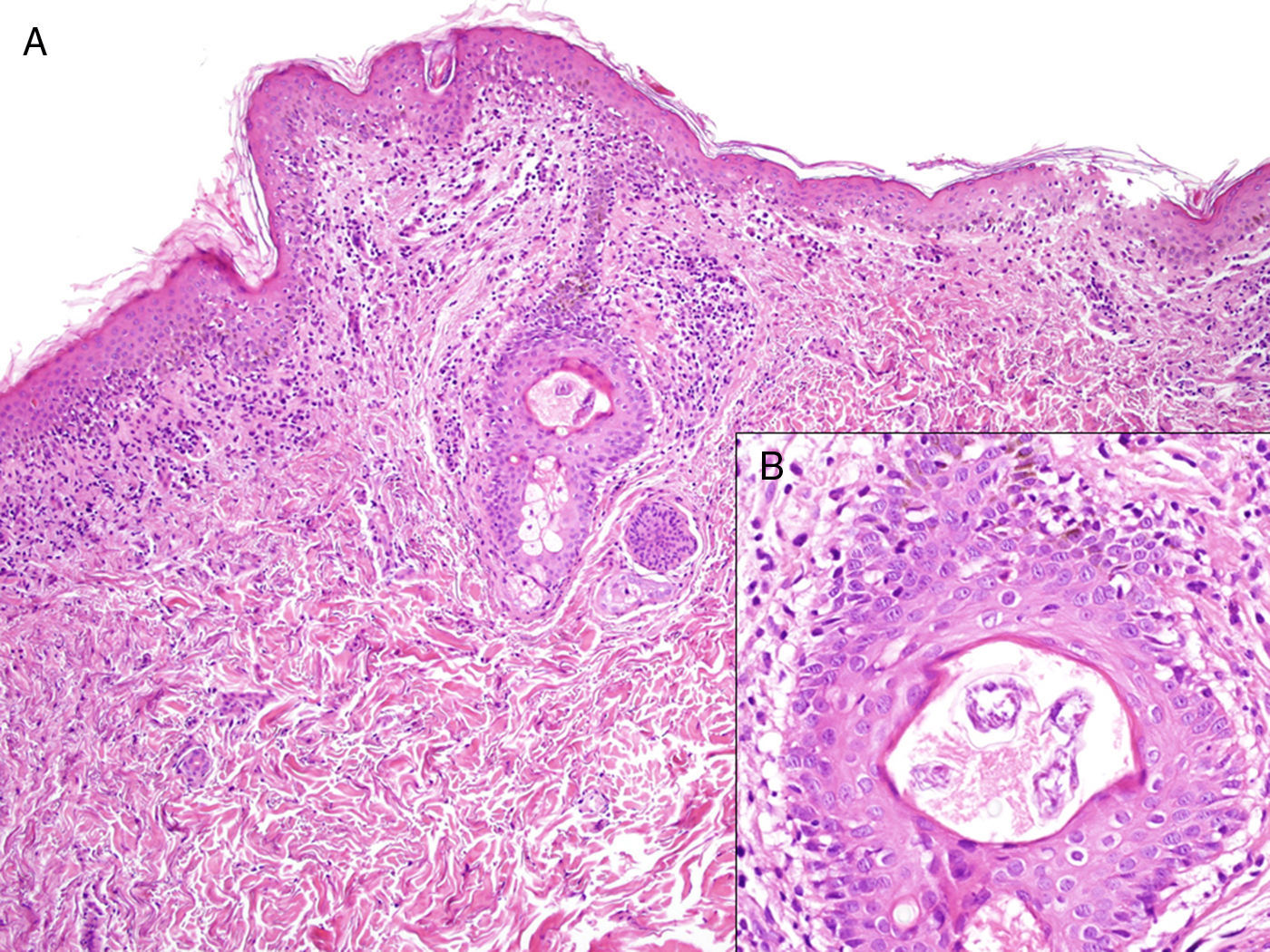
A, Hyperkeratosis with parakeratosis, vacuolization of the basal layer of the epidermis, necrosis of keratinocytes and lymphocytic infiltrate in the dermis (hematoxylin-eosin, original magnification ×10). B, Detail of histologic image showing hair follicle with keratinocyte necrosis (hematoxylin-eosin, original magnification ×40).
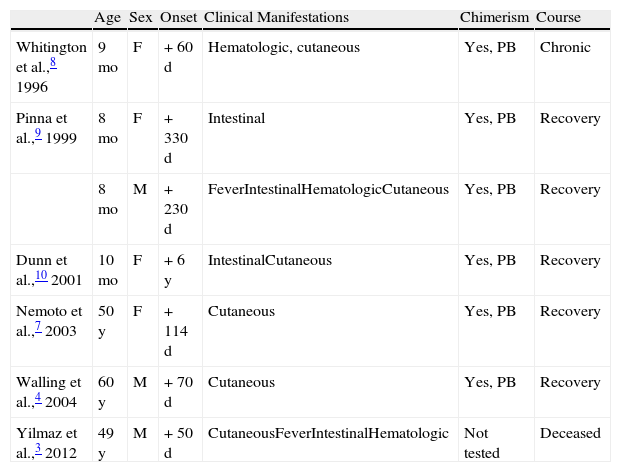
Chronic GVHD typically appears either de novo or following recovery from acute GVHD. Only Yilmaz et al.3 described a similar case to ours, in which acute GVHD progressed to chronic GVHD without a quiescent phase. It is difficult to determine the incidence of acute and chronic GVHD as their clinical and histologic findings overlap4 and the chronological criterion that establishes that acute GVHD occurs within 100 days of transplantation and that chronic GVHD occurs afterwards is insufficient. Lymphoid cells in the transplanted liver are responsible for the immune attack on the host's tissues. The skin, bone marrow, and digestive system are the most common targets. Unlike the situation with hematopoietic cell transplantation, the liver is not a target in this case as it is the engrafted organ. The lymphocytes reach peak levels a week after transplantation, but then become undetectable in the recipient's blood.5 The coexistence of donor and host cell populations is known as mixed chimerism and it has been associated with the development of GVHD. Chimerism is detected by polymerase chain reaction, which is a highly sensitive method that can detect donor polymorphisms in host tissue with a sensitivity of up to 0.1%.6 In our patient, we tested peripheral blood for chimerism on 2 separate occasions, but the results were negative. We did, however, observe a high rate of donor lymphocytes in lesional skin, suggesting an attack by the immune system. To our knowledge, this is the first time these cells have been described in target tissue without also being present in peripheral blood. We do not know if earlier tests would have detected lymphocytes in peripheral blood, that is, before they had reached the tissues. Cutaneous involvement has been reported in most cases of chronic GVHD in the literature (Table 1), but only 3 of these described a lichenoid pattern.3,4,7 Chimerism in the skin was not tested in any of the cases. Diagnosis of GVHD after liver transplantation is frequently delayed because the condition is rare and has nonspecific signs and symptoms that may be confused with those seen in drug-induced reactions or viral infections. Furthermore, the histology findings are practically indistinguishable from those seen in drug-induced reactions, particularly in the early stages of disease. We would like to stress that chimerism testing in both peripheral blood and affected tissue is a valuable diagnostic tool in GVHD, a potentially fatal disease.
Characteristics of Chronic Graft-vs-Host Disease After Liver Transplantation.
| Age | Sex | Onset | Clinical Manifestations | Chimerism | Course | |
| Whitington et al.,8 1996 | 9 mo | F | +60 d | Hematologic, cutaneous | Yes, PB | Chronic |
| Pinna et al.,9 1999 | 8 mo | F | +330 d | Intestinal | Yes, PB | Recovery |
| 8 mo | M | +230 d | FeverIntestinalHematologicCutaneous | Yes, PB | Recovery | |
| Dunn et al.,10 2001 | 10 mo | F | +6 y | IntestinalCutaneous | Yes, PB | Recovery |
| Nemoto et al.,7 2003 | 50 y | F | +114 d | Cutaneous | Yes, PB | Recovery |
| Walling et al.,4 2004 | 60 y | M | +70 d | Cutaneous | Yes, PB | Recovery |
| Yilmaz et al.,3 2012 | 49 y | M | +50 d | CutaneousFeverIntestinalHematologic | Not tested | Deceased |
Abbreviations: F, female; M, male; PB, peripheral blood.
Please cite this article as: Sanz-Bueno J, Pérez-Rial G, Castellanos M, Vanaclocha F. Enfermedad injerto contra huésped liquenoide tras trasplante hepático con afectación exclusivamente cutánea. Actas Dermosifiliogr. 2014;105:198–200.