The patient was a 68-year-old man who presented with a 10-year history of a growth on the dorsum of the tongue. The lesion was asymptomatic, had not been previously treated, and had grown slowly and progressively. The patient had no relevant past medical history, smoked 20 cigarettes a day, used a dental prosthesis that he removed at night, and was undergoing treatment with nystatin mouthwashes (after meals) and omeprazole (20mg/d).
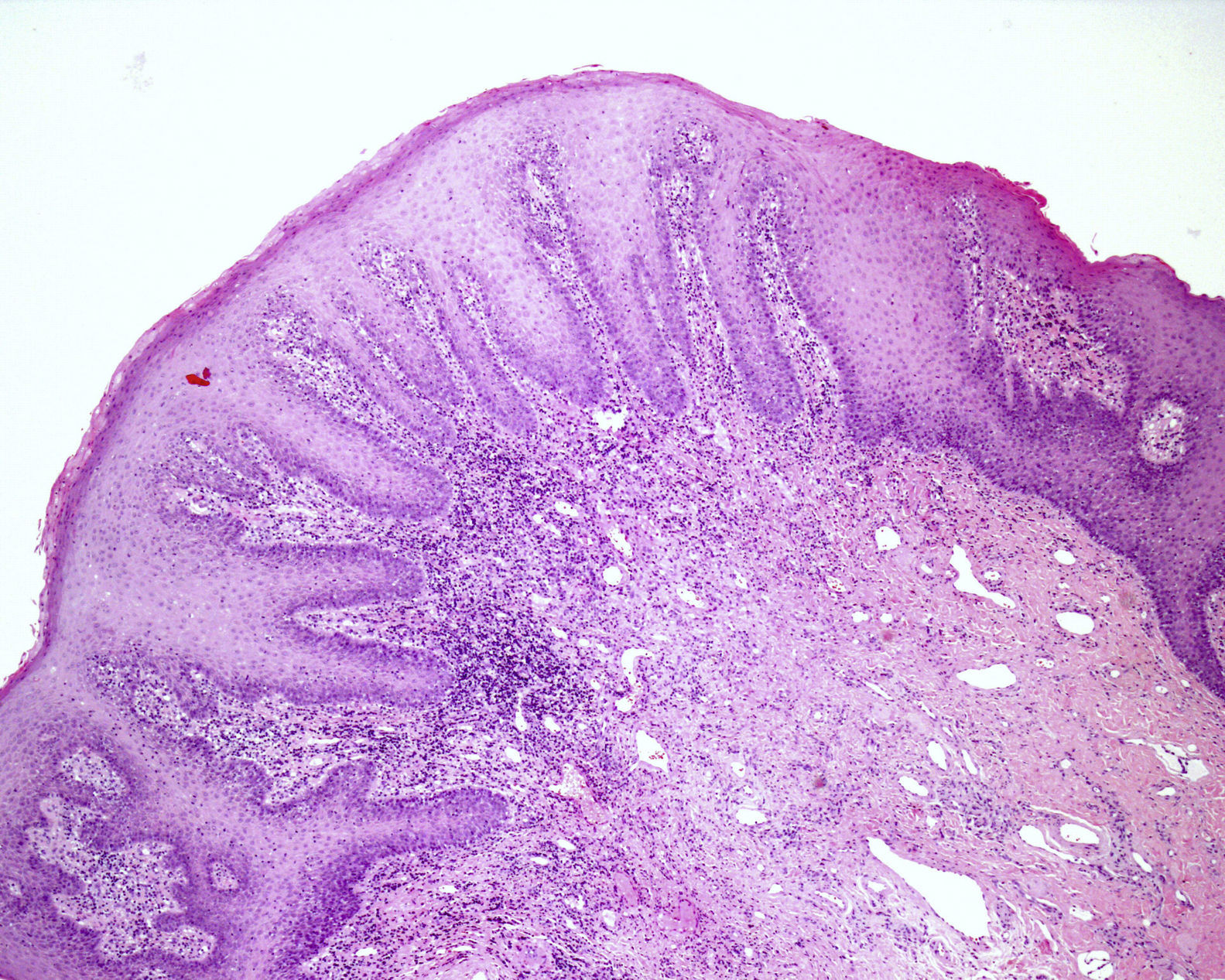
Physical ExaminationExamination revealed a coated tongue, and along the dorsal midline a pinkish, lobulated plaque with a shiny surface and rubbery consistency (Fig. 1). No lymphadenopathies were detected on palpation of the craniocervical region.
Additional testsThe following tests were performed: punch biopsy; culture in Sabouraud's medium, which was positive for Candida albicans; and routine blood tests, which were normal, including negative HIV serology.
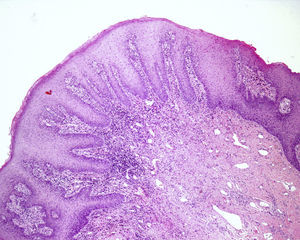
HistologyOn histology, the mucosa exhibited marked acanthosis and papillomatosis, as well as an increase in the mitotic activity of the basal layer, with no alterations in cell polarity or maturation. A moderate lymphohistiocytic interstitial infiltrate and vascular ectasia were observed in the chorion (Fig. 2). Periodic acid Schiff (PAS) and PAS diastase staining revealed no fungal structures.
What Is Your Diagnosis?
DiagnosisHypertrophic median rhomboid glossitis (MRG).
Clinical CourseQuitting smoking was recommended, and this resulted in a significant improvement and a decrease in the size of the lesion (Fig. 3). The patient was subsequently treated with fluconazole (50 mg/12 h by mouth) for 14 days, which led to some additional improvement. Despite continued systemic antifungal treatment and replacement of the patient's dental prosthesis, subsequent cultures were only transiently negative. The patient was thus referred to the otolaryngology service for carbon-dioxide laser treatment of the residual lesion, which resulted in complete resolution of the plaque with no recurrences after more than a year of follow-up.
DiscussionMRG is uncommon and probably underdiagnosed, and for many years was considered to be a malformation.1 It manifests as a clearly defined, rhomboid-shaped, atrophic or globular erythematous plaque, which appears on the midline of the dorsum of the tongue. It most commonly affects men, smokers, and diabetics, and the response to antifungal therapy is variable. Several hypotheses have been proposed to explain why the infection in MRG manifests in such a localized manner. According to Whitaker and coworkers,2 the affected region lies on the hard palate during deglutition, phonation, and rest, thus reducing its exposure to the the action of the saliva. Other authors propose that blood flow in this region is reduced compared with the rest of the tongue. In some cases an opposing erythematous plaque, or “kissing lesion”, is observed on the hard palate; according to Brown and colleagues,3 this may be a marker of associated immunosuppression.
Diagnosis is clinical, supported by a positive culture. The most commonly isolated species is Candida albicans, followed by Candida glabrata, Candida tropicalis, and Candida parapsilosis, although up to 10% of samples can contain 2 or more Candida species.4 In some cases a biopsy may be required to rule out neoplasia. PAS staining can be negative in up to 13% of cases, as Candida does not invade the epithelium and is lost during sample processing. The principal differential diagnosis is with squamous cell carcinoma and Abrikossoff tumor.5 Barret and coworkers6 observed a statistically significant association between moderate-severe epithelial dysplasia and the presence of fungi on staining with PAS; they therefore recommend screening with this staining method in this type of lesion. However, those authors were unable to state whether Candida exerts a pathogenic effect in these cases or merely colonizes previously altered tissue.
Treatment is usually topical, associated with the correction of predisposing factors; combined topical and oral therapy is reserved for highly recurrent infections or immunosuppressed patients. Surgical treatment may be useful in cases of persistent exophytic lesions, for which medical treatments are of limited effectiveness.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Ángel Castaño Pascual of the Pathology Department of Hospital Universitario de Fuenlabrada for his help with the histological study in this case.
Please cite this article as: Meseguer-Yebra C, et al. Tumoración exofítica y lineal en el dorso de la lengua. Actas Dermosi-filiogr. 2013;104:435-6.