Genital ulcer is a common presenting complaint in clinical practice and may cause considerable anxiety for patients and their families.1 Its etiology is diverse and includes infection, inflammation, drugs, injury, and tumors, and diagnosis may prove challenging.2 Lipschütz ulcer is an acute noninfectious genital ulcer that has traditionally been reported in girls who have not yet started having sexual relations,3 although it may be a frequent cause of genital ulcer in sexually active adult women.1 We report the case of a young woman with Lipschütz ulcer.
The patient was a 21-year-old woman with no history of disease and an active sex life who came to the emergency department with a 1-week history of very painful genital ulcers. She also reported odynophagia and fever during the previous 3 days. She denied having had sexual relations during the previous 2 months or having taken medication. Physical examination revealed fever (axillary temperature, 37.5 °C), painful cervical lymph nodes, and pharyngeal erythema. We observed marked edema of the labia majora and multiple round ulcers with a fibrin base and grayish halo distributed symmetrically on both sides of the vulva (Fig. 1). Cultures taken from the pharynx and the genital ulcers and serology for Epstein-Barr virus (EBV), including heterophile antibody agglutination testing and IgM and IgG testing were negative. Negative results were also recorded in serology testing for cytomegalovirus, Mycoplasma pneumoniae, syphilis, and HIV, as well as in the polymerase chain reaction (PCR) assay of the sample of the ulcer for herpesvirus types 1 and 2, Treponema pallidum, venereal lymphogranuloma, Chlamydia trachomatis (serotypes D-K), and Haemophilus ducreyi. PCR was not performed for influenza virus or other respiratory viruses. The patient was treated with ibuprofen 400 mg every 8 hours for 4 days, eau de Goulard dressings, and methylprednisolone 1% cream for 10 days. The patient’s condition progressed favorably with no complications. Her pain was relieved, and the ulcers healed in the following weeks.
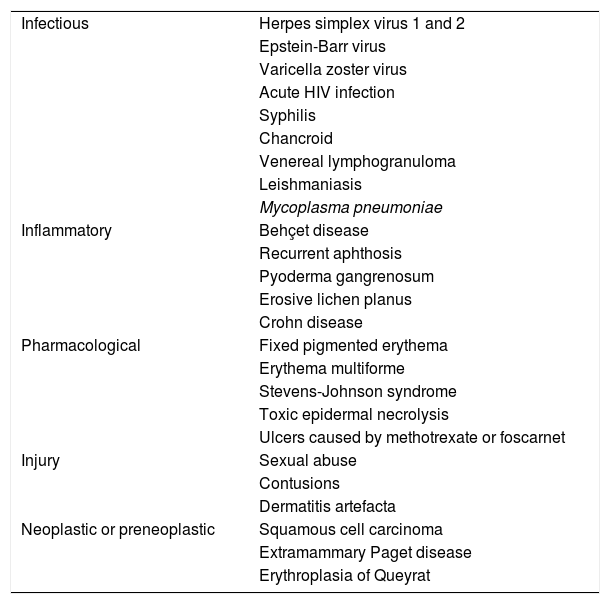
Lipschütz ulcer is a disease of unknown origin characterized by acute painful and necrotic ulcers, which have a classic symmetrical “kissing” pattern. It is sometimes preceded by flu symptoms or mononucleosis-type symptoms and is common in young women and girls who have not yet started having sexual relations.3,4 Cases in children aged under 2 years are exceptional.5 As there are no clear diagnostic criteria, Lipschütz ulcer is considered a diagnosis of exclusion; sexually transmitted infections must be ruled out as the main differential diagnosis (Table 1).1 It is generally not necessary to perform a biopsy of the mucous membrane.1 Etiology and pathogenesis seem to involve a hypersensitivity reaction to a virus or bacteria such as EBV, Mycoplasma pneumoniae, cytomegalovirus, influenza virus, and Salmonella. Consequently, we observe immune complex deposition, complement activation, small vessel thrombosis, and tissue necrosis.1,5,6
Etiology of Acute Genital Uulcers.
| Infectious | Herpes simplex virus 1 and 2 |
| Epstein-Barr virus | |
| Varicella zoster virus | |
| Acute HIV infection | |
| Syphilis | |
| Chancroid | |
| Venereal lymphogranuloma | |
| Leishmaniasis | |
| Mycoplasma pneumoniae | |
| Inflammatory | Behçet disease |
| Recurrent aphthosis | |
| Pyoderma gangrenosum | |
| Erosive lichen planus | |
| Crohn disease | |
| Pharmacological | Fixed pigmented erythema |
| Erythema multiforme | |
| Stevens-Johnson syndrome | |
| Toxic epidermal necrolysis | |
| Ulcers caused by methotrexate or foscarnet | |
| Injury | Sexual abuse |
| Contusions | |
| Dermatitis artefacta | |
| Neoplastic or preneoplastic | Squamous cell carcinoma |
| Extramammary Paget disease | |
| Erythroplasia of Queyrat |
Source: Sehgal et al.
Although Lipschütz ulcer has been associated with children, a recent publication that analyzed a series of 110 women with genital ulcers found that 30% had been diagnosed with Lipschütz ulcer at a mean age of 29 years (10–79 years) and that more than 80% had started having sexual relations. No patients had symmetrical (kissing) ulcers. The most frequent finding was multiple ulcers in the vulvar vestibule, although clinical expression was markedly polymorphic. Up to 30% had had a previous episode, and an associated microorganism, such as cytomegalovirus, EBV, Mycoplasma pneumoniae, or parvovirus B19 was detected in 27%.1
Lipschütz ulcer generally resolves spontaneously in 2 to 3 weeks without scarring. Management is based on support measures and control of pain. The measures used include sitz bath (warm water), poultices/dressings, local cleansing, oral analgesics (nonsteroidal anti-inflammatory agents or paracetamol), and topical anesthetics such as lidocaine 2%. In moderate to severe cases, we can prescribe high-potency topical corticosteroids, reserving systemic corticosteroids for cases with multiple necrotic lesions. Oral antibiotics are only indicated in the case of superinfection of the ulcers or accompanying cellulitis.6 Lipschütz ulcer can recur in up to one-third of patients. In recurrent cases, it is necessary to rule out Behçet disease.1
Lipschütz ulcer must be taken into account in the differential diagnosis of genital ulcers in adult women, even in those with an active sex life, and in recurrent cases. Given that it is a diagnosis of exclusion, it is always necessary to screen for sexually transmitted infections.
FundingThe authors declare that no funding was received for this study.
Conflicts ofinterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morgado-Carrasco D, Bosch-Amate X, Fustà-Novell X, Giavedoni P. Úlcera de Lipschütz. una úlcera genital aguda no infecciosa para tener en cuenta en mujeres adultas. Actas Dermosifiliogr. 2020;111:624–626.