A 72-year-old man was assessed for the sudden onset of an asymptomatic lesion in the malar region associated with a slight worsening of dyspnea but no sputum or fever. The patient had a history of chronic obstructive pulmonary disease for which he had been receiving treatment for several years with inhaled fluticasone propionate and repeated cycles of oral methylprednisolone.
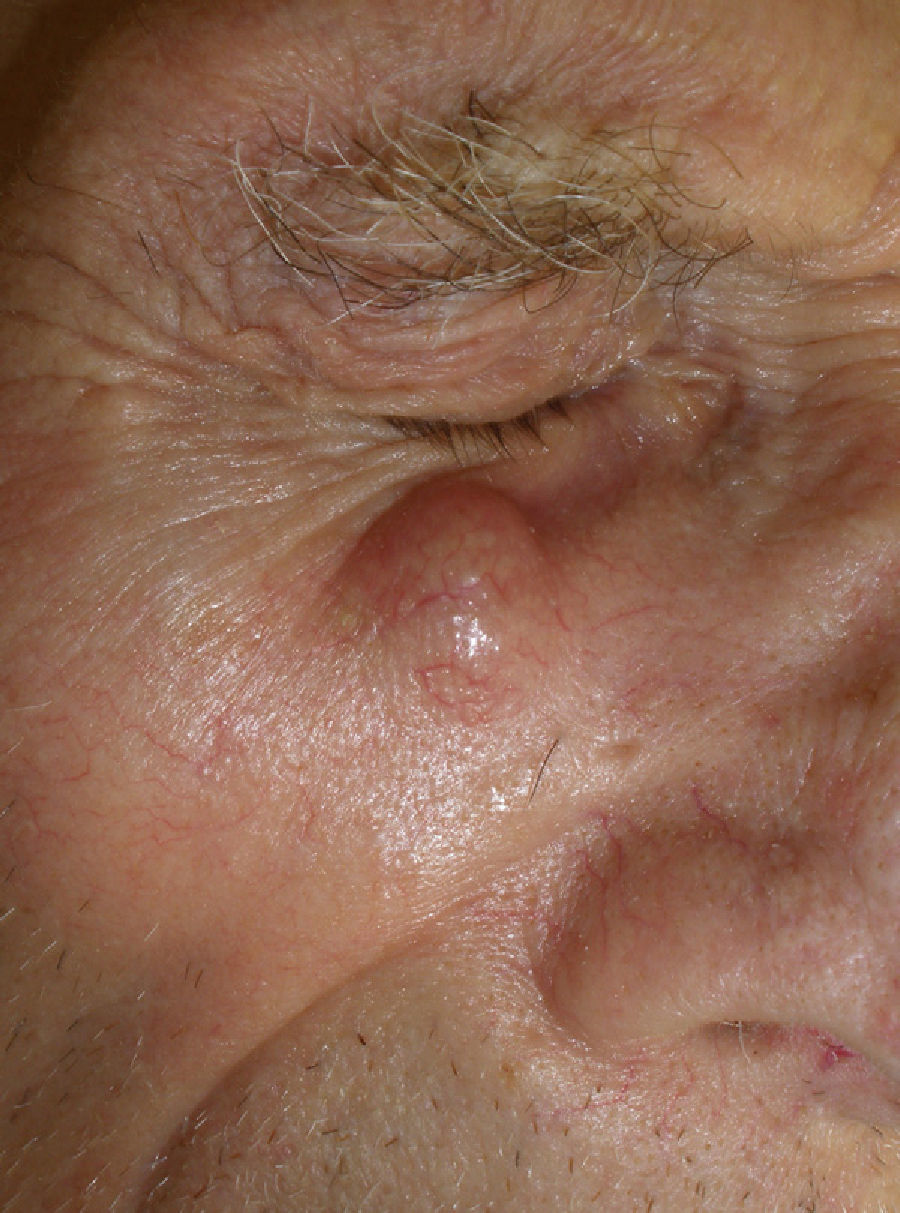
Physical ExaminationPhysical examination revealed a nodule of elastic consistency that was nonfluctuant but not attached to the underlying tissue (Fig. 1). The surface skin was intact, and no other lesions were present in the mouth or at other sites.
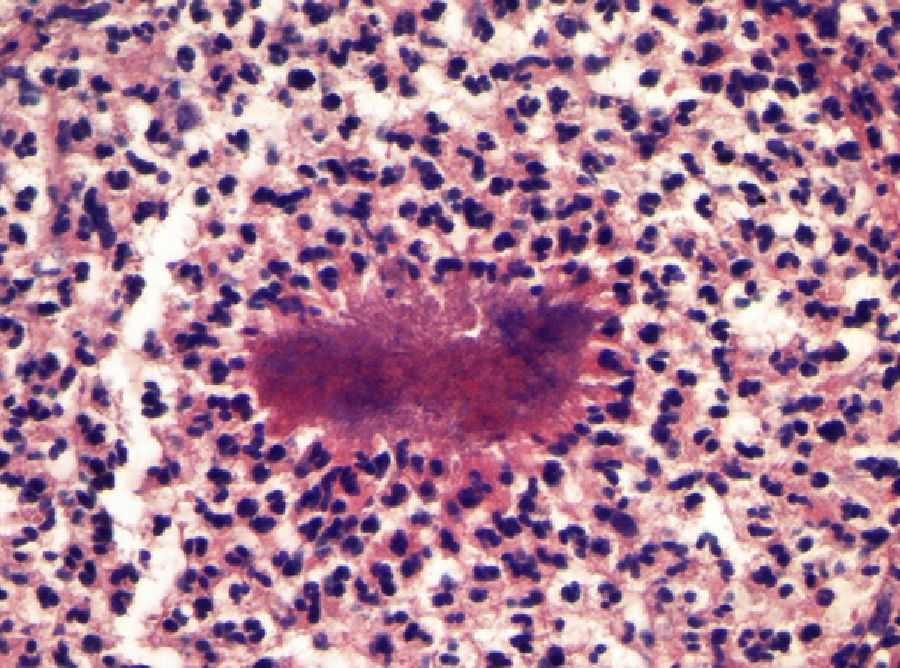
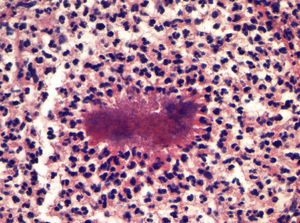
Additional TestsA punch biopsy revealed a whitish-yellow granular material, which was sterile in standard culture media. Histopathology showed an inflammatory infiltrate in the reticular dermis composed of lymphocytes, histiocytes, and numerous polymorphonuclear cells in addition to diffuse structures with basophilic cores surrounded by a filamentous eosinophilic halo (Gram, silver methenamine, and periodic acid-Schiff positive) (Fig. 2). Computed tomography of the head, neck, and abdomen revealed multiple minute, cavitated nodules distributed throughout both lung fields. Blood and sputum cultures were sterile.
What Is Your Diagnosis?
DiagnosisDisseminated actinomycosis.
Clinical CourseThe clinical, histopathologic, and radiologic findings led to a presumptive diagnosis of disseminated actinomycosis in a patient who had undergone prolonged treatment with steroids. During his hospital stay, the patient received intravenous ceftriaxone and after discharge he continued treatment with oral amoxicillin plus clavulanic acid. Radiologic assessment 3 months after completion of antibiotic treatment showed a considerable reduction in lung involvement, with no evidence of recurrence or new subcutaneous nodular lesions.
DiscussionActinomycosis is a chronic suppurative disease caused by gram-positive, non-acid-fast bacteria of the Actinomyces genus.1 These colonizing microorganisms are normally found in the gastrointestinal tract (from the oropharynx to the distal intestine) and the female genital apparatus, but they are considered to be opportunistic pathogens in specific situations, such as immunosuppression, diabetes mellitus, impaired mucosal barrier, and bronchial aspiration. The most common clinical forms are cervicofacial, lung, and abdominal.2 Skin involvement can be the result of contiguous spread resulting from maxillofacial injury or dental work, or may be caused by dissemination through the blood stream from a primary infection in one of the sites mentioned above. Clinically the lesions are asymptomatic, slow-growing abscesses or nodules with a tendency to fistulize. They exude a yellowish-white granular material (also known as sulfur granules), which contains filamentous bacterial colonies, associated with tissue elements in the exudate.3
Microbiological diagnosis is usually difficult for a variety of reasons, including the presence of other microorganisms in the samples and prior antibiotic treatment However, one of the main causes of the failure to diagnose this condition, particularly in extra-mandibular sites, is the failure to obtain and transport the sample under anaerobic conditions as a result of a low level of clinical suspicion.4–6 Blood and sputum cultures are usually negative in the pulmonary and disseminated forms. When microbiological isolation fails, treatment with beta-lactam antibiotics should be administered to patients who present symptoms suggestive of infection with bacteria of the genus Actinomyces in the presence of histopathologic findings compatible with this diagnosis.7 The differential diagnosis should include adnexal tumors, infundibular cysts, skin metastases, and other disorders caused by agents that produce actinomycetoma, such as Nocardia and Streptomyces somaliensis species.
While various antibiotics are effective against Actinomyces, beta-lactam antibiotics (penicillin, ampicillin, amoxicillin, cephalosporins) are the first-line option. Clindamycin, doxycycline, and macrolides can be used for patients allergic to beta-lactams. Surgical drainage should be performed if the lesions are accessible.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pulido Pérez A, Fernández-Antón Martínez MC, Suárez Fernández R. Nódulo malar en un varón inmunodeprimido. Actas Dermosifiliogr.2012;103:735-736.