Dermatologic surgery for tumors affecting only the ciliary region is not very common and it can sometimes be difficult to find published descriptions that deal specifically with surgery to this area. However, reconstruction of the ciliary region is very important, not only because this region is necessary to protect the eye, but also because its position and continuity are of great importance in facial expression, aesthetic appearance, and harmony. We present the cases of patients who have undergone oncologic surgery to the eyebrow region in our department in recent years and review the different techniques proposed for reconstruction of this region.
La cirugía dermatológica de tumores que afecten únicamente a la región ciliar no es muy frecuente, y en ocasiones es difícil encontrar en los distintos tratados y artículos texto que trate únicamente de la cirugía en esta región. Sin embargo, la reconstrucción de la zona ciliar es muy importante, ya que además de su función protectora del globo ocular, su posición y continuidad tienen gran importancia en la expresividad, estética y armonía facial. Presentamos casos clínicos de cirugía oncológica en la región de la ceja intervenidos en nuestro servicio en los últimos años, y realizamos una revisión de distintas técnicas propuestas para la reconstrucción de la región ciliar.
The main function of the eyebrows is to protect the eye, avoiding external aggression, whether from sweat, rain, or dust that can fall on the face; they are also of great importance in facial expression and cosmetic appearance.1 Anatomically the eyebrows can be divided into a head, body, and tail, the head being the broadest and most medial part. The hair follicles of the head of the eyebrow are oriented almost vertically, whereas those of the body and the tail are finer and become more horizontally oriented with increasing distance from the midline.2 The position of the eyebrows differs between the sexes; in women, the eyebrows are usually more arched and in a slightly higher position than in men.3 Beneath the skin of the eyebrows are the frontalis, orbicularis oculi, pyramidalis, and corrugator muscles. The blood supply to the area of the eyebrow comes mainly from anastomoses of branches of the supratrochlear, supraorbital, and superficial temporal arteries.3
Various skin tumors can arise in this area, the most common being basal cell and squamous cell carcinomas. We present case descriptions of oncologic surgery to the area of the eyebrow performed in our department. These cases include the excision of squamous cell and basal cell carcinomas and lentigo maligna melanoma, with subsequent reconstruction using advancement, advancement-rotation, and island flaps, with a subcutaneous pedicle, and we review the distinct techniques available for reconstruction of the ciliary region.
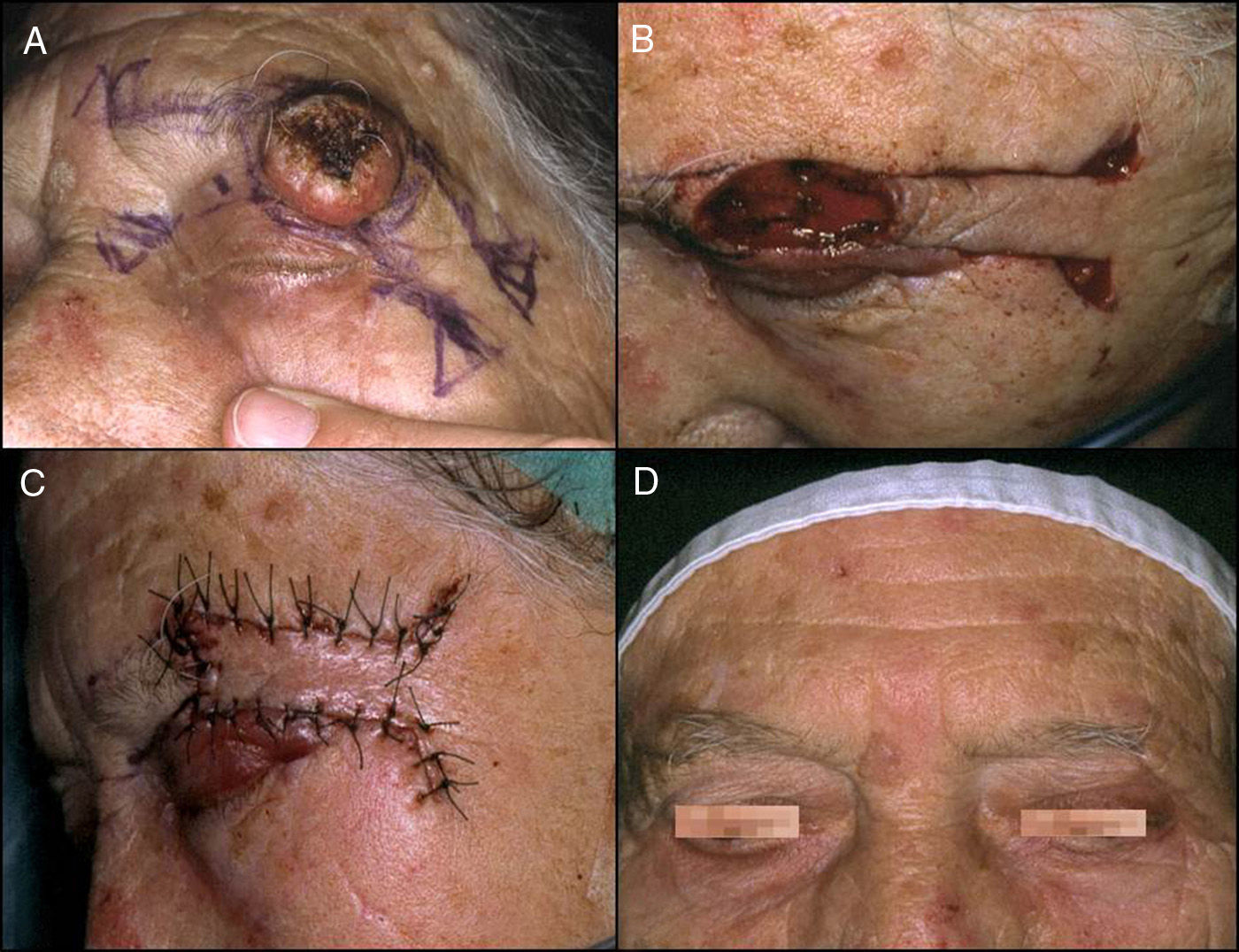
Case DescriptionsCase 1The patient was an 85-year-old woman with an indurated, lobulated plaque measuring about 12mm in diameter in the area of the tail of the left eyebrow (Fig. 1A). Under local anesthesia plus sedation, the lesion was excised with a surgical resection margin and deep dissection down to the level of the muscle, triangulating the defect superiorly. A left lateral advancement flap with a tension-releasing triangle in the inferior preauricular area was designed to cover the defect created (Fig. 1B); the flap was sutured with 3/0 polyglycolic acid and silk sutures (Fig. 1C). The pathology report described a moderately differentiated squamous cell carcinoma. At the time of removal of the sutures, the scar presented a good appearance, and the eyebrows were seen to be symmetrical (Fig. 1D).
A, Squamous cell carcinoma in the area of the tail of the left eyebrow. B, Excision of the lesion, triangulating the defect superiorly, with a left lateral advancement flap to cover the defect created. C, Result immediately after suturing with 3/0 polyglycolic acid and silk sutures. D, Result at the time of removal of the stitches, with symmetry of the 2 eyebrows.
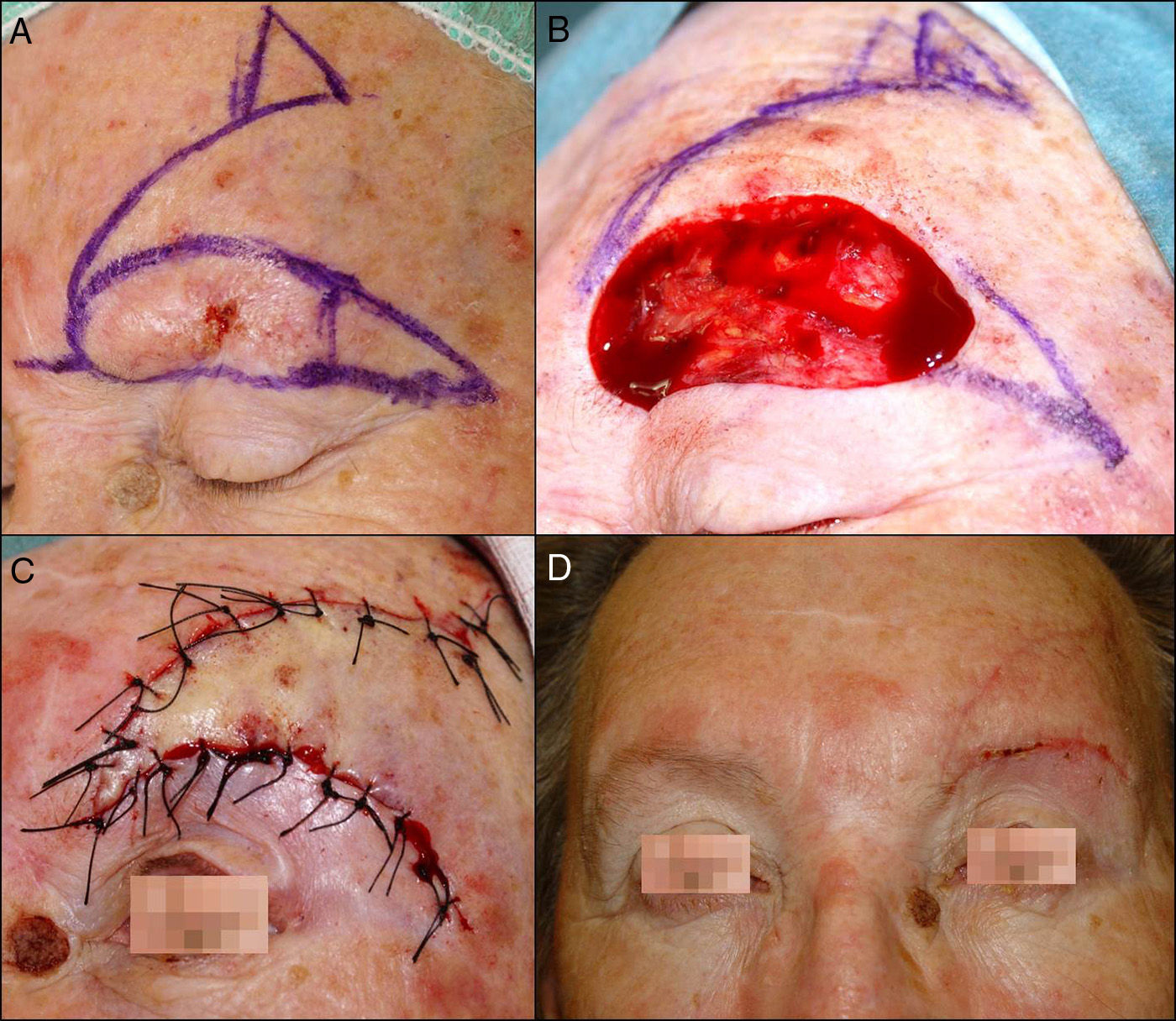
This patient, a woman of 92 years, presented a rapidly growing exophytic tumor with a central keratotic cone, situated in the area of the left eyebrow (Fig. 2A). The lesion was excised with a surgical resection margin and deep dissection down to the level of the muscle. A quadrangular advancement flap with Burow triangles at the base was designed to cover the defect (Fig. 2B); the flap was sutured with 3/0 silk (Fig. 2C). The pathology report was keratoacanthoma and the surgical margins were free of disease. The result of the surgery was satisfactory from a cosmetic point of view, with a good appearance of the scars and maintenance of eyebrow symmetry, though there was alopecia of the tail of the eyebrow (Fig. 2D).
A, Keratoacanthoma in the area of the left eyebrow. B, Excision of the lesion and design of a quadrangular advancement flap with Burow triangles at the base to cover the defect created. C, Result immediately after suturing the flap with 3/0 silk. D, Final result, showing symmetry of the eyebrows and alopecia of the tail of the left eyebrow.
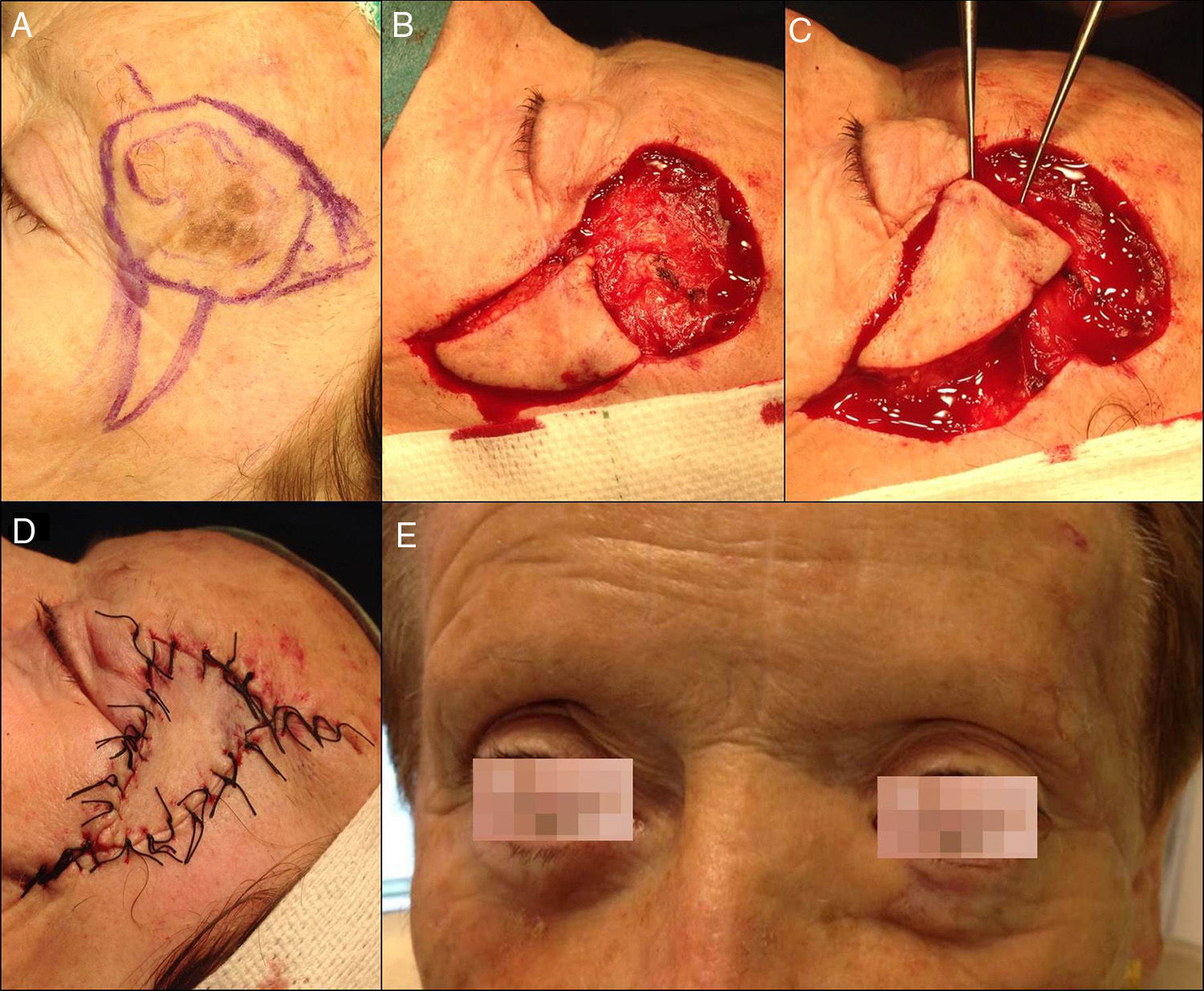
An 83-year-old woman presented a pigmented plaque in the left temporal region. The lesion contained a destructured area, with a non-homogeneous network in its superior region (Fig. 3A). An incisional biopsy was taken from the left temporal region in outpatients; this revealed histological characteristics of lentigo maligna melanoma. Subsequently, in the operating room, the lesion was excised with a 5mm surgical margin, dissecting down to the level of the subcutaneous cellular tissue. An advancement-rotation island flap with a subcutaneous cellular pedicle was designed in the left malar region (Figs. 3B and 3C). The flap was sutured with 3/0 and 4/0 silk (Fig. 3D). The pathology diagnosis was in situ lentigo maligna melanoma, at not less than 5mm from the resection margin. The result 1 month after surgery is shown in Figure 3E.
A, Asymmetric pigmented plaque in the left temporal region,with a non-homogeneous network in its superior portion; a diagnosis of lentigo maligna melanoma was made on the incisional biopsy. B and C, Excision of the lesion with 5mm surgical margins and design of an advancement-rotation flap with a subcutaneous pedicle island flap from the left malar region. D, Result immediately after suturing with 3/0 and 4/0 silk. E, Result 1 month after the operation.
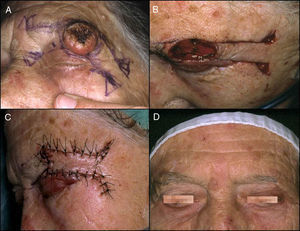
This patient was a 78-year-old woman with recurrence of a basal cell carcinoma that affected the whole body of the left eyebrow (Fig. 4A). Excision of the lesion left a large defect. The tail of the eyebrow was also excised to allow rotation of the flap (Fig. 4B). The defect was reconstructed with a superior rotation flap of the forehead, with a tension-releasing Burow triangle (Fig. 4C). The result 1 month after surgery is shown in Figure 4D.
DiscussionSkin tumors of the ciliary region are not common, as this area, like the preauricular, mandibular, and chin areas, is an area of the face that is relatively less exposed and receives less than 20% of the maximum UV exposure.4 Dermatologic surgery textbooks include this anatomic area either in the chapter on surgery of the eyelid or in the one on surgery of the forehead. We have considered it interesting to present surgical cases of large defects that mainly affect the ciliary region due to the difficulty in their reconstruction and their importance in facial esthetic appearance. When treating these cases, our main objective after performing complete tumor excision must be to reconstruct the defect with the minimal possible disturbance to eyebrow anatomy, motor function, blood supply, or innervation. In addition, the destruction of hair follicles and the creation of discontinuities in the eyebrow unit must be avoided insofar as is possible, as the cosmetic result is of great importance in facial expression.3,5 We must take a number of key points into account during reconstruction of these defects, including maintenance of the symmetry and equal length of the 2 eyebrows, as far as possible, giving preference to maintenance of the more medial portion of the eyebrow over the length of the tail.3,5
Numerous reconstruction techniques are available that help to resolve these issues, varying from direct closure to more complex surgery. Advancement, transposition, and sliding V-T or A-T flaps can be used to repair defects of the ciliary area.2,6 Silapunt et al.3 reviewed techniques for reconstruction of the eyebrow area, including the subcutaneous pedicle island flap for defects of the central or lateral area, the bilateral advancement flap for the central area, the O-T flap for the inferior border, the rotation flap, and vertical closure. Bakkour et al.5 also proposed using the subcutaneous pedicle island flap to repair defects in the medial area of the eyebrow, including the most medial area of the head of the eyebrow. Hikage et al.7 considered the use of bilobed flaps for the reconstruction of lateral defects of the eyebrow. An option for small circular defects of the ciliary region is the Mercedes flap, which allows lesions to be excised with a minimum of healthy skin and requires less tissue for closure of the defect, making the scar less visible.8 The V-Y island flap, as described by Schonauer et al.,9 drawing its blood supply from the supratrochlear artery, is another surgical option. Kim et al.10 described a technique using 2 flaps, one receiving its blood supply from the supraorbital artery and the other from a branch of the superficial temporary artery.
In order to perform a correct reconstruction, eyebrow epilation must not be performed as the direction of the hair follicles indicates the direction to be followed when suturing the defect, avoiding postsurgical asymmetry. Should complete excision of the eyebrow be necessary, patients can be offered various options to improve the cosmetic appearance of the face, such as hair microimplants2,11 and the use of false eyebrows, which give a good cosmetic result and are better than tattooing as they do not impede early detection of a possible recurrence, which can affect the area of tattoos; the appearance of basal cell carcinomas, melanomas, and squamous cell carcinomas has also been reported in the area of tattoos.4
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data confidentialityThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Santesteban R, Iglesias ME, Bonaut B. Cirugía oncológica en la región ciliar. Actas Dermosifiliogr. 2015;106:e27–e31.