The patient was a 58-year-old black man from Senegal who was living in Tenerife and had no personal or family history of interest. During his most recent trip to Senegal 1 month earlier, the patient had manipulated a wound with a wooden stick.
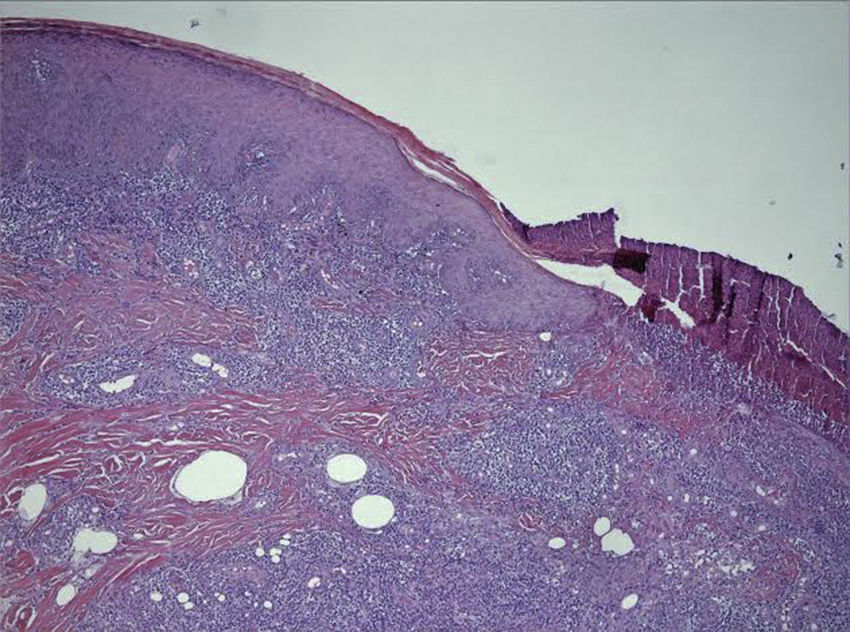
Physical ExaminationPhysical examination revealed a painful papule on the right knee with a whitish bloody exudate, measuring 1×2cm. An ulcer measuring 7×5cm, with an indurated border and a central zone containing granulation tissue, was observed on the left thigh (Fig. 1). The patient was afebrile, normotensive, with palpable peripheral pulses, and was in good general condition except for a visual analogue scale score of 7/10.
Additional TestsComplete blood count and biochemistry showed no abnormalities. Bacterial culture of the purulent exudate and a skin biopsy specimen taken from the center of the ulcer were positive for Staphylococcus aureus. Mycobacteria and fungal cultures and polymerase chain reaction for Leishmania species were negative. Serology for syphilis, human immunodeficiency virus, and hepatitis C and B viruses were negative. A tuberculin skin test was positive (11mm). An interferon-gamma release assay (QuantiFERON) was negative and a chest radiograph was within normal limits.
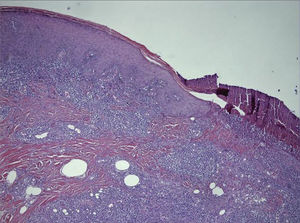
HistopathologyHistologic examination of a biopsy specimen taken from the edge of the ulcer revealed a granulomatous reaction and granulation tissue with abscess formation (Fig. 2). Periodic acid–Schiff and Ziehl-Neelsen staining of the cutaneous sample did not detect any biologic agents.
What Is Your Diagnosis?
DiagnosisTropical phagedenic ulcer.
Clinical Course and TreatmentTreatment was started with amoxicillin–clavulanic acid at a dose of 875/125mg every 78h for 14 days. Topical fusidic acid was applied to the wound on a daily basis. After 3 weeks the lesion had reduced in size by 50%, and after 3 months only the scar was visible.
CommentTropical (or tropical phagedenic) ulcers are skin lesions caused by a synergistic bacterial infection. Most cases that have been reported are associated with Fusobacterium species, Staphylococcus aureus, spirochetes, and other bacteria. The infection tends to be caused by trauma or contact with stagnant water in endemic countries such as Equatorial Guinea and Senegal.1 In the past, malnutrition was considered an important risk factor, but recent studies appear to show that there is no relationship between nutrition levels and tropical ulcers.2
A tropical ulcer is a synergistic anaerobic bacterial infection that, during its clinical course, can be colonized by aerobic microorganisms such as Staphylococcus aureus.3 In many cases, it is difficult to isolate the causative microorganism.1,4–6 The infection does not confer immunity and recurrence is therefore possible. The pathogenesis is unknown. It is now accepted that tropical ulcers are secondary to inoculation with microorganisms caused by trauma or contact with stagnant water.3,4 Diagnosis is made clinically by exclusion.3 Systemic antibiotics are curative. Penicillin is the antibiotic used most frequently and metronidazole is used in patients allergic to penicillin.1–4,6 Tropical ulcers that are not treated appropriately can progress to chronic ulcers or malignant processes such as squamous cell carcinoma.2 Given the increase in immigration and tourism to endemic countries, it is important to include tropical ulcer in the differential diagnosis for infectious ulcers, since this entity may be underdiagnosed due to its unfamiliarity. According to our review of the specialized literature, this is the third case reported in Europe to date.4,6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Latour-Álvarez I, Arteaga-Henriquez M, Rosario AdA-d. Úlcera dolorosa en paciente de raza negra. Actas Dermosifiliogr. 2018;109:351–352.