Breast cancer is the malignant tumor with the highest incidence and mortality in women worldwide.1
These tumors can give rise to both systemic and skin metastases.
Skin metastases are defined as malignant tumors that affect the dermis or subcutaneous tissue but are not contiguous with the primary tumor of origin.2
Skin metastases from internal tumors are uncommon; they can occur during the course of the neoplastic disease or be its initial manifestation.3
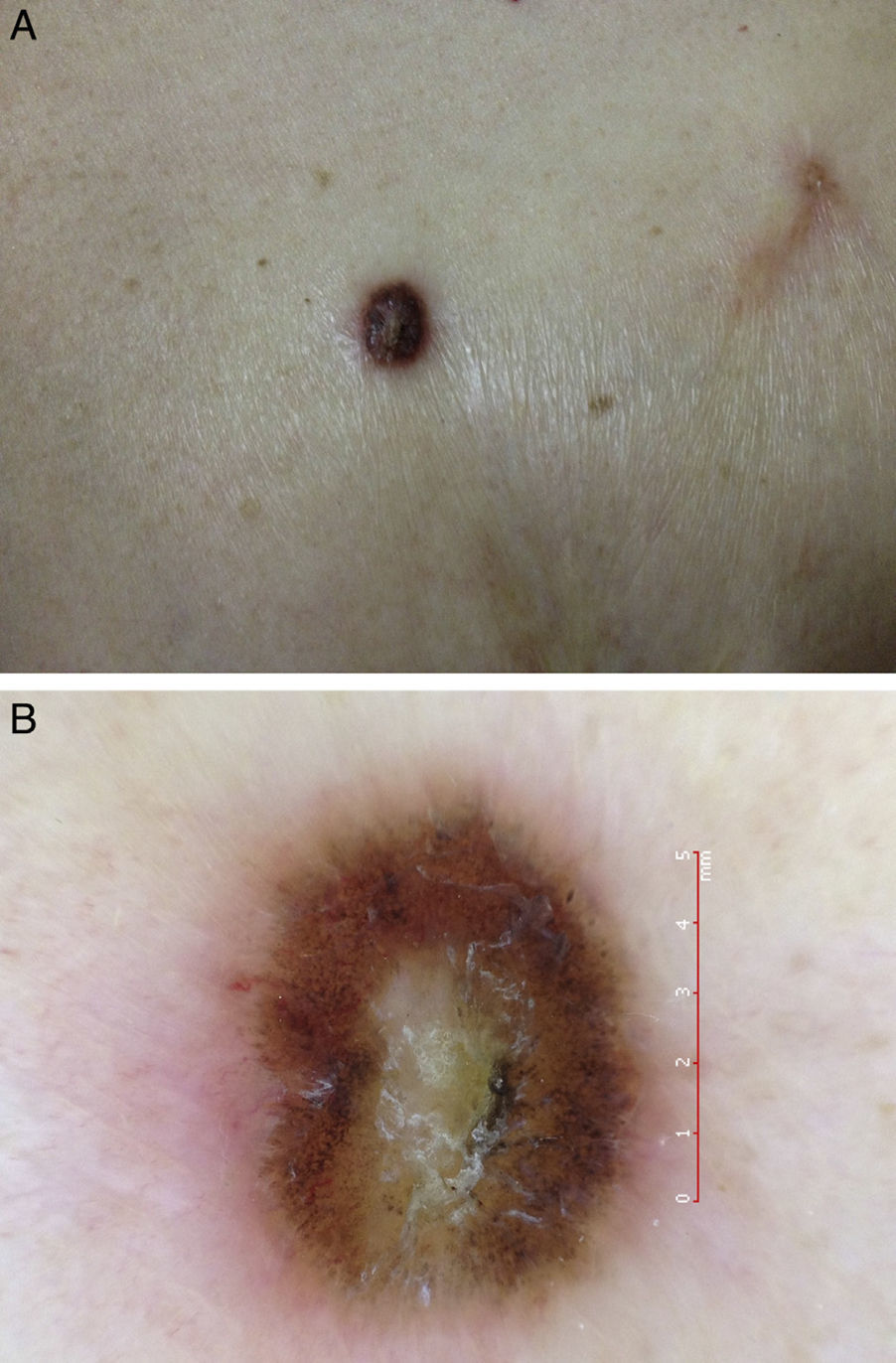
Case DescriptionA 67-year-old woman diagnosed with an infiltrating ductal carcinoma of the right breast 20 years earlier, treated by radical mastectomy, radiotherapy, and chemotherapy, and disease free up to the time of consultation, was seen for a pigmented tumor in the area of the right breast.
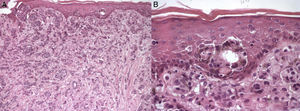
On physical examination there was a round tumor with well-defined borders on the mastectomy scar. The tumor had a black, keratotic surface and an erythematous base and measured approximately 1cm in diameter (Fig. 1A). It was slightly indurated on palpation. Dermoscopy revealed central hypopigmentation with radial projections and peripheral globules. Tortuous vessels were observed at the inferior pole (Fig. 1B).
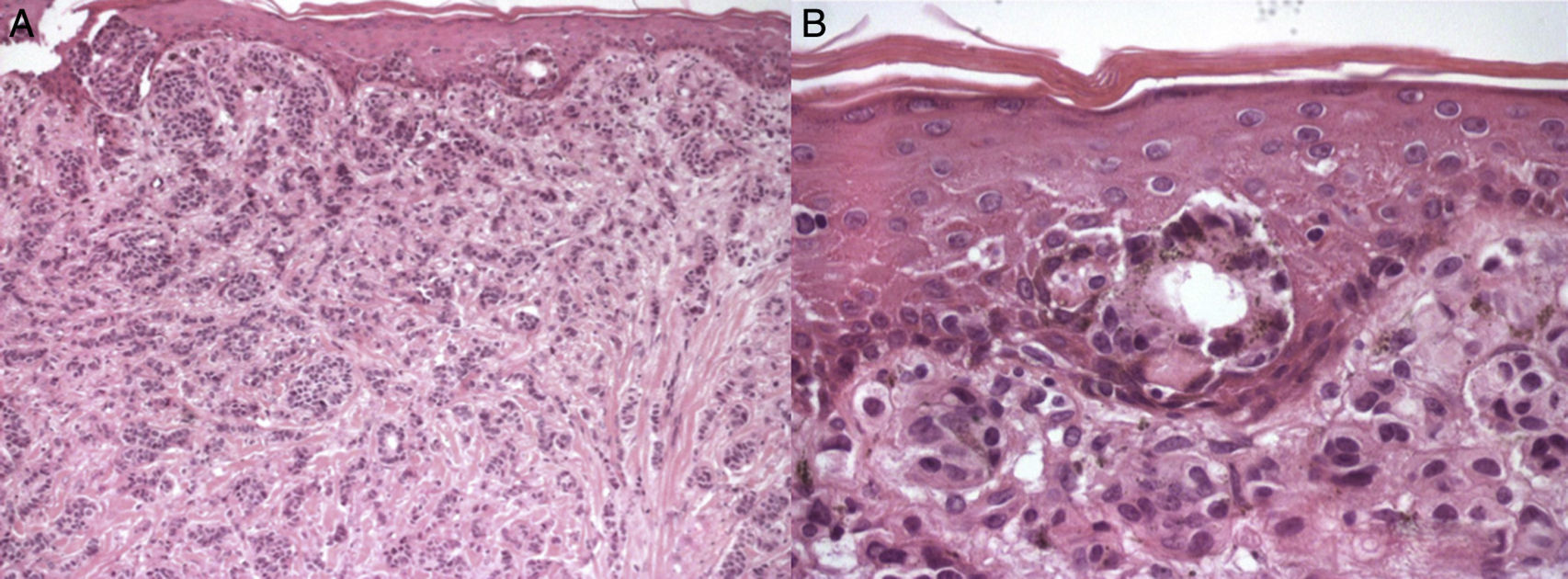
Histology of the lesion showed the dermis to be diffusely infiltrated by epithelial tumor cells with moderate cellular and nuclear pleomorphism. In some sectors the cells formed ductal structures, while in others the tumor cells were arranged in rows. The tumor infiltration affected the epidermis, showing marked epidermotropism. Pigment was observed in the superficial tumor cells and in the superficial dermis (Fig. 2).
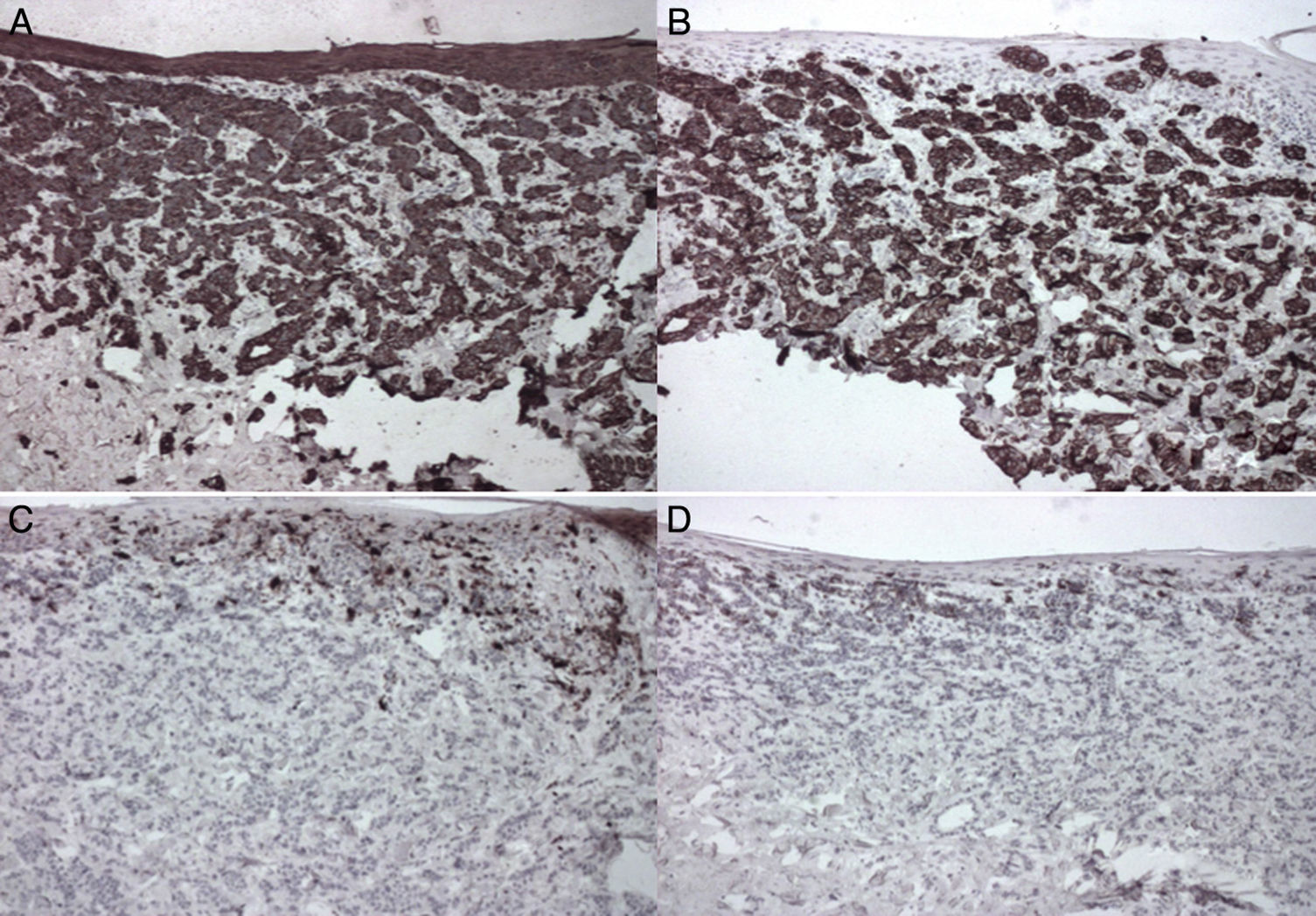
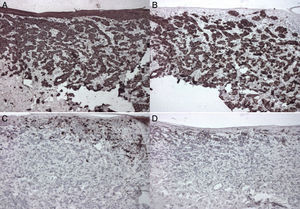
Immunohistochemistry was positive for cytokeratin (CK) 7 and negative for S100, HMB45, Melan-A, and CK20 (Fig. 3). There was focal positivity for estrogen and progesterone receptors, and the Hercep test was negative.
Based on the histopathology and immunohistochemistry findings, the patient was diagnosed with pigmented metastases from her breast carcinoma.
DiscussionThe pigmented epidermotropic form of breast carcinoma is a rare and atypical clinical presentation first described by Azzopardi and Eusebi in 1977.4,5
There are several theories about the origin of the pigment in this type of lesion. One of these theories suggests an increase in the number of melanocytes and in melanin synthesis in the lesion.5,6 Other theories maintain that there is a transfer of melanin from the melanocytes into the carcinoma cells or even that the tumor cells themselves can produce melanin.6
Clinically, the tumor presents as an indurated black lesion that usually arises in or close to the mastectomy scar.7 The most important differential diagnosis is with melanoma, which this tumor can mimic both clinically and histologically.4,7
Dermoscopy can be a useful diagnostic tool, although the literature has few data on the dermoscopic findings in skin metastases; the pigmented forms are one of the rarest.8
The histopathology of metastases from breast cancer shows the dermis to be affected by the tumor cells, which can be organized as individual cells, in rows between bundles of collagen, or forming cords, nests, glandular structures, or solid aggregates. At higher magnification, the cells have polygonal, pleomorphic, hyperchromatic nuclei. Pigmented metastases from breast cancer show a connection with the epidermis and a pagetoid ascent both of individual cells and of irregular nests. The intraepidermal and dermal tumor cells contain melanin in their cytoplasm, and numerous dermal melanophages are also seen.4,9
Immunohistochemistry is another tool that helps us to make the etiologic diagnosis of the lesion, differentiating it from other clinically similar diseases such as melanoma, and it is also of prognostic significance.
Breast carcinomas usually have a CK7-positive and CK20-negative pattern. Staining for proteins S100, HMB45, and Melan-A is negative in the majority of cases, differentiating the lesion from melanoma, which usually expresses these proteins. Estrogen and progesterone hormone receptors can also be studied.
Another useful immunohistochemistry technique with prognostic and therapeutic implications is the Hercep test, which analyzes protein HER2 overexpression in breast cancer tissues; expression is associated with a poorer prognosis.10
The treatment of skin metastases is by excision, although restaging of the disease must be performed to determine the most suitable management.
In conclusion, we have presented a case of a pigmented skin metastasis from breast cancer that had been diagnosed 20 years earlier. We highlight the importance of its clinical and histological differentiation from malignant melanoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ubillos N, Vola M, Mazzei ME, Magliano J. Metástasis cutánea pigmentada de carcinoma de mama simulando un melanoma. Actas Dermosifiliogr. 2016;107:699–701.