A 45-year-old man with no relevant past history presented with a lesion of 2 years’ duration on the left wing of the nose. He reported no itching, pain, or any other symptoms.
Physical ExaminationExamination showed a poorly circumscribed, firm erythematous plaque with a diameter of approximately 3cm on the left wing of the nose and cheek. There were also several nodules with a hard consistency and a slight yellowish color on the plaque (Fig. 1).
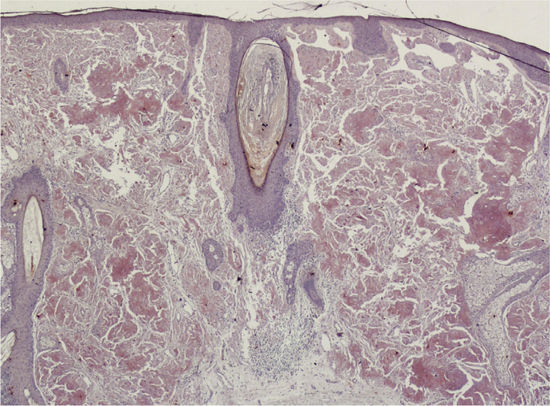
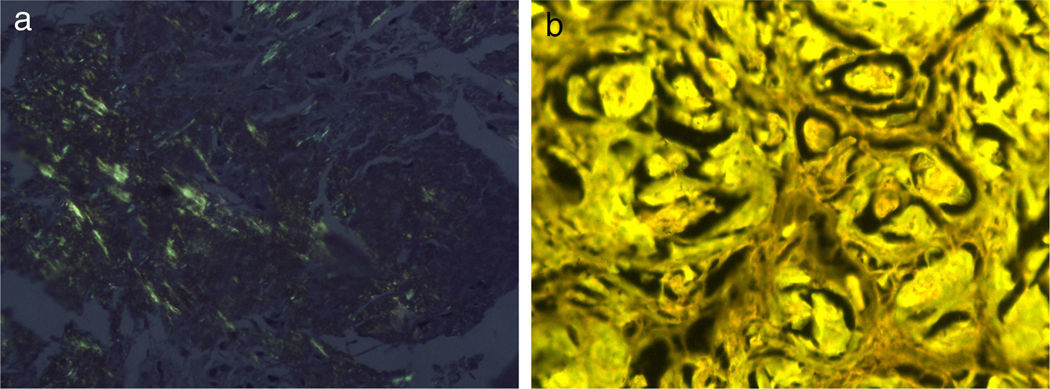
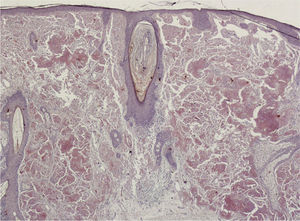
HistopathologyHistology of the lesion showed epidermal atrophy and deposits of an amorphous eosinophilic material throughout the papillary and reticular dermis. Next to this material was a mild plasma cell infiltrate (Fig. 2). Congo red staining showed bright apple-green birefringence under polarized light (Fig. 3A), and the deposited material exhibited fluorescence with thioflavin T staining under fluorescence microscopy (Fig. 3B).
Additional TestsGene rearrangement analysis of the skin biopsy specimen showed B-cell clonality. Laboratory tests, which included a complete blood count, kidney and liver function tests, a protein profile and immunoglobulin tests, showed no abnormalities.
What Is Your Diagnosis?
DiagnosisPrimary nodular localized cutaneous amyloidosis (PNLCA).
CourseTwelve months later, the lesions are still stable and the patient attends periodic follow-up visits.
CommentAmyloidosis refers to a spectrum of disorders characterized by amyloid deposits in the tissues. In primary cutaneous amyloidosis, the deposited material is confined to the skin, without involvement of any other organs.1 A distinction is made between macular amyloidosis, lichen amyloidosis, and the less common form, nodular amyloidosis.2 In macular and lichenoid amyloidosis, the amyloid deposits, which are typically found in the papillary dermis, are derived from the degeneration of keratin filaments.3 In PNLCA, the deposited material is observed in both the papillary and the reticular dermis, and may extend as far as the subcutaneous tissue. Because the amyloid proteins deposited in PNLCA are produced by plasma cells, some authors have suggested that the condition should be considered an extramedullary plasmacytoma with local amyloid deposition. Gene rearrangement studies have demonstrated plasma-cell but not bone marrow–cell clonality.4
The clinical presentation consists of firm erythematous or yellowish nodules or plaques with a shiny surface. The lesions are usually solitary, but multiple, disseminated lesions may occasionally be observed.3 PNLCA tends to affect acral sites and the most frequently involved locations are the lower limbs, the nose, and the periauricular areas.5 The condition has been associated with systemic diseases such as Sjögren syndrome,6 diabetes mellitus, and CREST syndrome (Calcinosis, Raynaud phenomenon, Esophageal dysmotility, Sclerodactyly, and Telangiectasia).
Histology findings include epidermal atrophy and deposits of amorphous eosinophilic material occupying the dermis and the hypodermis. A perivascular plasma cell infiltrate is also a characteristic feature
PNLCA generally runs an indolent course, but close follow-up is recommended as there have been reports of progression to systemic amyloidosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Dr Adrian Lloret for his help.
Please cite this article as: de Unamuno-Bustos B, Ballester-Sánchez R, Alegre de Miquel V. Placa en la nariz. Actas Dermosifiliogr. 2014;105:305–306.