A 47-year-old woman with no past medical history of interest had previously been seen for genital warts that had resolved completely after treatment with imiquimod cream, 5%. Five years later, she was referred back to dermatology for the appearance of similar lesions in the vulvar region.
Physical ExaminationMultiple translucent exophytic papular lesions, some of them pedunculated, were observed in the pubic region, with further grouped lesions producing a cobblestone pattern, occupying a large area of the labia majora (Fig. 1).
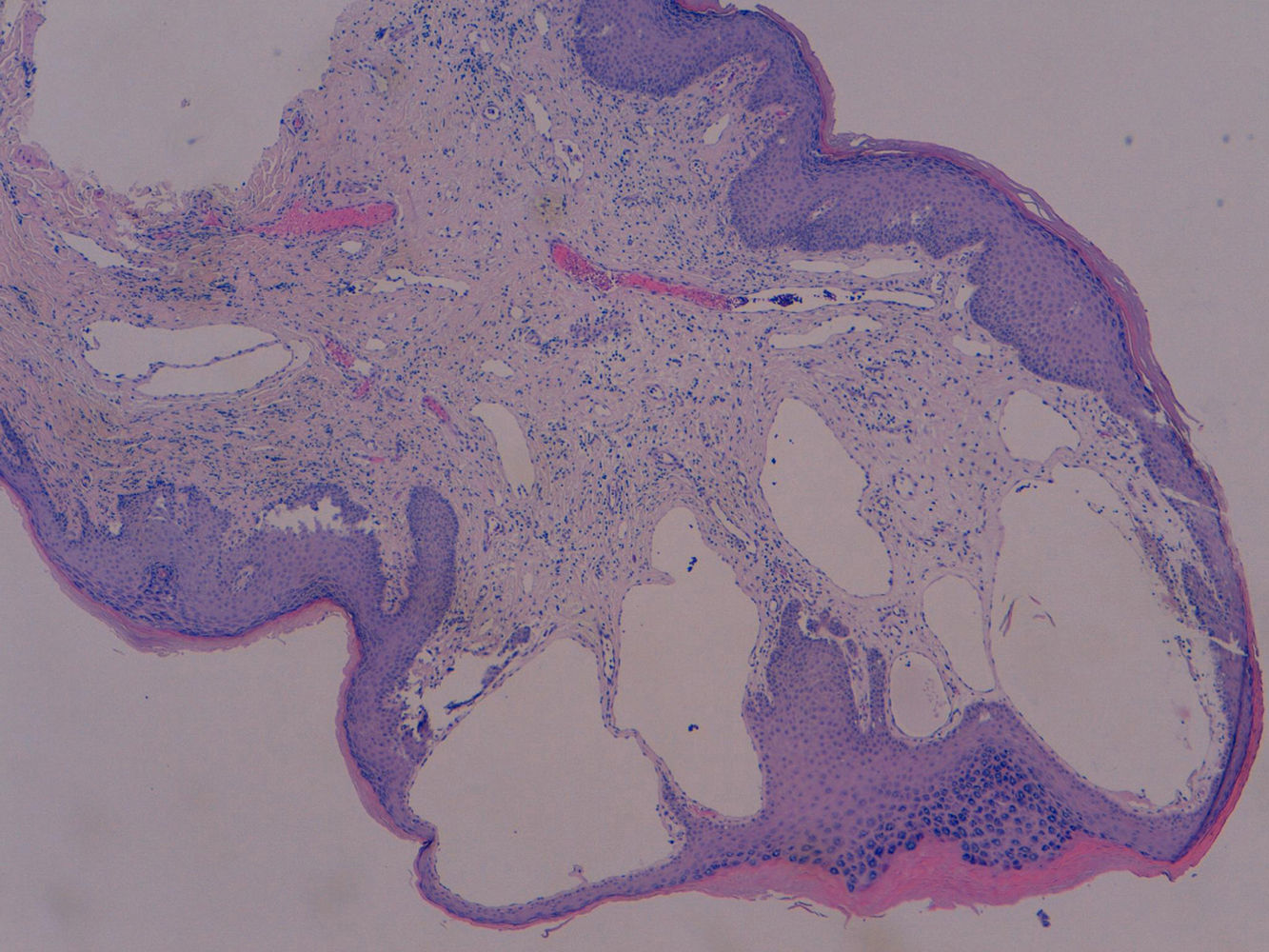
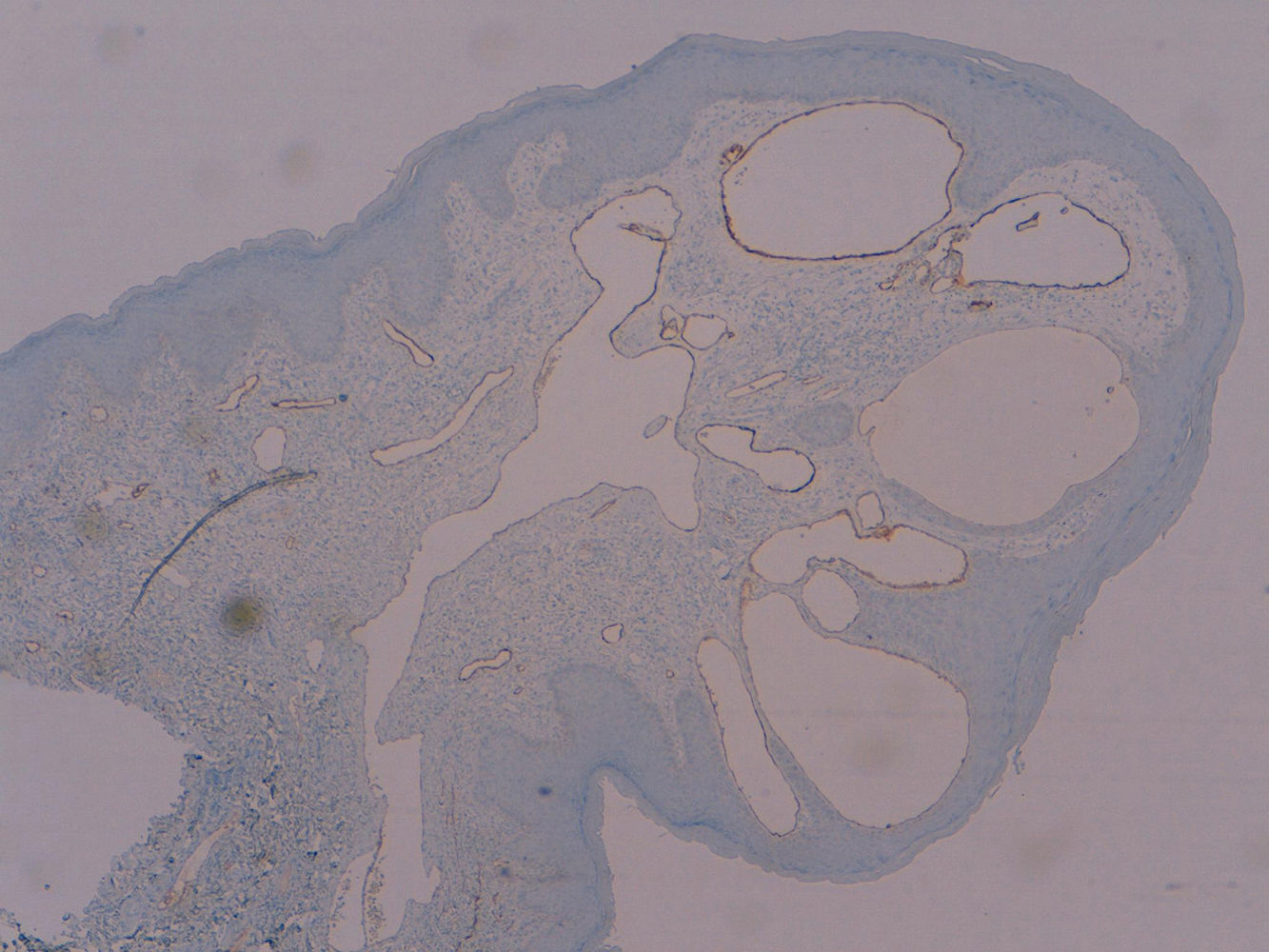
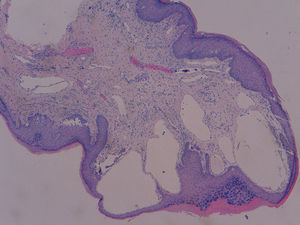
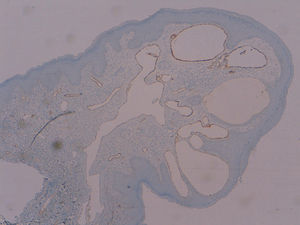
HistopathologyBiopsy of a lesion showed epidermal hyperplasia with acanthosis and hyperkeratosis with dilated lymph vessels in the papillary dermis (Fig. 2). Immunohistochemistry was positive for podoplanin (D2-40) (Fig. 3).
Additional TestsHigh-resolution skin ultrasound revealed well-defined hypoechoic dermal lesions with no intralesional blood vessels. No significant alterations of the internal genitalia were observed on abdominopelvic magnetic resonance imaging.
What is Your Diagnosis?
DiagnosisAcquired vulvar lymphangioma circumscriptum.
Clinical CourseSurgical treatment of the affected area achieved resolution of the lesions and a good functional and cosmetic result.
CommentLymphangioma circumscriptum (LC) is a rare, benign lymph vessel disorder that can arise on any area of the skin, though it is most common on the chest, thighs, and buttocks. Lesions on the vulva are uncommon. The etiology of LC is unknown, but differs between the congenital and acquired forms of the disease.1 One of the proposed etiologies for acquired LC is obstruction of the normal lymph channels, leading to their sequestration and subsequent dilatation, and the main predisposing factors for acquired vulvar LC are radical surgery and radiation therapy for cervical neoplasms. Other etiological factors include genital tuberculosis, Crohn disease with vulvar and peritoneal fistulas, infection (cellulitis, erysipelas, lymphogranuloma venereum, filariasis), trauma, keloid scars, scleredema, rhabdomyosarcoma, and pregnancy.2 Two variants have been identified: localized and classic. Classic LC is more common and presents at birth or at an early age (less than 30 years) with lesions larger than 1cm2. The localized variety is less common, occurs at any age, and the lesions, which are of less than 1cm2, are grouped in a single anatomical area. The 2 variants are distinguished histologically by the presence of grouped lymph vessels in the localized form and isolated dilated lymph vessels in the classic variant.3
Clinically, LC is characterized by the presence of isolated or grouped vesicular lesions that contain a clear fluid and measure between 1 and 5mm in diameter. The lesions may appear pink, purpuric, or black if they contain blood. Hyperkeratosis, if present, will produce a verrucous appearance, mimicking genital warts. Lesions can arise on normal skin or on preexisting papules. Vulvar LC is usually asymptomatic, although it can cause pruritus, a burning sensation, pain, or dyspareunia.4
The differential diagnosis of vulvar LC should include in particular genital warts, leiomyoma, cellular angiofibroma, angiomyofibroblastoma, angiomyxoma, verrucous tuberculosis, and lymphogranuloma venereum.5 The most common complications are vulvar edema, pain, recurrent cellulitis, and sexual dysfunction.
Numerous therapeutic options exist: cryotherapy, electrocoagulation, sclerotherapy, carbon-dioxide laser, 5-fluorouracil, and surgical excision. Although the treatment of choice is surgery, there is a high rate of recurrence, which may even be observed after radical vulvectomy, particularly with lesions measuring over 7cm.6
We have presented a new case of LC at an unusual site. This is a rare disease that can cause diagnostic error leading to the application of inappropriate treatments. It carries significant social repercussions due to possible confusion with sexually transmitted infections.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Padilla-España L, Bosco Repiso-Jiménez J, Abitei C. Pseudoverrucous Lesions of Recent Appearance on the Vulva. Actas Dermosifiliogr. 2018;109:65–66.