Digital myxoid cysts are the most common benign tumors of the fingers and toes. They present as single, generally translucent, nodules that typically affect the dorsal or lateral aspect of the distal interphalangeal joints or the proximal nail fold.1 They tend to be asymptomatic, although they can cause pain.2 The mechanism underlying their development is unclear. In most cases, degenerative changes involving the fibrous capsule of the joint are present. Multiple treatments exist, but none has proven ideal.
Polidocanol solution is a liquid sclerosing detergent that has been used to treat varicose veins, venous malformations, and other vascular anomalies.1 The aim of this study was to describe our experience with the use of polidocanol sclerotherapy in the treatment of digital myxoid cysts at 2 university hospitals in Spain.
We performed a descriptive study of 15 digital myxoid cysts treated with polidocanol at Hospital Universitario Germans Trias i Pujol and Hospital Universitario Virgen de las Nieves. The procedure consisted of making an incision in the cyst and draining the fluid after application of cryoanesthesia. Polidocanol (Etoxisclerol 20/mL) was injected through the drainage incision using an insulin needle. The area was then covered with a compression bandage for 1 week. The first follow-up visit to assess response to treatment was held after 6 weeks. Patients with persistent cysts were advised to receive a second injection and return in 6 weeks.
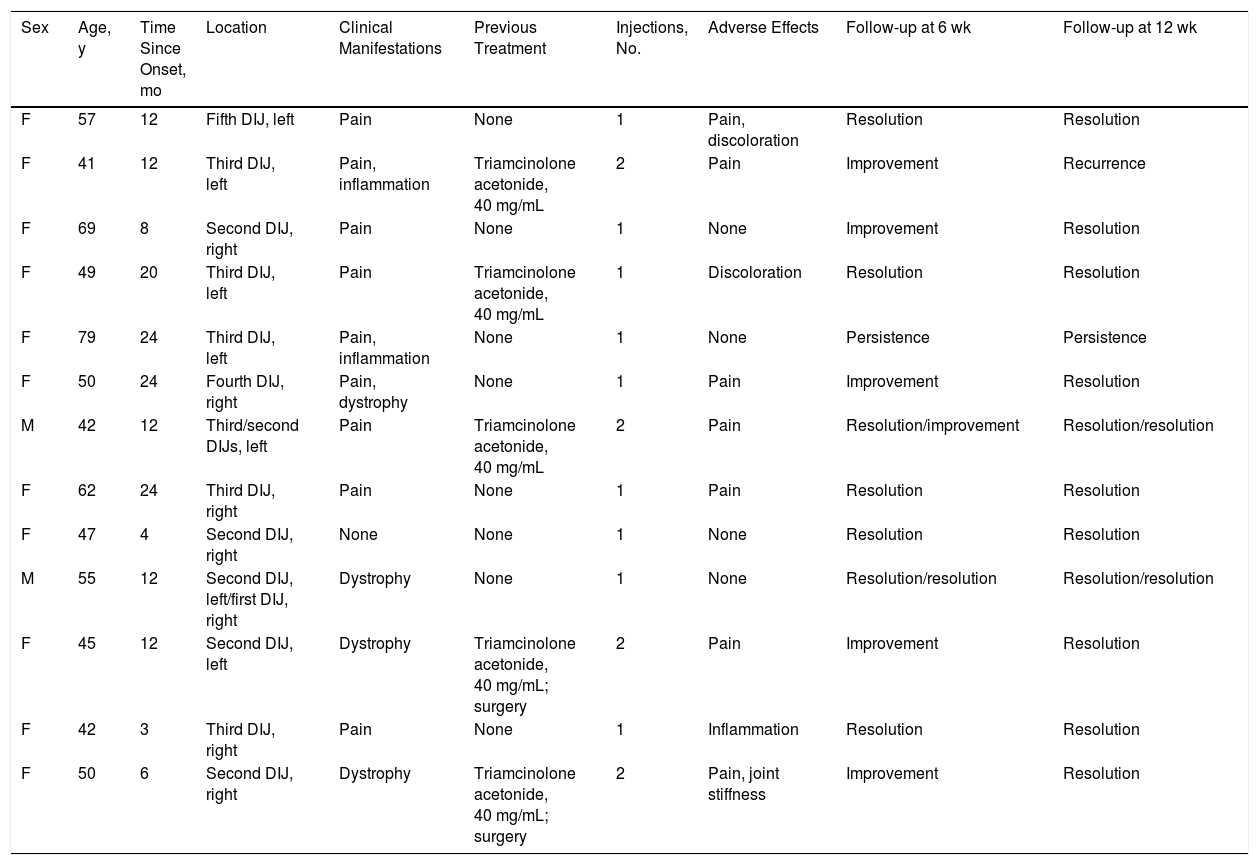
Thirteen patients with 15 myxoid cysts were treated with polidocanol sclerotherapy (Table 1). Most of the patients (11/13 [85%]) were women. Their median age was 49.5 years (range, 41-79 years) and the median time since onset was 12 months (range, 4-24 months). Pain (9/13) and nail dystrophy (4/13) were the most common symptoms. One-third of the patients (5/13) had undergone previous treatment with corticosteroid injections and surgery. All 15 myxoid cysts were located on the fingers and the most common location was the distal interphalangeal joint of the third right finger.
Summary of Clinical and Epidemiological Variants.
| Sex | Age, y | Time Since Onset, mo | Location | Clinical Manifestations | Previous Treatment | Injections, No. | Adverse Effects | Follow-up at 6 wk | Follow-up at 12 wk |
|---|---|---|---|---|---|---|---|---|---|
| F | 57 | 12 | Fifth DIJ, left | Pain | None | 1 | Pain, discoloration | Resolution | Resolution |
| F | 41 | 12 | Third DIJ, left | Pain, inflammation | Triamcinolone acetonide, 40 mg/mL | 2 | Pain | Improvement | Recurrence |
| F | 69 | 8 | Second DIJ, right | Pain | None | 1 | None | Improvement | Resolution |
| F | 49 | 20 | Third DIJ, left | Pain | Triamcinolone acetonide, 40 mg/mL | 1 | Discoloration | Resolution | Resolution |
| F | 79 | 24 | Third DIJ, left | Pain, inflammation | None | 1 | None | Persistence | Persistence |
| F | 50 | 24 | Fourth DIJ, right | Pain, dystrophy | None | 1 | Pain | Improvement | Resolution |
| M | 42 | 12 | Third/second DIJs, left | Pain | Triamcinolone acetonide, 40 mg/mL | 2 | Pain | Resolution/improvement | Resolution/resolution |
| F | 62 | 24 | Third DIJ, right | Pain | None | 1 | Pain | Resolution | Resolution |
| F | 47 | 4 | Second DIJ, right | None | None | 1 | None | Resolution | Resolution |
| M | 55 | 12 | Second DIJ, left/first DIJ, right | Dystrophy | None | 1 | None | Resolution/resolution | Resolution/resolution |
| F | 45 | 12 | Second DIJ, left | Dystrophy | Triamcinolone acetonide, 40 mg/mL; surgery | 2 | Pain | Improvement | Resolution |
| F | 42 | 3 | Third DIJ, right | Pain | None | 1 | Inflammation | Resolution | Resolution |
| F | 50 | 6 | Second DIJ, right | Dystrophy | Triamcinolone acetonide, 40 mg/mL; surgery | 2 | Pain, joint stiffness | Improvement | Resolution |
Abbreviation: DIJ, distal interphalangeal joint.
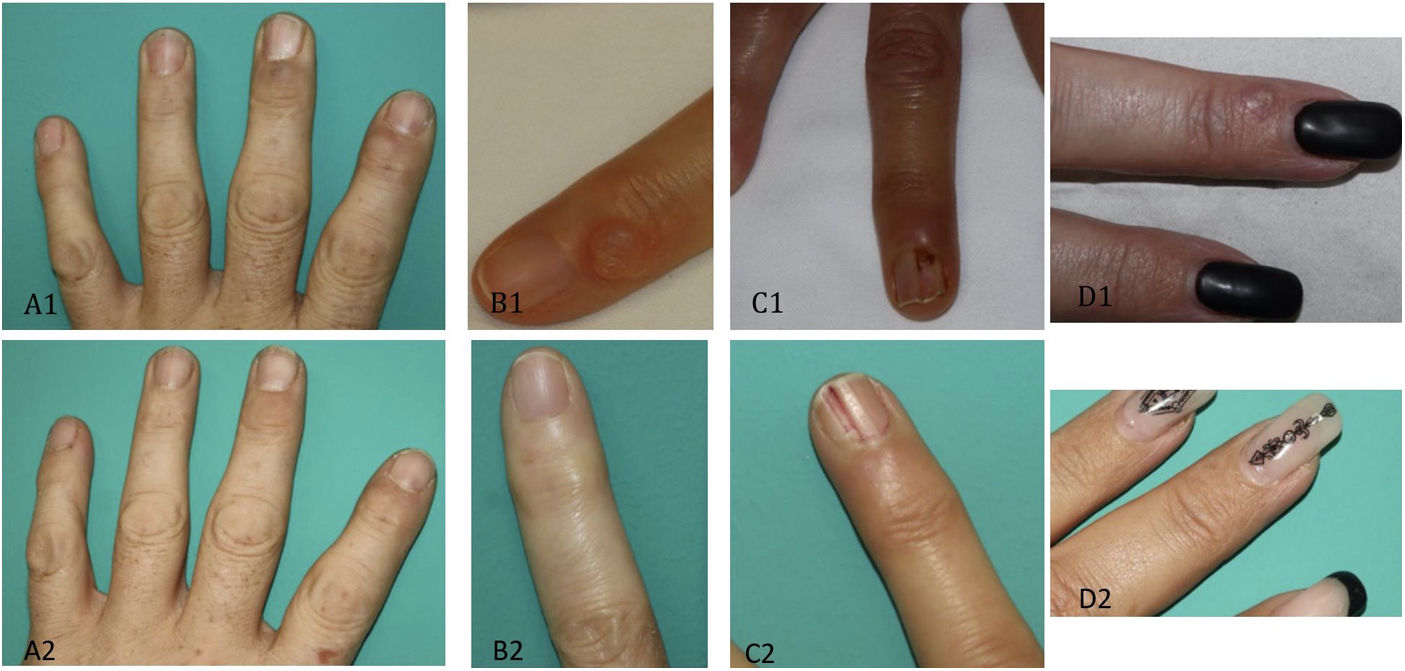
At the 6-week follow-up visit, 8 of the 15 cysts had resolved completely, 6 had improved, and 1 persisted. The 6 cysts that showed improvement were treated with a second injection and 5 of them resolved. After 12 weeks thus, 13 of the 15 cysts (86%) had resolved (Fig. 1). Half of the patients (7/13) described pain as the most common adverse effect, but this disappeared in a few days. Just 3 of the 15 myxoid cysts recurred over a follow-up period of 6 months.
Various treatments exist for symptomatic digital myxoid cysts, including drainage, injection therapy with corticosteroids or sclerosing agents, cryotherapy, carbon dioxide or Nd:YAG laser therapy, and surgical excision. No treatment guidelines are available and none of the treatments used to date has proven to be totally effective.1 Recurrence and adverse effects are common.
Little has been published on the use of polidocanol sclerotherapy in the treatment of digital myxoid cysts. Sclerosing agents include detergents (polidocanol, sodium sulfate, and sodium diatrizoate), chemical agents (iodine, alcohol), and osmotics (salicylates, hypertonic saline). Polidocanol is the most widely used agent for myxoid cysts.2 Sclerosing agents attack the cell membrane, damaging the endothelial lining and triggering occlusion of the blood vessels that feed the cyst.2
The authors of a systematic review proposed sclerotherapy as second-line treatment after surgery, as they found it was the nonsurgical technique with the highest cure rates.2,4
The response rate in our series is similar to that described in 2 previous series of 63 and 6 cases, which reported a cure rate of 80% after 1 or 2 sessions.3
Surgery has the highest success rate, with resolution in up to 95% of cases and recurrence rates ranging from 2% to 10%, depending on the approach.2,4 It is, however, an invasive technique that can cause considerable adverse effects.2 Cryotherapy has a cure rate of 61.1% and a recurrence rate of 10%.2 Corticosteroid injection therapy combined with drainage and aspiration of cyst contents is associated with a cure rate of 50% to 64% and frequent recurrences.2,4 Finally, carbon dioxide laser therapy is associated with a 66% cure rate and a 33% relapse rate.2
We have presented the largest Spanish series of digital myxoid cysts treated with polidocanol. We believe that polidocanol sclerotherapy is a good option for treating digital myxoid cysts, as it is minimally invasive and is associated with high cure rates and low recurrence and complication rates.
Please cite this article as: Blanco de Tord M, Vilchez-Márquez F, del Alcázar E, Arrieta A, Jaka A. Tratamiento de los quistes mixoides digitales con escleroterapia con polidocanol: serie de 15 casos. Actas Dermosifiliogr. 2021;112:961–963.