Herpes simplex virus (HSV) infections are widespread among humans. Their diagnosis is predominantly clinical, but its laboratory confirmation is increasingly encouraged. We conducted a 6-year retrospective, observational study of polymerase chain reaction (PCR) confirmed mucocutaneous HSV infections in the largest Portuguese tertiary teaching hospital. Throughout this period, a total of 947 PCR herpesvirus tests in mucocutaneous swabs were performed, 448 of which tested positive (266 for HSV). Regarding the PCR-confirmed mucocutaneous HSV infections, HSV-1 was the main cause of orolabial herpes and HSV-2 of genital herpes. A significant proportion of patients were immunocompromised, demonstrating the risk for herpesvirus infection and reactivation in this setting. HSV-1 genital herpes was more common in women, younger individuals and had a lower rate of recurrences. This study demonstrates the variable clinical spectrum of HSV infections, and the importance of their laboratory confirmation, as the recognition of the specific pathogen may determine optimal management and prognosis.
Las infecciones por el virus del herpes simple (VHS) son muy prevalentes a nivel mundial. Su diagnóstico es predominantemente clínico, pero cada vez se fomenta más su confirmación mediante pruebas de laboratorio. Se realizó un estudio observacional retrospectivo de las infecciones mucocutáneas por VHS confirmadas mediante reacción en cadena de la polimerasa (PCR) durante 6 años, en el mayor hospital universitario terciario portugués. Durante el periodo de estudio, se realizaron 947 pruebas mucocutáneas para detección de herpesvirus por PCR, de las cuales 448 fueron positivas, 266 para VHS. Considerando las infecciones mucocutáneas por VHS confirmadas por PCR, el VHS-1 fue la causa principal de herpes oral y el VHS-2 de herpes genital. Un tercio de los pacientes estaban inmunodeprimidos, lo que demuestra el riesgo de infección por herpesvirus y de su reactivación en este contexto. El herpes genital debido al VHS-1 fue más frecuente en mujeres, en pacientes más jóvenes y presentó una menor proporción de infección recurrente. Este estudio demuestra el espectro clínico variable de las infecciones por VHS y la importancia de su confirmación mediante pruebas de laboratorio, ya que el reconocimiento del patógeno específico puede determinar el pronóstico y el tratamiento más adecuado.
Herpes simplex virus (HSV) infections are widespread among humans, lifelong and characterized by periodic reactivations.1–3 HSV type 1 (HSV-1) is primarily transmitted by oral-to-oral contact and generally causes orolabial herpes.1 HSV type 2 (HSV-2) is almost exclusively sexually transmitted, causing genital herpes. HSV-1 genital infection from oral-to-genital contact is becoming increasingly common.4,5
HSV infection diagnosis is predominantly clinical. However, its laboratory confirmation is increasingly encouraged, as the recognition of the specific pathogen may determine optimal management and define prognosis.6 Diagnostic techniques include Tzanck smear, histopathology, immunofluorescence, electron microscopy, antigen/antibody detection, viral culture, and polymerase chain reaction (PCR). PCR is the most sensitive and specific diagnostic test.6,7 In our hospital, PCR has been available for laboratory confirmation of HSV infections since 2017.
This study aimed to characterize the clinical spectrum of PCR-confirmed HSV mucocutaneous infections in the largest tertiary teaching hospital in Portugal regarding the patients’ demographic features and comorbidities, disease clinical type, and HSV type. Furthermore, this study aimed to analyze the subgroup of PCR-confirmed genital herpes.
MethodsWe conducted a 6-year long (from January 2017 through December 2022) retrospective observational study of PCR laboratory-confirmed HSV mucocutaneous infections in Centro Hospitalar Universitário Lisboa Norte (CHULN), Portugal. Laboratory PCR test results for HSV detection in mucocutaneous swabs were analyzed (2017–2019: HSV1&HSV2 VZV R-GENE ref 69-014B®; 2020–2022: Meningitis Viral/Herpes MGB Panel ELIRTSS07ING ELITECH®), alongside health records. Patients’ demographic characteristics and comorbidities, clinical types of infection, stage of infection, and HSV type were collected. Regarding the subgroup of genital herpes, the patients’ sexual orientation and sexual behavior, type of HSV, and concomitant sexually transmitted infections (STI) were evaluated.
Statistical procedures were conducted using IBM-SPSS-Statistics®. Pairwise comparisons (post-hoc) were performed using the z-test and the independent-sample t-test, with correction for alpha inflation. Two-sided p-values <0.05 were considered statistically significant.
This study was performed in full compliance with the principles set forth in the Declaration of Helsinki. Approval was obtained from the CHULN Health Ethics Committee (335/25).
ResultsDuring the study period, a total 947 PCR tests for HSV detection in mucocutaneous swabs were performed, 448 (47.3%) of which tested positive. Of these, 182 (40.6%) identified varicella zoster virus; and 266 (59.4%), HSV.
Regarding the HSV-positive PCR tests, a total of 50.4% (n=134) were performed in the emergency department, 38.9% (n=106) during inpatient care (mostly in internal medicine and dermatovenereology departments), and 9.8% (n=26) during outpatient consultation (mainly dermatovenereology).
Most patients with PCR-confirmed HSV infection were women (n=149; 56.0%) (mean age, 43.3±22.6 years).
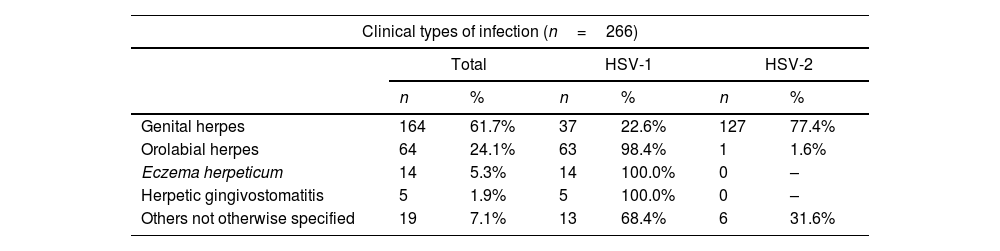
Regarding the clinical type of infection, 61.7% were genital herpes; 24.1%, orolabial herpes; 5.3%, eczema herpeticum; and 1.9%, herpetic gingivostomatitis (Table 1); 46.2% (n=123) were considered primary infections while 53.8% (n=143) were considered recurrences.
Clinical types of PCR laboratory-confirmed HSV mucocutaneous infections and associated type of HSV.
| Clinical types of infection (n=266) | ||||||
|---|---|---|---|---|---|---|
| Total | HSV-1 | HSV-2 | ||||
| n | % | n | % | n | % | |
| Genital herpes | 164 | 61.7% | 37 | 22.6% | 127 | 77.4% |
| Orolabial herpes | 64 | 24.1% | 63 | 98.4% | 1 | 1.6% |
| Eczema herpeticum | 14 | 5.3% | 14 | 100.0% | 0 | – |
| Herpetic gingivostomatitis | 5 | 1.9% | 5 | 100.0% | 0 | – |
| Others not otherwise specified | 19 | 7.1% | 13 | 68.4% | 6 | 31.6% |
Half of the patients had comorbidities (n=131; 49.2%), most commonly iatrogenic immunosuppression (n=52; 39.7%), in association with immune-mediated diseases (n=41; 31.3%), and solid organ transplant (n=11; 8.4%). Regarding the immune-mediated diseases, atopic eczema was present in 14 patients, all of them associated with eczema herpeticum. The second most common comorbid condition was oncologic disease (n=33; 25.2%), including solid organ malignancies (n=17; 13.0%), and hematologic diseases (n=16; 12.2%). Other causes of immunosuppression were also identified in this group of patients, including human immunodeficiency virus (HIV) infection (n=22; 16.8%), pregnancy (n=13; 9.9%), and diabetes mellitus (n=11; 8.4%). Regarding the stage of infection, recurrent episodes of mucocutaneous herpes simplex were more common in patients with comorbidities (n=98/131, 74.8%) vs patients without comorbidities (n=45/135, 33.3%) (p<0.01).
HSV-1 was identified in 49.6% and HSV-2 in 50.4% of patients (Table 1). Most cases of orolabial herpes, and all cases of eczema herpeticum and herpetic gingivostomatitis were caused by HSV-1. Genital herpes cases were associated with HSV-2 in 77.4% of patients.
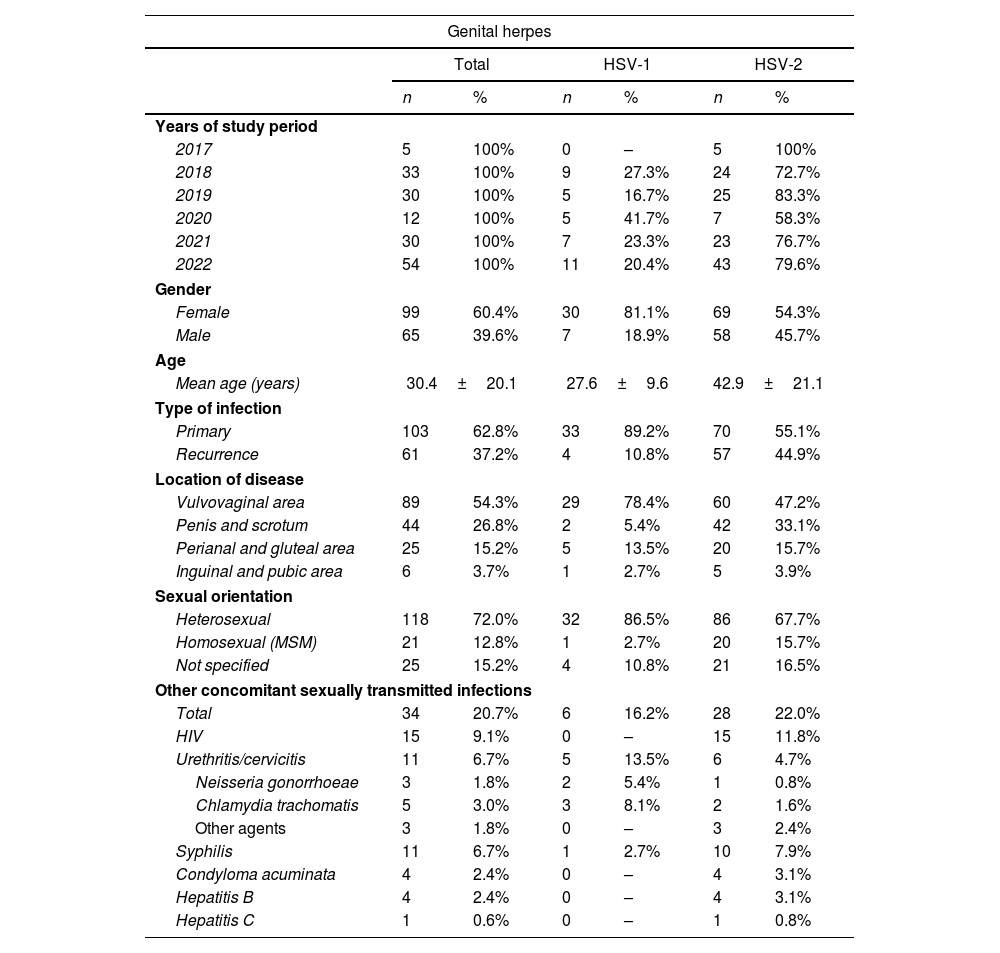
Regarding the subgroup of PCR-confirmed genital herpes (Table 2), most patients were women (60.4%) (mean age, 39.4±20.1 years), 72.0% considered themselves heterosexual and 12.8% were men who had sex with men (MSM). Genital herpes occurred most frequently on the vulvovaginal area, followed by the penis and scrotum, the perianal and gluteal areas, and the inguinal and pubic regions. A total of 103 cases of primary infection (62.8%) and 61 recurrences (37.2%) were reported.
Clinical and epidemiological characteristics of patients with PCR laboratory-confirmed genital herpes, according to HSV type.
| Genital herpes | ||||||
|---|---|---|---|---|---|---|
| Total | HSV-1 | HSV-2 | ||||
| n | % | n | % | n | % | |
| Years of study period | ||||||
| 2017 | 5 | 100% | 0 | – | 5 | 100% |
| 2018 | 33 | 100% | 9 | 27.3% | 24 | 72.7% |
| 2019 | 30 | 100% | 5 | 16.7% | 25 | 83.3% |
| 2020 | 12 | 100% | 5 | 41.7% | 7 | 58.3% |
| 2021 | 30 | 100% | 7 | 23.3% | 23 | 76.7% |
| 2022 | 54 | 100% | 11 | 20.4% | 43 | 79.6% |
| Gender | ||||||
| Female | 99 | 60.4% | 30 | 81.1% | 69 | 54.3% |
| Male | 65 | 39.6% | 7 | 18.9% | 58 | 45.7% |
| Age | ||||||
| Mean age (years) | 30.4±20.1 | 27.6±9.6 | 42.9±21.1 | |||
| Type of infection | ||||||
| Primary | 103 | 62.8% | 33 | 89.2% | 70 | 55.1% |
| Recurrence | 61 | 37.2% | 4 | 10.8% | 57 | 44.9% |
| Location of disease | ||||||
| Vulvovaginal area | 89 | 54.3% | 29 | 78.4% | 60 | 47.2% |
| Penis and scrotum | 44 | 26.8% | 2 | 5.4% | 42 | 33.1% |
| Perianal and gluteal area | 25 | 15.2% | 5 | 13.5% | 20 | 15.7% |
| Inguinal and pubic area | 6 | 3.7% | 1 | 2.7% | 5 | 3.9% |
| Sexual orientation | ||||||
| Heterosexual | 118 | 72.0% | 32 | 86.5% | 86 | 67.7% |
| Homosexual (MSM) | 21 | 12.8% | 1 | 2.7% | 20 | 15.7% |
| Not specified | 25 | 15.2% | 4 | 10.8% | 21 | 16.5% |
| Other concomitant sexually transmitted infections | ||||||
| Total | 34 | 20.7% | 6 | 16.2% | 28 | 22.0% |
| HIV | 15 | 9.1% | 0 | – | 15 | 11.8% |
| Urethritis/cervicitis | 11 | 6.7% | 5 | 13.5% | 6 | 4.7% |
| Neisseria gonorrhoeae | 3 | 1.8% | 2 | 5.4% | 1 | 0.8% |
| Chlamydia trachomatis | 5 | 3.0% | 3 | 8.1% | 2 | 1.6% |
| Other agents | 3 | 1.8% | 0 | – | 3 | 2.4% |
| Syphilis | 11 | 6.7% | 1 | 2.7% | 10 | 7.9% |
| Condyloma acuminata | 4 | 2.4% | 0 | – | 4 | 3.1% |
| Hepatitis B | 4 | 2.4% | 0 | – | 4 | 3.1% |
| Hepatitis C | 1 | 0.6% | 0 | – | 1 | 0.8% |
Other STIs were present in 20.7% of these patients, namely HIV (9.1%) (6 of which were new diagnoses), syphilis (6.7%), and urethritis/cervicitis (6.7%). Other variables of sexual behavior were not specified in most patients, and we could not characterize them.
Table 2 illustrates the clinical and epidemiological data of genital herpes according to HSV type. Compared to HSV-2, HSV-1-associated genital herpes was more common in women (p<0.01) and in younger individuals (p<0.01). Concomitant STIs were more frequent in patients with HSV-2, although with no statistical significance (p=0.22). The proportion of MSM was higher in HSV-2 associated genital herpes (p=0.03).
When evaluating recurrences, most were due to HSV-2 (n=57/61; 93.4%) (p<0.01). Moreover, the rate of recurrences was higher in patients with HSV-2 associated genital herpes (n=57/127, 44.9% vs n=4/37, 10.8%; p<0.01). The number of recurrences/year was not specified in most patients, so this parameter was not evaluated.
The proportion of HSV-1/HSV-2 laboratory-confirmed genital herpes cases throughout the study period was variable with no specific increasing or decreasing tendency (Table 2).
DiscussionAlthough the diagnosis of herpetic infections is predominantly clinical, laboratory confirmation with virus type identification is recommended, due to prognostic and therapeutic implications. PCR is the most sensitive and specific test for this purpose and has been increasingly used.6 Early and exact diagnosis of herpetic infections is especially important in cases of eczema herpeticum, genital herpes, in immunosuppressed individuals, pregnant women, and newborns. In these cases, laboratory confirmation of mucocutaneous herpetic infections with identification of the specific virus type may guide therapeutic decisions and patient monitoring.6,7
As previously reported, our study demonstrates the variable clinical spectrum of HSV mucocutaneous infections, with a good representation of different disease presentations. HSV-1 was the main cause of orolabial herpes, herpetic gingivostomatitis, and eczema herpeticum, and HSV-2 the main cause of genital herpes.1,2,8
Comorbidities were present in 50% of the patients (mostly immunosuppression), and recurrences were more common in this group, demonstrating the risk for herpesvirus infection and reactivation in this setting.1,2,7 Although most HSV mucocutaneous infections are self-limiting, there is a risk for severe and widespread infection in immunocompromised patients with possible life-threatening complications,2,7 meaning it is of paramount importance that physicians pay closer attention to this group of patients.
Regarding the subgroup of PCR-confirmed genital herpes, other STIs were present in a significant percentage of individuals, especially HIV infection. Almost half of these HIV infections were new diagnoses at the time of observation for genital herpes. Evidence suggests there is a strong biological association between HIV and HSV-2 infections: HSV-2 infection increases susceptibility to HIV acquisition, both viruses increase transmissibility of the other, and HSV-2 disease can become severe among people with HIV.9
The incidence rate of genital herpes is increasing worldwide, and HSV-2 is the main agent. Yet, over the past decades, the proportion of HSV-1 genital herpes has increased, mainly in developed countries.4,5,10–12 In contrast, in our study, the proportion of HSV-1/HSV-2 cases was variable throughout the years with no specific increasing or decreasing tendency. Social and cultural differences across countries might amount for these differences.
Nevertheless, there were statistically significant differences between HSV-2 and HSV-1 genital herpes regarding demographic and clinical characteristics. Compared to HSV-2, HSV-1 genital herpes occurred more frequently in women and younger individuals, and were associated with a lower rate of recurrences.
The higher proportion of younger individuals associated with HSV-1 has been previously stated and might be explained by the hygiene hypothesis. The lower rates of HSV seropositivity acquired in childhood, alongside earlier sexual debut, and oral-to-genital sexual contact (mainly oral receptive sex in women) are the main risk factors for HSV-1 genital infection. Furthermore, the anatomic and histologic differences of the anogenital area in both genders may justify these differences.4,10–14
Although without statistical significance, other STIs were more common in HSV-2 genital herpes, which is consistent with previous findings that demonstrate a higher rate of sexual risk behaviors in these patients.5,12
Finally, similarly to previous reports, HSV-1 genital herpes was associated with a lower rate of recurrences, given the lesser tropism of HSV-1 to genital epithelia.4,5,10–14 These differences in frequency of reactivation are important to define the patients’ prognosis and therapy, such as indications for prophylaxis, while reducing the patients’ phycological distress and improving their quality of life.
One limitation of our study is that it was a single-center analysis based on health records, and some data could not be obtained. Another limitation is that our study only included PCR-confirmed mucocutaneous HSV infections, and did not evaluate those that were diagnosed clinically. Nonetheless, our hospital is the largest Portuguese tertiary teaching hospital and the only one in the country with an open dermatovenereology emergency department, which provided us with a substantial sample size. Hence, our findings corroborate the importance of HSV infection laboratory confirmation, as the exact diagnosis and recognition of the specific pathogen may determine optimal management and define prognosis.
CRediT authorship contribution statementAll authors contributed to the study conception and design, material preparation, data collection, and analysis. All authors contributed to the drafting process of this manuscript, critical assessment, and eventually approved its final version for submission and publication.
FundingNone declared.
Conflicts of interestNone declared.
This study was performed after being authorized by Centro Hospitalar Universitário Lisboa Norte Health Ethics Committee, Portugal (Comissão de Ética do Centro Académico de Medicina de Lisboa), process No. 335/22, February 17th, 2023. All experiments were performed in full compliance with relevant laws and institutional guidelines and in full compliance with the ethical standards set forth in the Declaration of Helsinki.