The results of the surgical excision of tumors situated in areas of skin tension, especially on the back and thighs, are often poor. Wound dehiscence can occur in the immediate postoperative period, and scar dehiscence almost always occurs in the long term. To avoid these complications, suture removal is often delayed, but this frequently leaves suture marks along the borders of a scar in which dehiscence has occurred, giving rise to a typical “crab-like” appearance (Fig. 1). However, if the sutures are removed too early, wound dehiscence is possible.
In 1992, Weber and Wulc1 described the vector-running suture for the closure of wounds situated in areas of tension in order to avoid dehiscence; when tension occurs across the borders, these sutures tend to further approximate the borders instead of allowing them to separate. Soon after that paper was published, we were regularly using these sutures to close skin defects on the back, but although the results were better than with traditional techniques, they were not always satisfactory.
Other proposed techniques can effectively prevent wound dehiscence, but subsequent scar dehiscence remains a possibility, as absorbable sutures dissolve within a period that varies between 10 and 30 days.2
To avoid scar dehiscence in the long term, we use a well-tolerated, nonabsorbable suture material that does not deteriorate over time. This ensures that wound tension is controlled and dehiscence avoided in the short term and that an imperceptible scar is achieved in the long term. We decided to place the vector-running suture entirely subcutaneously in order to leave no visible points of entry or exit.
At the 2005 CILAD conference,3 we presented a personal technique that resolved the problem of dehiscence and, since that time, we have used this technique regularly in suitable cases.
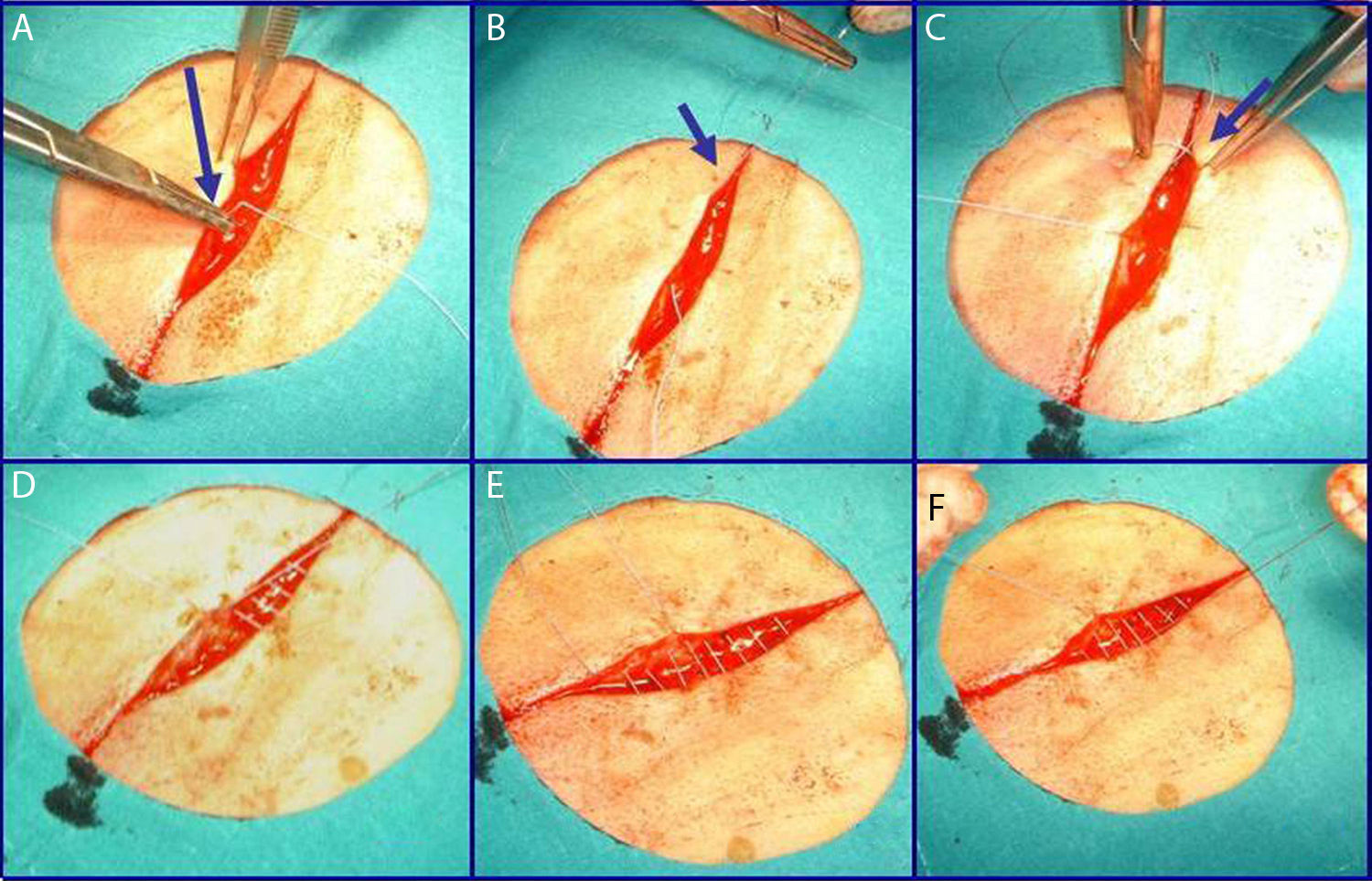
Surgical techniqueAfter excision of a tumor, and in accordance with the general principles of dermatologic surgery, we initiate closure of the resulting defect. We first suture the deep plane with a 3/0 or 4/0 braided, multifilament, absorbable, polyglycolic acid suture (Vicryl, Ethicon). We then perform the vector-running suture subcutaneously (Fig. 2). We start the suture at the midpoint of one of the borders of the wound (Fig. 2A). The curved needle is inserted into the mid-to-deep dermis and, using a circular movement, it is exteriorized as close as possible to one end of the wound (Fig. 2B). From here (Fig. 2C), we enter the opposite border of the wound to start a normal subcutaneous suture (Fig. 2D), which we continue until we reach the opposite end of the wound (Fig. 2E). From the most distal extreme of the opposite lip of the wound to where the suture was started, we introduce the needle so as to exit just opposite to the initial point of entry and we tie it with the opposite side to approximate the 2 borders (Fig. 2F). In this way, when tension develops in the wound borders, the pulley design of the suture draws the borders closer together, avoiding dehiscence.
We initially employed Gore-Tex as the suture material, based on our experience accumulated over many years with the use of these sutures as filler material in cosmetic dermatology.4 In recent years we have changed to Ti-cron (Tyco-Healthcare Spain, SL), a nonabsorbable, silicone-coated braided polyester suture uniformly, which has shown excellent tolerance in cardiac and ophthalmologic surgery.5
IndicationsThe main indication for this technique is primary closure of skin defects in areas subject to movement, particularly on the back and limbs. The tension that can develop in the borders of such wound or scar could provoke dehiscence.
As in all primary closures, wide dissection of the borders is necessary to avoid tension during suturing.
ComplicationsThe complications associated with any surgical technique can occur. Tolerance to the suture material we use is excellent. We have had no complications.
ConclusionsThe technique we have described is a simple way to prevent dehiscence of a wound or of the subsequent scar in areas of skin under tension (Fig. 3).
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Serrano-Ortega S, Serrano-Falcón C, Fernández-Pugnaire M. Sutura oblicua subcutánea. Actas Dermosifiliogr. 2015;106:71–73.