Mycosis fungoides (MF) is the most common type of primary cutaneous T-cell lymphoma (CTCL), affecting middle-aged and elderly population. The clinical manifestations are limited to the skin in early stages (eMF). Skin histopathology, immunohistochemistry and other complementary studies are required, in order to classify MF stages. The prognosis of eMF is favourable, with 98% five-year survival rate for limited patch or plaque disease.1,2
The most recommended treatments for eMF are topical therapies and phototherapy.3 Narrowband UVB phototherapy (NB-UVB) is considered to have a safer profile than PUVA and broadband UVB regarding side effects, tolerability and carcinogenesis.4 Up to the present, most MF and NB-UVB studies were performed on Caucasian and Asian populations with a schedule of three sessions per week.2,5
The aims of this study are to evaluate the response, relapse and side effects of a twice-weekly NB-UVB regimen in eMF. We compared the results with the classic three times a week schedule published in the literature. We also described for the first time the response to NB-UVB therapy in an Argentinean cohort, a mixture of Caucasian and Mestizo people (Amerindian and European ancestry).
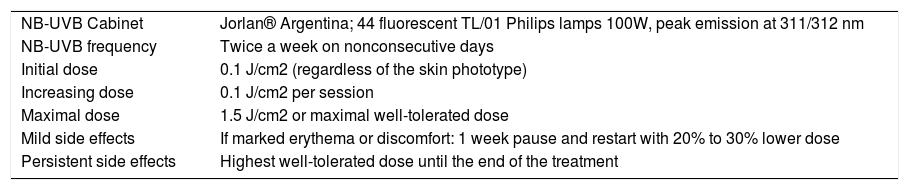
We present a retrospective analysis of adult patients (> 18 years old) with confirmed eMF,6 who underwent NB-UVB in the Department of Dermatology at “Hospital Italiano de Buenos Aires” for 8 years. Patient data were obtained from the electronic medical records. No patients presented advanced-stage MF prior to the treatment. NB-UVB treatment scheme is depicted in Table 1. Clinical evaluation was performed every 10 sessions or in the presence of side effects.
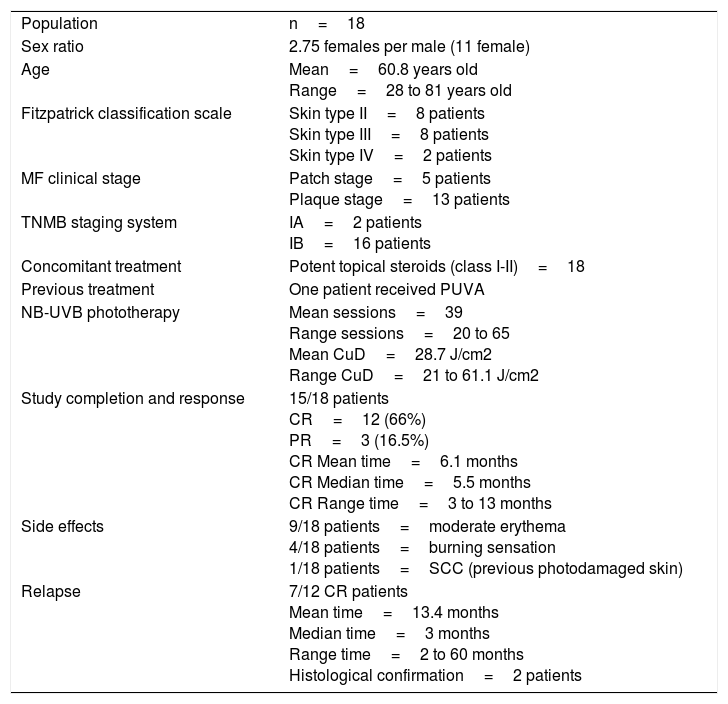
Early-stage mycosis fungoides population features.
| Population | n=18 |
| Sex ratio | 2.75 females per male (11 female) |
| Age | Mean=60.8 years old Range=28 to 81 years old |
| Fitzpatrick classification scale | Skin type II=8 patients Skin type III=8 patients Skin type IV=2 patients |
| MF clinical stage | Patch stage=5 patients Plaque stage=13 patients |
| TNMB staging system | IA=2 patients IB=16 patients |
| Concomitant treatment | Potent topical steroids (class I-II)=18 |
| Previous treatment | One patient received PUVA |
| NB-UVB phototherapy | Mean sessions=39 Range sessions=20 to 65 Mean CuD=28.7 J/cm2 Range CuD=21 to 61.1 J/cm2 |
| Study completion and response | 15/18 patients CR=12 (66%) PR=3 (16.5%) CR Mean time=6.1 months CR Median time=5.5 months CR Range time=3 to 13 months |
| Side effects | 9/18 patients=moderate erythema 4/18 patients=burning sensation 1/18 patients=SCC (previous photodamaged skin) |
| Relapse | 7/12 CR patients Mean time=13.4 months Median time=3 months Range time=2 to 60 months Histological confirmation=2 patients |
Clinical response was classified as complete (CR, >95% of skin lesions clearance), partial (PR, 50% to 95%), stable disease (<50%) and progressive disease. After achieving CR, NB-UVB frequency was reduced once-weekly for 5 weeks and then, discontinued. Remission and relapse were clinically assessed every 3 months and skin biopsies were performed, provided that the clinical picture was unclear. Late relapse was defined as the recurrence of MF more than 12 months after completion of NB-UVB.
We included a cohort of eighteen eMF patients. The study was completed by fifteen patients, while three were excluded as they developed a progressive disease. The eMF population and NB-UVB details are described in Table 2. All twelve CR patients received maintenance and five did not relapse during the follow-up period up to 36 months. Figure 1 shows the response to NB-UVB in eMF patients.
Narrowband UVB treatment scheme.
| NB-UVB Cabinet | Jorlan® Argentina; 44 fluorescent TL/01 Philips lamps 100W, peak emission at 311/312 nm |
| NB-UVB frequency | Twice a week on nonconsecutive days |
| Initial dose | 0.1 J/cm2 (regardless of the skin phototype) |
| Increasing dose | 0.1 J/cm2 per session |
| Maximal dose | 1.5 J/cm2 or maximal well-tolerated dose |
| Mild side effects | If marked erythema or discomfort: 1 week pause and restart with 20% to 30% lower dose |
| Persistent side effects | Highest well-tolerated dose until the end of the treatment |
NB-UVB is an effective therapy to improve life quality and to induce a short-term CR in MF. Our cohort of patients was treated with a twice-weekly schedule, reaching a 80% CR in a mean time of 6.1 months. Hofer et al7 reported 6 patients treated with NB-UVB 3-4 times-weekly for 5 to 10 weeks, with a mean cumulative dose (CuD) of 16.3J/cm2. Although 83% of the patients achieved CR, all of them relapsed within 6 months. Gökdemir et al8 published a prospective study with 23 early-stage MF patients, treated with a thrice-weekly schedule. A CR was achieved in 91.3% patients, the mean CuD was 90.3J/cm2 with an average of 36 sessions. In the 3-year follow-up period, only one CR patient relapsed. Relapse rate appears to be related to the CuD, rather than to the number of sessions or the schedule applied. However, we also observed a late relapse in 2 patients, which it would suggest that the response variability is still insufficiently understood.
The establishment of a maintenance therapy should be mandatory as relapse is expected in most of the patients. Boztepe et al described a maintenance therapy based on 80-160 NB-UVB sessions (12-30 months) on a decreasing frequency schedule. During this period, no relapse was observed.9 In regard to avoiding unnecessary energy accumulation and longer therapy, we decided a short-term maintenance, with a close follow-up. Relapsed eMF patients restarted NB-UVB or began PUVA (data not shown).
In order to lower side effects, we apply a common schedule to our cohort and no severe reactions were observed. Despite most publications show a shorter mean time treatment to reach CR (3-4 months), twice-weekly regimen reduces theoretically the risk of acute side effects, as well as the immunosuppressive response in the short term.8–10
A twice-weekly NB-UVB schedule in eMF is as effective as the three-times-weekly regimen. Our CR and relapse rate can be compared to the classic scheme, which confirms that the total amount of energy delivered could be more important than the frequency of exposure or the initial dose. Although longer treatments could be required to reach CuD, we emphasize the low rate of side effects and an adequate treatment compliance. Based on our clinical study, we can recommend a twice-weekly schedule as an alternative to the classical schedule, if patients report intolerance to NB-UVB.
Conflicts of InterestConflicts of Interest The authors declare that they have no conflicts of interest.
Please cite this article as: De Luca DA, Zambrano EA, Galimberti RL, Enz PA. Efectividad de la fototerapia ultravioleta B de banda estrecha con un esquema bisemanal en el tratamiento de la micosis fungoide estadio temprano en una cohorte de 18 pacientes argentinos. Actas Dermosifiliogr. 2018;109:922–924.