Poroma is a benign, exclusively cutaneous, adnexal tumor with a predilection for palmoplantar skin.
ObjectiveTo analyze the clinical characteristics of poroma in our population.
Material and methodsRetrospective study of patients diagnosed with poroma between 2002 and 2021. We conducted a chart review to record age; sex; number, location, and diameter of lesions; time since onset; clinical characteristics; suspected clinical diagnosis; resection margin status; recurrences; and follow-up duration. Categorical variables were compared using the Fisher exact test. Continuous variables were compared using the t test or the Mann–Whitney U test depending on whether they were normally or nonnormally distributed.
ResultsWe studied 80 patients (31 women and 49 men) with a median (interquartile range [IQR]) age of 65.5 (29) years. Median time since onset of poroma was 12 (21) months. Median lesion diameter was 8 (7)mm, and none of the patients had multiple lesions. The lesions were located on the head and neck in 13 cases, the trunk in 13, the upper extremities in 11, and the lower extremities in 43. Twenty-three lesions (28.8%) were located at acral sites (5 on the palms and 18 on the soles). Women were more likely to have scalp lesions (P=.041). Acral lesions were more likely to be erythematous (P=.014). Five patients experienced local recurrence.
ConclusionsAlthough poromas are particularly common in acral locations (especially the feet), most of the lesions in our series (71.3%) were located elsewhere. Acral lesions were more likely to show the classic clinical features of erythema and exophytic growth.
El poroma es un tumor anexial benigno exclusivo de la piel que tiene predilección por la piel palmoplantar.
ObjetivoAnalizar las características clínicas del poroma en nuestra población.
Material y métodosEstudio retrospectivo de los pacientes con poroma diagnosticados entre 2002 y 2021. Se revisaron las historias clínicas para obtener los siguientes datos: edad, sexo, localización, número de lesiones, diámetro, tiempo de evolución, características clínicas de los tumores, diagnóstico clínico de sospecha, estado de los márgenes de resección, desarrollo de recidiva y tiempo de seguimiento. Las variables categóricas se compararon mediante la prueba exacta de Fisher. Las variables continuas se compararon mediante la prueba t de Student cuando se confirmó la normalidad de la distribución de datos. De lo contrario, se realizó la prueba U de Mann-Whitney.
ResultadosSe incluyeron 80 pacientes con poroma (31 mujeres y 49 varones, con una edad mediana de 65,5años y rango intercuartílico [RIC] de 29años). La mediana del tiempo medio de evolución fue de 12meses, RIC 21meses, y la mediana del diámetro 8mm, RIC 7. Ningún paciente presentó lesiones múltiples. Las lesiones se localizaron en la cabeza y en el cuello en 13 casos, en el tronco en 13, en las extremidades superiores en 11 y en las extremidades inferiores en 43. Veintitrés lesiones (28,8%) se localizaron en piel acral (palmas 5, plantas 18). La localización en el cuero cabelludo fue más frecuente en el sexo femenino (p=0,041). Las lesiones acrales fueron con mayor frecuencia eritematosas (p=0,014). Cinco pacientes presentaron recidiva local.
ConclusionesAunque los poromas son especialmente frecuentes en la piel acral, sobre todo de los pies, en la mayoría de pacientes se localizan en otras regiones anatómicas (71,3%). El aspecto clínico clásico de lesión exofítica eritematosa se observa con una mayor frecuencia en las lesiones acrales.
Poroma is a benign, adnexal, tumor that was first described in 1956 by Pinkus et al.1 and exclusively affects the skin.2 It was traditionally thought to originate in the intraepidermal portion of the excretory duct of the eccrine glands (acrosyringium),3 although it is now thought to be both eccrine and apocrine in origin2,3 and may be characterized by apocrine, sebaceous, and follicular differentiation.3,4 Depending on the location of the neoplastic cells, poroid tumors used to be divided into 4 subtypes: hidroacanthoma simplex, eccrine poroma, poroid hidradenoma, and dermal duct tumor.5 However, the 2006 World Health Organization classification of cutaneous tumors considers these terms to be synonymous and groups them under the term poroma.5
Our objectives were to review the clinical characteristics of poromas in our population and to analyze possible differences between the sexes and locations.
Material and MethodsWe performed a study of cases coded as poroma in the database of the histopathology department of our hospital between 2002 and 2021. Ours is an 800-bed teaching hospital that provides care to approximately 1 million people. We performed a chart review to collect the following data: age at diagnosis (quantitative, years), sex (1, female; 2 male), location of the lesions (1, head and neck; 2, anterior trunk; 3, posterior trunk; 4, upper limbs; 5, lower limbs), location on acral skin of the hands and feet (palms, soles, and toes/fingers with a thick horny layer and absence of hair follicles), number of lesions (quantitative), tumor diameter (quantitative, mm), time from onset to diagnosis (quantitative, months), and suspected clinical diagnosis (1, poroma; 2, verruca vulgaris; 3, fibrokeratoma; 4, fibroma; 5, seborrheic keratosis; 6, basal cell carcinoma). We also recorded the clinical characteristics of the tumor, as follows: exophytic (1, yes; 2, no), plaque (1, yes; 2, no), erythema (1, yes; 2, no), painful (1, yes; 2, no), treatment (1, resection; 2, other), complete resection (1, yes; 2, no), recurrence (1, yes; 2, no), and follow-up (quantitative, months).
The data were analyzed using SPSS Statistics for Windows, Version 17.0 (SPSS Inc). A descriptive study was performed and the normality of the distribution of the quantitative variables analyzed. For the laboratory workup, we compared the parameters by sex. In addition, the characteristics of the tumors located on acral skin (palms and soles) were compared with those of tumors at other sites. Categorical variables were compared using the Fisher exact test. Continuous variables were compared using the t test when the distribution was normal. Otherwise, the Mann–Whitney test was performed. Statistical significance was set at P<.05.
ResultsWe identified 80 patients from whom a lesion had been removed and who had a histologic diagnosis of poroma during the inclusion period. The patients comprised 31 women and 49 men, with a median (interquartile range [IQR]) age of 65.5 (29) years. Time from onset to diagnosis ranged from 1 to 180 months, with a median of 12 (21) months. The median diameter was 8 (7)mm. No patients presented with multiple lesions. The lesions were located on the head and neck in 13 cases, trunk in 13, upper limbs in 11, and lower limbs in 43. Twenty-three lesions (28.8%) were located on acral skin (5 on the palms and 18 on the soles). Clinically, the lesions were exophytic in 75 cases and superficial plaques in the remainder. In 15 cases, the lesions were clinically ulcerated, in 24 they were erythematous, and in 10 cases they were painful. In 3 cases, the lesions were described as pigmented in the clinical history. The most common clinical diagnoses were fibroma (14 cases), verruca vulgaris (12), basal cell carcinoma (12), fibrokeratoma (8), seborrheic keratosis (7), and poroma (6). Treatment comprised surgical resection in 54 patients and electrocoagulation after histologic confirmation in the remainder. Resection was complete in 46 of the 54 cases. Local recurrence was recorded in only 5 patients, all after incomplete resection. Follow-up ranged from 1 to 144 months, with a median of 3 (10) months.
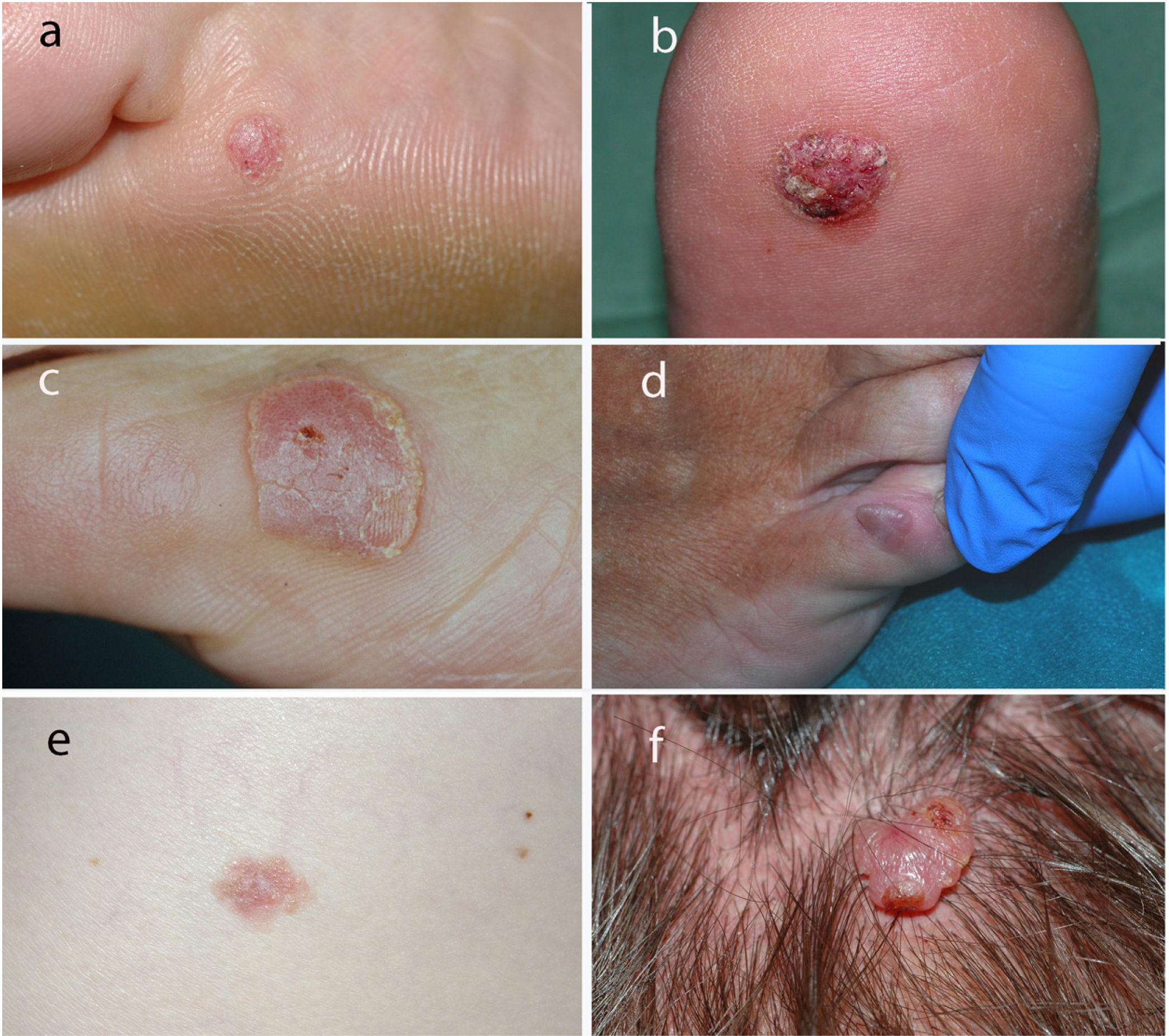
Fig. 1 shows the clinical appearance of some of the lesions.
Table 1 shows the results of the comparison of the patients’ clinical characteristics by sex. The only statistically significant differences detected were for the scalp as a location (more frequent in women [P=.041]).
Clinical Characteristics of 80 Patients with Poroma by Sex.
| 80 patients | Women, 31 (38.66%) | Men, 49 (61.34%) | |
|---|---|---|---|
| Median (IQR) age at diagnosis, y | |||
| 65.5 (29) | 62 (28) | 63 (23) | |
| Median (IQR) time from onset to diagnosis, mo | |||
| 12 (21) | 14 (19) | 12 (27) | |
| Location (80 tumors) | |||
| Head and neck, 13 (16.25%) | 8 (25.81%) | 5 (10.20%) | P=.041 |
| Scalp, 10 | Scalp, 7 | Scalp, 3 | |
| Face, 2 | Face, 0 | Face, 2 | |
| Neck, 1 | Neck, 1 | Neck, 0 | |
| Trunk, 13 (16.25%) | 5 (16.13%) | 8 (16.33%) | |
| Anterior 6 | Anterior, 3 | Anterior, 3 | |
| Posterior 7 | Posterior, 2 | Posterior, 5 | |
| Upper limbs, 11 (13.75%) | 5 (16.13%) | 6 (12.25%) | |
| Arm-forearm, 3 | Arm-forearm, 2 | Arm-forearm, 1 | |
| Hand 8 | Hand, 3 | Hand, 5 | |
| Lower limbs, 43 (53.75%) | 13 (41.94%) | 30 (61.22%) | |
| Thigh-leg, 17 | Thigh-leg, 4 | Thigh-leg, 13 | |
| Foot, 26 | Foot, 9 | Foot, 17 | |
| Acral skin, 23 (28.75%) (hand, 5; foot, 18) | 7 (22.58%) | 16 (32.65%) | |
| Median (IQR), diameter, mm | |||
| 8 (7) | 6.5 (5) | 10 (7) | |
| Exophytic, 75 (93.75%) | 28 (90.32%) | 47 (95.92%) | |
| Plaque, 5 (5.25%) | 3 (9.68%) | 2 (4.08%) | |
| Ulcerated, 15 (18.75%) | 6 (19.35%) | 9 (18.38%) | |
| Erythematous, 24 (30.00%) | 11 (35.48%) | 13 (26.53%) | |
| Painful, 10 (12.50%) | 5 (16.13%) | 5 (10.20%) | |
| Complete resection, 46/54 (85.19%) | 21/21 (100%) | 25/33 (75.75.%) | |
| Local recurrence, 5/80 (6.25%) | 2 (6.45.%) | 3 (6.12%) | |
Table 2 shows the clinical characteristics of the tumors on acral skin (palms and soles) compared with the other lesions. The acral lesions were erythematous in 52% of cases compared with 21% for the other locations (P=.014). No significant differences were observed in the remaining comparisons.
Comparison of Poromas on Acral Skin and in Other Areas.
| 80 patients | Acral, 23 (28.75%) | Other, 57 (71.25%) | |
|---|---|---|---|
| Median (IQR) age at diagnosis, y | |||
| 65.5 (29) | 64.5 (20) | 63 (29) | |
| Median (IQR) from onset to diagnosis, mo | |||
| 12 (21) | 10 (22) | 24 (30) | |
| Median (IQR) diameter, mm | |||
| 8 (7) | 8 (5) | 10 (8) | |
| Exophytic, 75 (93.75%) | 23 (100%) | 52 (91.23%) | |
| Plaque, 5 (5.25%) | 0 (0%) | 5 (8.77%) | |
| Ulcerated, 15 (18.75%) | 4 (17.39%) | 11 (19.30%) | |
| Erythematous, 24 (30.00%) | 12 (52.17%) | 12 (21.05%) | P=.014 |
| Painful, 10 (12.50%) | 4 (17.39%) | 6 (10.53%) | |
| Complete resection, 46/54 (85.19%) | 11/12 (91.67%) | 35/43 (81.40%) | |
| Local recurrence, 5/80 (1.22%) | 3 (13.04%) | 2 (3.51%) | |
Comparison of the clinical characteristics of the lesions by location highlighted that those on the head and neck develop at younger ages (47.1 [SD, 13.78] vs. 65 [14.88]; P=.001) and that no lesions at this location were described as erythematous (vs. 36.37% at the other sites [P=.007]).
DiscussionPoroma is a relatively common tumor that is not associated with ethnicity.2,3 It usually appears in middle or old age5 and more frequently affects males (1.5:1).2,3,5 Consistent with these data from the literature, our study showed that the median age of affected patients was 62.5 years and that males accounted for 61.3% of cases (1.6:1).
According to most dermatology texts, poroma can be found on any part of the body surface, although it is very common on the soles and palms,2,3,6 in contrast with other adnexal tumors, which tend to be concentrated in the area of the head and neck.3 Some authors report it to be located in the distal areas of the limbs in 65% of cases.7 However, others report it to be less common on the palms and soles. In one study of 101 patients, only 33% of lesions were on the palms and soles (11 and 22, respectively).5 In line with this study, we found 23 poromas on acral skin (5 on the palms and 18 on the soles [28.8%]). While these data suggest that acral skin is not as frequently affected as previously thought, this tumor clearly has a predilection for palmoplantar skin, since approximately 30% of poromas affect a relatively small area of skin compared with the total body surface. This predilection could be explained by the high density of eccrine glands on palmoplantar skin.
According to the literature, poroma can present as a very superficial lesion in the form of a plaque or as a papular or nodular exophytic lesion.2 It is normally flesh-colored, pinkish, or brownish, with a smooth, verrucous, or—occasionally—ulcerated surface.8 The lesion generally appears in isolation and grows slowly, reaching 1–2cm in diameter.3 It may be pigmented. In our series, only 3 cases were reported to be pigmented in the clinical history, and the clinical differential diagnosis included melanocytic nevus and/or melanoma. Betti et al.5 reported most lesions to be erythematous.5 We found the lesions to be erythematous in 24 cases (30%), especially those located on acral skin. Some studies highlight that poromas can be painful,2,6 as reported in 10 clinical histories in our series (12.5%).
Given that the differential diagnosis is broad, poroma cannot always be diagnosed clinically; the lesions that are most likely to be diagnosed correctly are those on the palms and soles.5 In our study, most correctly diagnosed tumors were on the acral skin and erythematous. Dermoscopy can prove particularly useful for the diagnosis of nonacral lesions, with the characteristic finding being a polymorphous vascular pattern comprising irregular linear vessels, red lacunae, glomerular vessels, and hairpin vessels.9 However, various types of vessels are also seen in squamous cell carcinoma, amelanotic melanoma, and porocarcinoma.9
Several cases of multiple poromas (poromatosis) have been reported, especially in patients with lymphoma or leukemia. In some cases, the tumor developed on previously irradiated skin, and in others after chemotherapy.10 Multiple poromas can be limited to acral skin or generalized.10 They have also been reported in pregnancy.11 In our study, we did not detect any cases of multiple lesions.
Malignant transformation of poroma can lead to porocarcinoma. Robson et al.12 reported that 18% of porocarcinomas appeared on a pre-existing poroma. Malignant transformation of a poroma is thought to occur after a mean period of 8.5 years.13 Nevertheless, the risk of malignant transformation is very low; therefore, it is not considered necessary to inform the patient of this risk.2
It was recently noted that nuclear protein in testis is expressed in immunohistochemistry in 32% of poromas and porocarcinomas, especially poroid hidradenoma and hidradenocarcinoma, whereas it is negative in other adnexal tumors.14
The treatment of choice is surgical resection, although destruction of the lesion by cryotherapy or electrocoagulation can prove useful in superficial cases.2,3
Our study is limited by its observational retrospective design and the small number of patients.
In summary, while poromas are particularly common on acral skin, they were found at other anatomical sites in most of the patients in our study. Poromas are benign tumors that present as exophytic erythematous lesions on palmoplantar skin. In these cases, diagnosis can be based on clinical findings. At other sites, however, they may take on very varied clinical forms, with a very broad differential diagnosis and more difficult clinical diagnosis.
FundingThe authors declare that no funding was received for the present study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.