Photodynamic therapy (PDT) has been shown to be useful and effective in the treatment of actinic keratosis, Bowen disease, and basal cell carcinoma. We present a series of 13 Bowen disease lesions treated using PDT. Complete responses were achieved in 11 (84%) of the lesions after 3 months of treatment; at 18 months, complete responses were seen in 9 (70%) of the lesions. Patients who presented a partial response or recurrence were treated with topical 5% imiquimod and achieved complete responses. The lesions that presented partial response or recurrence were the largest lesions, between 3 and 5cm in diameter. PDT in monotherapy or combined sequentially with imiquimod is an excellent and well-tolerated therapeutic option for Bowen disease. The treatment has few adverse effects and shows satisfactory results, particularly in multiple large lesions in areas of difficult surgical reconstruction or in elderly patients with a high surgical risk.
La terapia fotodinámica (TFD) ha demostrado ser un tratamiento útil y eficaz en queratosis actínicas, enfermedad de Bowen (EB) y carcinoma basocelular. Presentamos una serie de 13 lesiones de EB tratados con TFD. A los 3 meses del tratamiento 11/13 (84%) lesiones presentaron respuesta completa. A los 18 meses la respuesta completa fue de 9/13 (70%) lesiones. Los pacientes que presentaron respuesta parcial o recidiva fueron tratados con imiquimod tópico al 5%, con la consiguiente respuesta completa. Las lesiones con respuesta parcial o recidiva fueron las de mayor tamaño: entre 3 y 5cm de diámetro. La TFD en monoterapia o combinada secuencialmente con imiquimod es una excelente opción terapéutica para la EB, bien tolerada, con mínimos efectos secundarios y unos resultados satisfactorios, y sobre todo indicada en lesiones de gran tamaño, múltiples, en áreas de difícil reconstrucción quirúrgica o en pacientes ancianos con riesgo quirúrgico elevado.
Bowen disease (BD) is a squamous cell carcinoma (SCC) in situ. It typically affects elderly patients and usually manifests as a slow-growing solitary erythematous, scaling plaque that can reach a considerable size. Lesions are mainly located on the head, the neck, or the extremities.
Several treatment options exist, including surgery, electrocoagulation, cryotherapy, 5-fluorouacil, 5% imiquimod, laser therapy, radiation therapy, and photodynamic therapy (PDT).1
PDT is approved for the treatment of actinic keratosis, superficial and nodular basal cell carcinoma (BCC), and BD. It is a simple technique, suitable for outpatient use, and has proven to be both useful and effective in BD.
Topical 5% imiquimod has also been used in the treatment of BD. It has been combined with PDT to treat diverse forms of non-melanoma skin cancer, including BD, and the combination appears to have a synergic effect.
We present a series of 13 BD lesions treated with PDT or with PDT and topical imiquimod at our department.
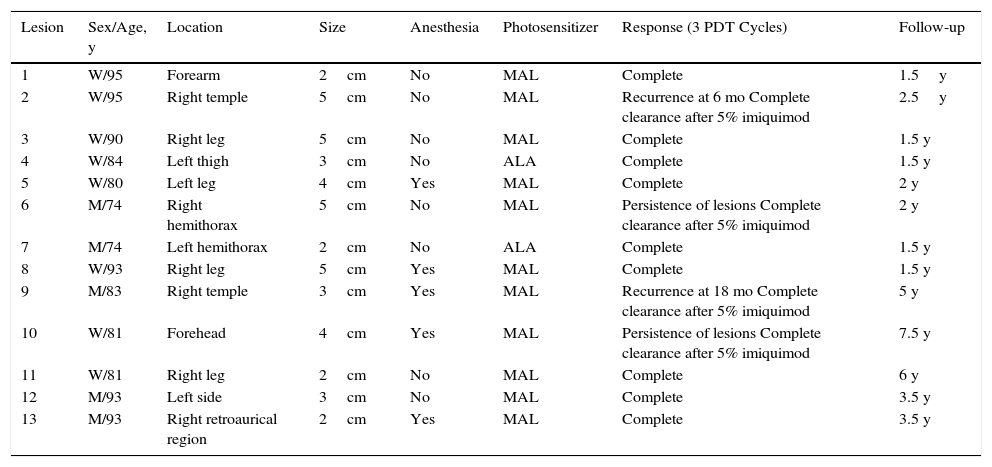
Case DescriptionsTable 1 summarizes the characteristics of the 13 lesions treated with PDT at our department. The lesions corresponded to 10 patients (7 women and 3 men) and they were all biopsied to confirm diagnosis and in some cases to investigate suspected cases of partial clearance or recurrence.
Clinical Characteristics of Bowen Disease Lesions Treated With PDT at Our Department.
| Lesion | Sex/Age, y | Location | Size | Anesthesia | Photosensitizer | Response (3 PDT Cycles) | Follow-up |
|---|---|---|---|---|---|---|---|
| 1 | W/95 | Forearm | 2cm | No | MAL | Complete | 1.5y |
| 2 | W/95 | Right temple | 5cm | No | MAL | Recurrence at 6 mo Complete clearance after 5% imiquimod | 2.5y |
| 3 | W/90 | Right leg | 5cm | No | MAL | Complete | 1.5 y |
| 4 | W/84 | Left thigh | 3cm | No | ALA | Complete | 1.5 y |
| 5 | W/80 | Left leg | 4cm | Yes | MAL | Complete | 2 y |
| 6 | M/74 | Right hemithorax | 5cm | No | MAL | Persistence of lesions Complete clearance after 5% imiquimod | 2 y |
| 7 | M/74 | Left hemithorax | 2cm | No | ALA | Complete | 1.5 y |
| 8 | W/93 | Right leg | 5cm | Yes | MAL | Complete | 1.5 y |
| 9 | M/83 | Right temple | 3cm | Yes | MAL | Recurrence at 18 mo Complete clearance after 5% imiquimod | 5 y |
| 10 | W/81 | Forehead | 4cm | Yes | MAL | Persistence of lesions Complete clearance after 5% imiquimod | 7.5 y |
| 11 | W/81 | Right leg | 2cm | No | MAL | Complete | 6 y |
| 12 | M/93 | Left side | 3cm | No | MAL | Complete | 3.5 y |
| 13 | M/93 | Right retroaurical region | 2cm | Yes | MAL | Complete | 3.5 y |
Abbreviations: ALA, aminolevulinic acid; M, man; MAL, methyl aminolevulinate; PDT, photodynamic therapy; W, woman.
Eleven lesions were treated with methyl aminolevulinate (MAL) 160mg/g cream and 2 were treated with a 5-aminolevulinic acid (ALA) 78mg/g nanoemulsion-based gel. The same PDT protocol was used in all cases. Following curettage of the area, the photosensitizing agent was applied to the lesion, which was covered with an occlusive dressing for 3hours before illumination. The lesions were irradiated with red light (PDT 1200L, Waldmann) at a wavelength of between 580 and 760nm (dose, 75J/cm2; fluence, 69-75mw/cm2). All the patients were treated with 3 sessions, each separated by a week. The lesions were photographed before and after treatment. Patients with recurrent lesions or lesions that only partially cleared were treated with 5% imiquimod applied 5 times a week for 6 weeks.
The mean age of the patients was 85.4 years. The most common locations were the lower limbs (38%), the head (31%), the trunk (24%), and the upper limbs (7%).
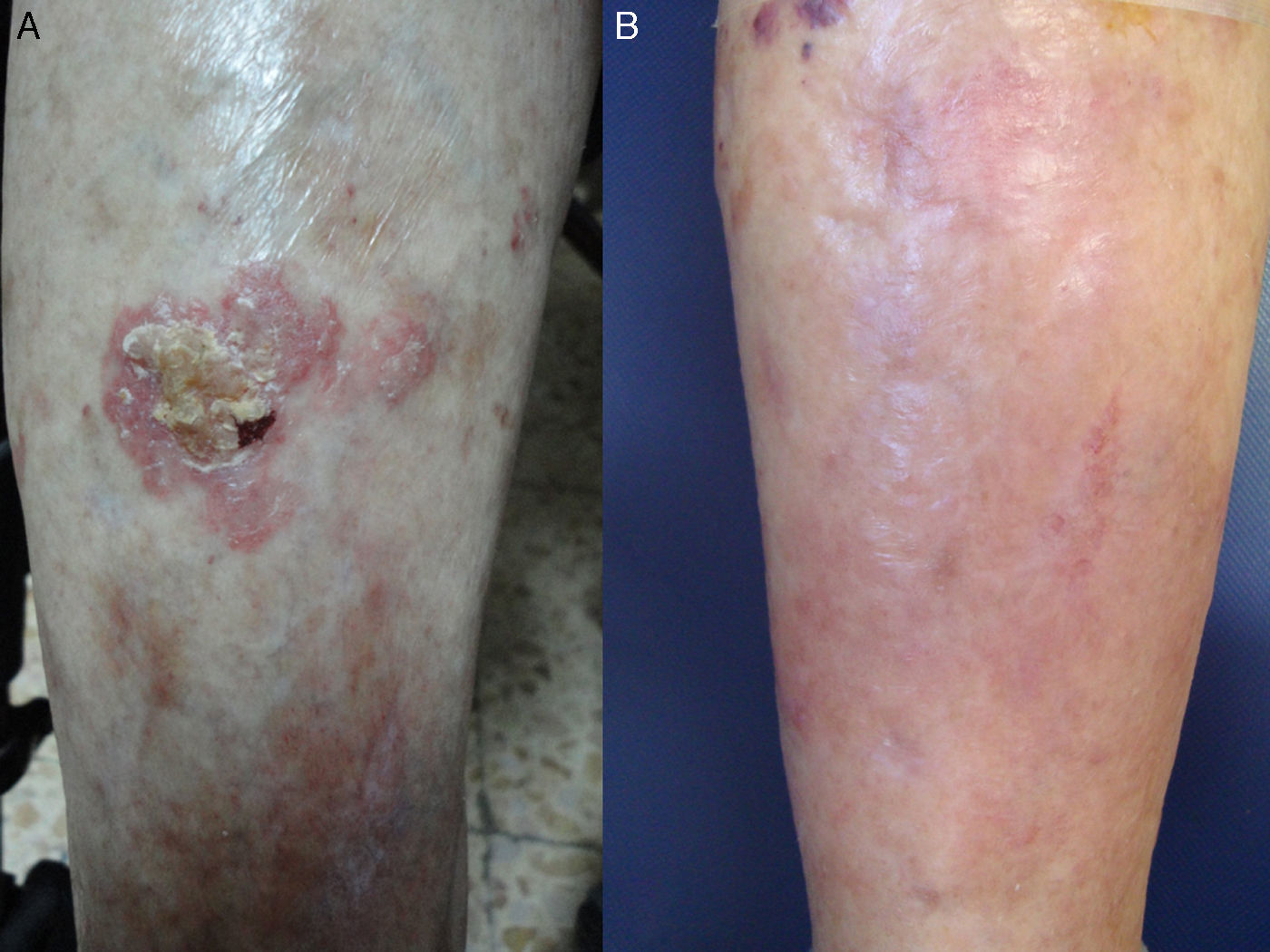
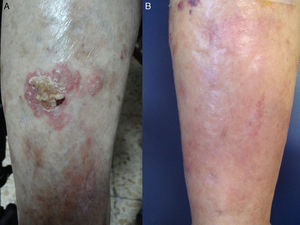
Most patients had a history of prolonged sun exposure and 1 patient, a radiologist, had been chronically exposed to ionizing radiation at work. Seven (70%) of the 10 patients had a history of nonmelanoma skin cancer. One patient also had a systemic lymphoma being treated with chemotherapy (Fig. 1). Most of the lesions were large (mean diameter, >3.5cm).
A, Bowen disease lesion on the anterior surface of the right leg of a 90-year-old woman with systemic lymphoma being treated with chemotherapy. B, Complete clearance of lesion after 3 cycles of photodynamic therapy with methyl aminolevulinate. No recurrences were detected during follow-up.
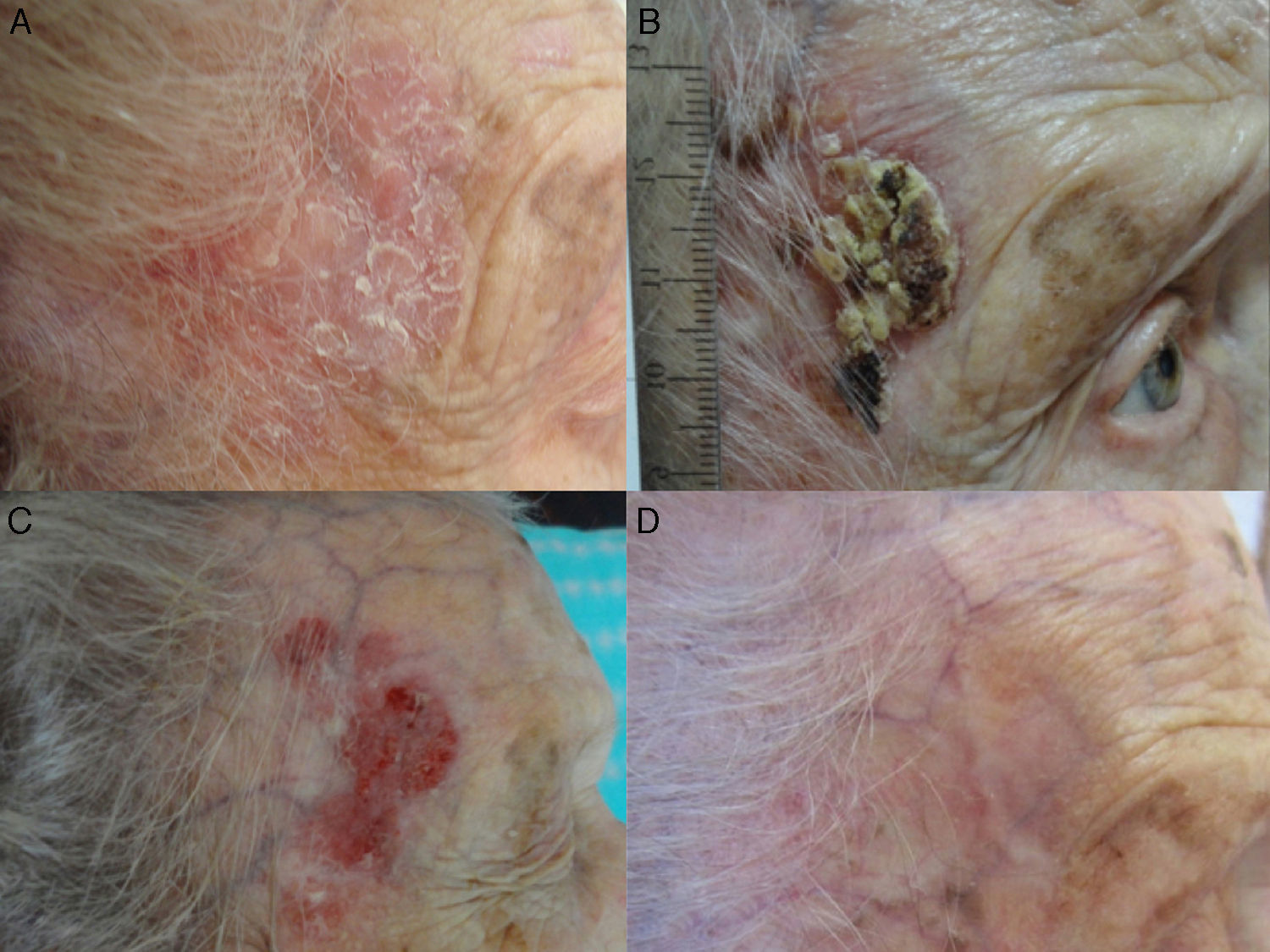
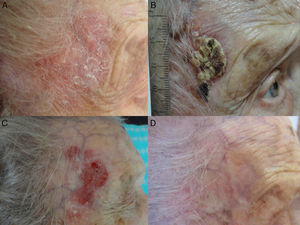
Treatment response was evaluated at 3 and 18 months. At the 3-month evaluation, 11 of the 13 lesions (84.6%) had cleared completely, while the other 2 (15.4%) showed partial clearance. At the 18-month follow-up, 2 recurrences (18.1%) were detected among the 11 lesions that had initially cleared. The 2 recurrent lesions and the 2 that had responded only partially to PDT were treated with imiquimod. They all cleared completely (Fig. 2) and had not recurred at the time of writing. The 4 lesions were all large (5cm, 4.5cm, 4cm, and 3cm); 2 were located on the face, 1 on the leg, and another on the chest.
A, Large Bowen disease lesion on the right temple of a 95-year-old woman. The lesion was treated with 3 sessions of photodynamic therapy with methyl aminolevulinate and cleared completely within 3 months. B, The patient developed a crusted lesion in the same area 6 months after treatment. Recurrence was confirmed by biopsy following removal of the crust. C, Treatment with topical 5% imiquimod was started. D, The treatment resulted in complete clearance and no recurrences were detected during follow-up.
The most common adverse effect during PDT was pain, which was rated with a mean score of 5.2 on a visual analog scale of 1 to 10. None of the treatments had to be interrupted due to pain. Some patients were administered local anesthesia. Transient swelling and redness were also observed after illumination.
Sequelae consisted of hyperpigmentation or hypopigmentation of the treated area. The cosmetic results were very good (Fig. 3) and the patients were all very satisfied with the outcome.
A, Bowen disease lesion that would have been difficult to treat surgically on the posterior surface of the left leg in an 80-year-old woman. B, Complete clearance of the lesion after 3 cycles of photodynamic therapy with methyl aminolevulinate. No evidence of sequelae or recurrence was detected during follow-up.
Mean follow-up was 3 years (range, 18 months-7.5 years).
DiscussionWe have reported on a series of patients with BD treated with PDT or with PDT and 5% imiquimod in the case of partial response or recurrence.
BD is an intradermal SCC. The risk of progression to invasive SCC has been estimated at between 3% and 8%, but it may be higher in the case of genital involvement (erythroplasia of Queyrat).2,3
PDT was approved for the treatment of BD in 2006. According to European guidelines, its use is supported by a level of evidence I and a strength-of-recommendation grade A. It is classified as a good or very good option for the treatment of large lesions, multiple lesions (which may need to be treated simultaneously), lesions in areas where surgical reconstruction is complicated, lesions in elderly patients with a high surgical risk, and lesions in immunosuppressed patients with altered wound healing.4
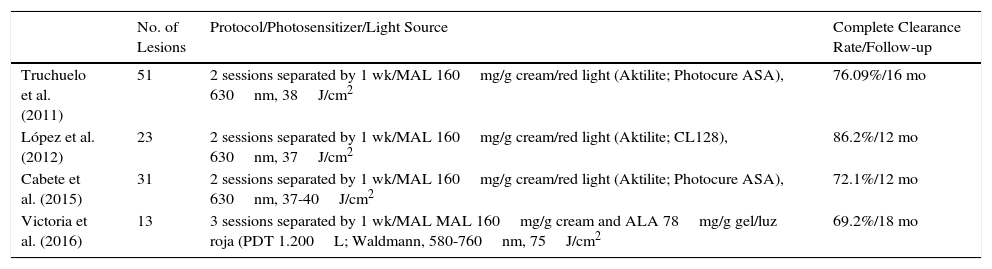
Several studies have shown that PDT is more effective and has fewer adverse effects than other nonsurgical alternatives.5 Complete clearance rates of 86% to 93% were reported at 3 months following 1 or 2 cycles (separated by a week) of PDT with MAL, and sustained clearance rates at 24 months ranged from 68% to 71%. One study reported a clearance rate of 76% at 16 months following 2 sessions of PDT with MAL.6 Our findings support previous reports of lower complete clearance rates in larger lesions.7,8 A recent study of 31 BD lesions and 44 superficial BCC lesions treated with PDT reported a recurrence rate of 53.8% for BD and 33.3% for BCC after a mean follow-up of 43.5 months.9 The risk of recurrence was higher in BD than in BCC and also in younger patients. Long-term follow-up is therefore advisable, as late recurrence, which typically affects small areas and is easy to treat, is a possibility (Table 2).
Summary of Other Series in the Literature Describing the Treatment of Bowen Disease With Photodynamic Therapy.
| No. of Lesions | Protocol/Photosensitizer/Light Source | Complete Clearance Rate/Follow-up | |
|---|---|---|---|
| Truchuelo et al. (2011) | 51 | 2 sessions separated by 1 wk/MAL 160mg/g cream/red light (Aktilite; Photocure ASA), 630nm, 38J/cm2 | 76.09%/16 mo |
| López et al. (2012) | 23 | 2 sessions separated by 1 wk/MAL 160mg/g cream/red light (Aktilite; CL128), 630nm, 37J/cm2 | 86.2%/12 mo |
| Cabete et al. (2015) | 31 | 2 sessions separated by 1 wk/MAL 160mg/g cream/red light (Aktilite; Photocure ASA), 630nm, 37-40J/cm2 | 72.1%/12 mo |
| Victoria et al. (2016) | 13 | 3 sessions separated by 1 wk/MAL MAL 160mg/g cream and ALA 78mg/g gel/luz roja (PDT 1.200L; Waldmann, 580-760nm, 75J/cm2 | 69.2%/18 mo |
There are no standardized PDT protocols for BD.10 This makes it difficult to compare results, as the protocols described to date have numerous differences, including type of photosensitizing agent used, interval between application of agent and irradiation, type of illumination, and number of sessions. Protocols typically consist of 2 PDT sessions separated by a week and the use of red light with a continuous spectrum of 570 to 670nm and a total dose of 75 to 200J/cm2 or a narrower spectrum, around 630nm, and a dose of approximately 37J/cm2. Although 4 sessions have been used in some series, we opted for 3 sessions separated by a week. If we compare our results with those described for 2 sessions, however, the 3-session protocol did not result in higher complete clearance rates.
Complete clearance rates of 73% to 93% have been reported for 5% imiquimod cream in the treatment of BD. Sequential PDT and imiquimod has been used successfully to treat actinic keratosis,11 basal cell carcinoma,12 vulvar intraepithelial neoplasia,13 and more recently some cases of BD.11,14 The mechanism of action underlying the combined treatment is unclear, although it is thought that the residual inflammation associated with PDT may help to activate innate immunity induced by imiquimod, improving the recruitment of effector cells activated in the tumor tissue,15 as occurs in cryoimmunotherapy.
In conclusion, PDT is an excellent treatment option for BD, particularly in patients with larger or multiple lesions or elderly patients with a high surgical risk. In our experience, the sequential use of PDT and imiquimod induces improved clinical and histologic response. Both treatments are well tolerated, cause minimum adverse effects, and produce satisfactory cosmetic outcomes.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that no private patient data appear in this article.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Victoria-Martínez AM, Martínez-Leborans L, Ortiz-Salvador JM, Pérez-Ferriols A. Tratamiento de la enfermedad de Bowen con terapia fotodinámica y ventajas de la aplicación secuencial de imiquimod tópico. Actas Dermosifiliogr. 2017;108:e9–e14.