There are a number of approaches for the repair of scalp defects, including local, regional, and distant options. The use of a local double triangular hatchet flap has numerous advantages due to its mixed rotational and advancement components, its large size, and the possibility of maintaining the cosmetic appearance of the hairline as the flap has similar characteristics to those of the area to be reconstructed. We present our experience with a series of skin tumors of the scalp. After oncologic excision, immediate repair of the defect was performed using this double flap. The surgical technique and the advantages of this type of reconstruction are discussed. We believe that the hatchet flap is an ideal option for the reconstruction of moderate-sized scalp defects.
Los defectos localizados a nivel del cuero cabelludo pueden reconstruirse mediante diversas opciones terapéuticas, de carácter local, regional o a distancia. El empleo de un doble colgajo local triangular en hacha aporta múltiples ventajas en la cobertura de estos defectos, debido a su componente mixto, tanto rotatorio como de avance, sus considerables dimensiones y la posibilidad de mantener la estética de la línea capilar, aportando similares características al territorio a reconstruir.
Presentamos nuestra experiencia en una serie de tumores cutáneos en el cuero cabelludo, en los que tras su exéresis oncológica se realizó la reconstrucción inmediata del defecto resultante mediante este doble colgajo, discutiéndose la técnica quirúrgica y las ventajas de este tipo de reconstrucción, para concluir su idoneidad como opción reconstructiva en defectos moderados del cuero cabelludo.
There are many, well-defined approaches for the repair of the different types of head and neck skin defects that can result from the resection of skin tumors; these repairs will vary according to the site, size, type, and degree of invasion of the tumor.
We would like to draw particular attention to the potential of the double hatchet flap. First described by Emmet1 in 1977, the hatchet flap is a triangular local rotation flap, with a greater or lesser degree of advancement and with a back cut at the base of the flap, through which it derives its vascular supply.This is a very versatile type of flap that can be used to repair defects anywhere on the body; for example, it is particularly appropriate for use on the limbs and after excision of the pulp of a finger or toe.2 For lesions in the craniofacial territory, it is useful for repairs of the frontal and temporal regions.3–5
The double-flap technique, with 2 flaps arranged one on either side of a given defect, is a reliable method for the repair of small and moderate-sized defects of the scalp. We consider it a good reconstruction technique for these cases, particularly when evaluating the possibility for coverage by means of local options, when it is not possible to use skin grafts (for example, oncologic surgery that requires deperiostization, which will not leave an adequate receptor bed) or other more complex options, such as microvascular free flaps. The minimal morbidity associated with the hatchet flap means that the procedure can be performed as ambulatory surgery or, when used for large defects, with only a single day of hospital admission. The ease of its design, the speed of its performance, the simple postoperative follow-up, and patient comfort (rapid healing, ease of wound care, and the absence of a donor site and of distant sequelae) make the double hatchet flap an ideal option.
Case DescriptionsBetween November 2008 and January 2011 we used the double hatchet flap to repair 20 scalp defects after oncologic surgery. In all cases the tumor was excised with adequate resection margins, and immediate postoncologic-surgery repair was performed. There were no significant complications (partial or total flap necrosis of arterial or venous etiology, hematomas, wound dehiscence) in any of the patients during the immediate or late postoperative periods. The underlying periostium was systematically preserved when oncologic surgery did not require its excision.
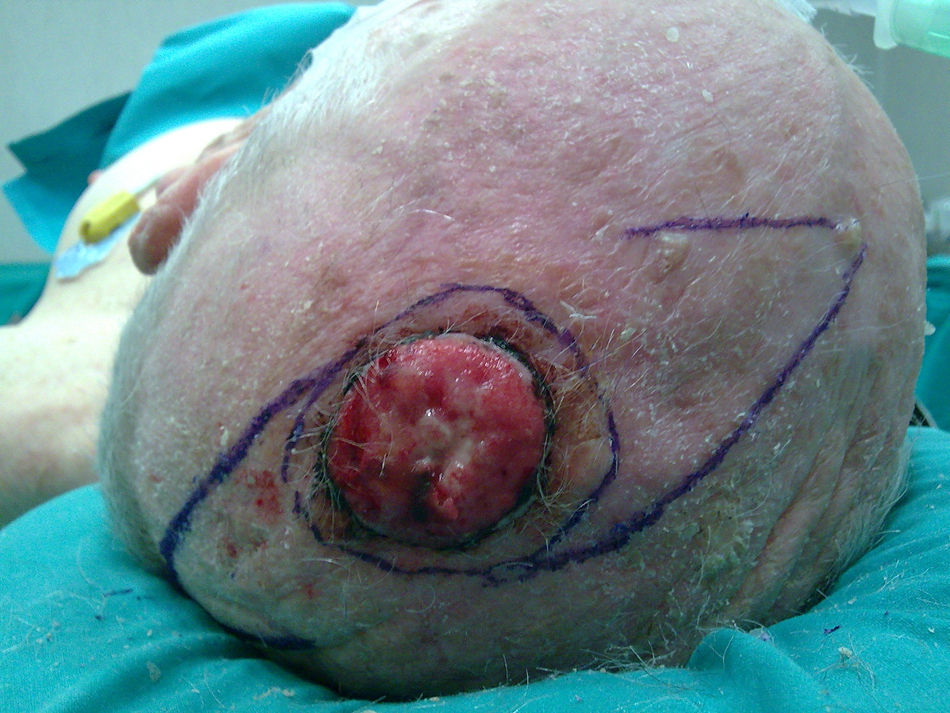
The majority of patients treated were men over 70 years of age (mean age, 76 years) with scalp lesions of 3 to 7cm in diameter (mean, 4cm). The lesions were clinically and histopathologically compatible with squamous cell carcinoma and most were located on the vertex or parietal region of the cranium (Figs. 1 and 2).
After excision of the lesion, with or without resection of the periostium, depending on oncologic requirements, the random-pattern double hatchet flaps were fashioned on either side of the lesion; the length of each flap was approximately 1.5 times the diameter of the initial defect and the width of the skin pedicle was equivalent to the radius of the defect. Dissection of the flap was performed in the subgaleal plane, preserving the rich supragaleal vascular network (and maintaining the periostium intact to facilitate reconstruction if necrosis of the flap should occur). The flaps were rotated and advanced, with release of the adjacent tissues along the same plane. The site of apposition of the 2 flaps, in the midline of the area of the defect to be repaired, was closed by tissue planes, and the donor areas of the flaps in V-to-Y fashion (Fig. 3). In large repairs, we favor leaving a drain for the first 24 hours.
The results 1 month after the operation show that a stable repair is achieved, with a cosmetic result that we have not been able to better using other reconstruction techniques in defects of these sizes (Fig. 4).
DiscussionThe double hatchet flap enables small or moderate-sized defects of the scalp to be covered in a single surgical session, providing tissue of the same characteristics as the area of the defect, with minimal morbidity of the donor site.
With regard to the general surgical technique for reconstructions with this type of flap, the excision of the skin lesions must be performed with a circular incision with adequate margins. To design the 2 flaps, the size of the defect left by the excision is measured (the maximum length of each flap is equivalent to 1.5 times the diameter of the defect, and the width of the pedicle of each flap is equivalent to 0.5 times that diameter).3 The dissection of the flap must be performed in the deep subcutaneous plane, preserving the vascularization from the subdermal plexus, after which the flaps are rotated until their advancement borders meet, and the distal area of the defect is closed in V-to-Y fashion.
When using this technique on the scalp, the plane of dissection is modified and is typically subgaleal in order to preserve the supragaleal vascularization. This form of dissection, with preservation of the galea aponeurotica, means that the flap is less elastic and that there is a greater need for advancement and rotation, as well as extensive release of the surrounding skin in order to distribute the tension of closure of the wound. The appearance of any deformity in the immediate postoperative period is uncommon.6 If deformity develops, it usually resolves in less than 2 months without the need for further surgery.
In small defects, the excision and reconstruction can be performed as ambulatory surgery under local anesthesia. In moderate or large defects, we recommend performing the operation under local anesthesia and sedation, or even under general anesthesia in selected patients. In such cases, hospital admission is required for postoperative monitoring (usually for 24 hours). Patients are seen every week for the first 3 weeks, until removal of the sutures, and then every 3 months as part of standard oncologic follow-up.
Because of the mixed movement component and the extensive coverage that reconstruction with this type of flap can offer, we consider it to be ideal to cover scalp defects in general and those of the central area in particular.7,8 Its constant and sufficient vascular supply together with the adaptability of the design of the flap, allowing the hairline to be preserved, provides an excellent cosmetic result with tissue of the same characteristics as the defect in terms of thickness, texture, and hair. Furthermore, compared to other options, such as skin grafts or microvascular free flaps, this technique offers the advantage of more stable coverage and a saving in terms of days of hospital stay (in addition to the advantage that this represents in elderly patients), postoperative follow-up, and ease of outpatient wound care.
In conclusion, the use of the double hatchet flap is proposed as a valuable technique for the reconstruction of scalp defects.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández-Calderón M, Casado-Sánchez C, Cabrera-Sánchez E, Casado-Pérez C. Versatilidad de colgajos en hacha en defectos del cuero cabelludo. Actas Dermosifiliogr.2012;103:629-631.