Vogt-Koyanagi-Harada disease is a rare condition that is characterized by bilateral uveitis, meningitis, auditory symptoms, and skin disorders such as vitiligo, poliosis, and alopecia.1 This report aims to draw attention to a condition that is widely discussed in the literature yet unfamiliar to dermatologists.
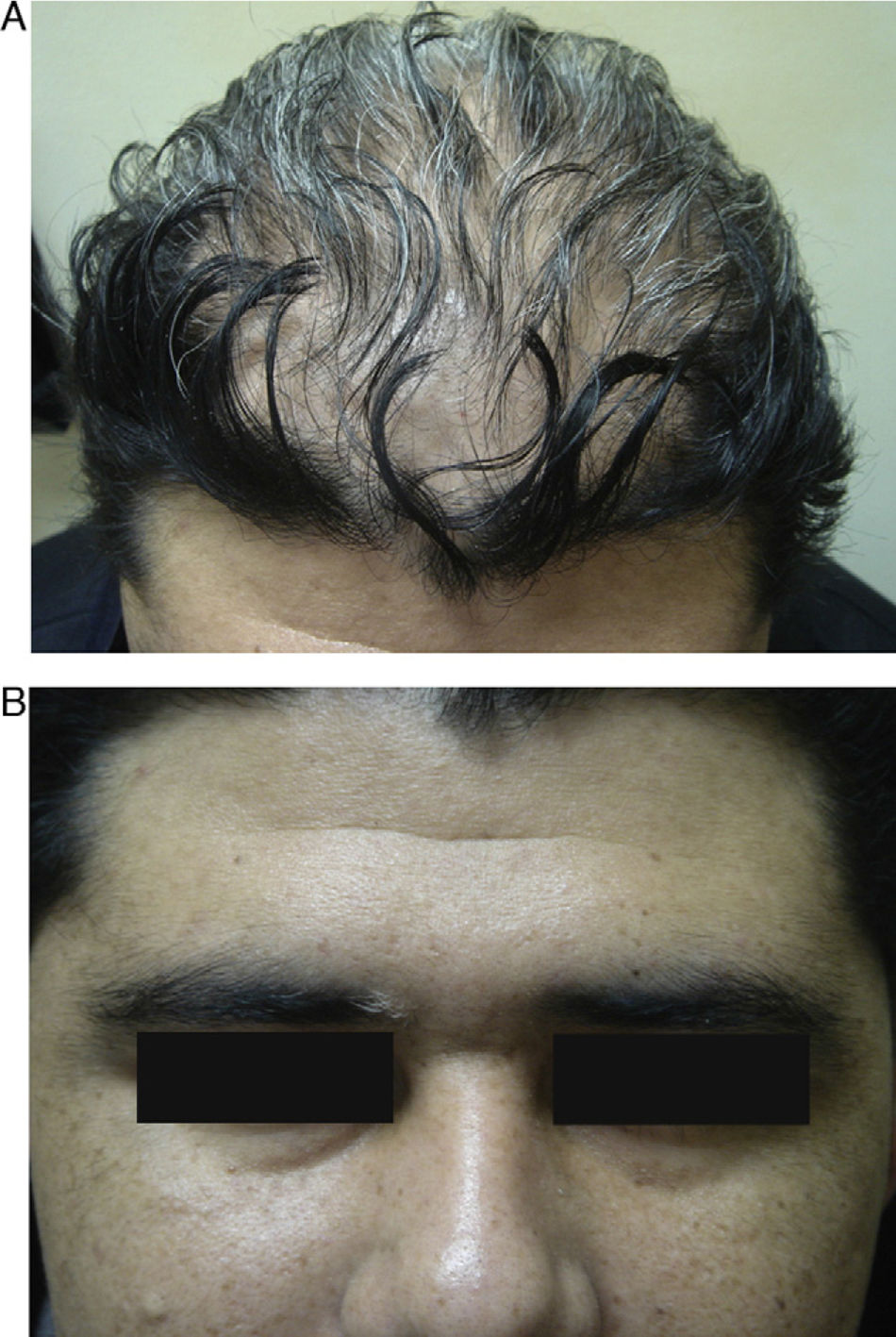
We present the case of a 37-year-old man from Bolivia who was seen in the emergency department with vertigo, headache, eye pain, and loss of vision in both eyes that had begun a week earlier. Three months later he was referred to the dermatology department with rapid-onset alopecia of the scalp. Physical examination revealed horizontal rotatory nystagmus at rest and on looking upward and to the right. Ophthalmological examination revealed a marked loss of visual acuity in both eyes; anterior pole biomicroscopy revealed Tyndall phenomenon with posterior synechiae (Fig. 1). Nonscarring diffuse alopecia was also observed on the scalp, together with poliosis of the right eyebrow (Fig. 2, A and B). The results of the blood workup—complete blood count, biochemistry, clotting, protein analysis, antibodies to antinuclear antigen and extractable nuclear antigen, serology for syphilis and viruses (hepatitis A, B, and C viruses; human immunodeficiency virus; Epstein-Barr virus; cytomegalovirus), and thyroid hormones—were negative or normal. Cerebral magnetic resonance imaging ruled out meningeal or encephalic disease. Histocompatibility testing was positive for HLA-DR4 and HLA-DR53. These findings enabled a diagnosis of Vogt-Koyanagi-Harada disease to be confirmed. Treatment with intravenous methylprednisolone (1g) was prescribed for 3 days, with subsequent oral administration tapered over 12 weeks. The patient's clinical condition improved considerably, not only in terms of systemic manifestations, but also with complete resolution of the alopecia. However, the new hair remained whitish-gray in color (Fig. 3).
Vogt-Koyanagi-Harada disease, which was first reported in 1951, is a rare systemic inflammatory disorder mediated by T lymphocytes acting against pigmented cells in the uvea, skin, inner ear, and leptomeninges.1
It has an incidence of 6.5 cases per million and is more common in Hispanic and Native American individuals and Asian women aged between 20 and 50 years. Although its etiology is unknown, immunogenetic analysis suggests a strong association with some HLA antigens (DR4, DRB1, and DR53) and genes of the tyrosinase family that cause susceptibility to the disease.2 It is associated with various infectious diseases and other disorders whose pathogenic mechanisms are of immunological origin, such as autoimmune thyroid disease, psoriasis, linear immunoglobulin A bullous dermatosis, and inflammatory vitiligo as a consequence of the destruction of melanocytes by cytotoxic CD8+ T lymphocytes.2–4
Diagnosis is based essentially on clinical manifestations, as there are no specific confirmatory tests, and the diagnostic criteria include dermatologic findings (alopecia, poliosis, and vitiligo) (Table 1). Typical extracutaneous clinical manifestations include disorders of the eyes (bilateral granulomatous uveitis, retinal detachment, and loss of vision) and neurological and auditory conditions (headache, aseptic meningitis, vertigo, nystagmus, and hypoacusis).5
Diagnostic Criteria of Vogt-Koyanagi-Harada Disease.
| Major Criteria |
| 1. No history of penetrating eye trauma or surgery before the episode of uveitis |
| 2. No clinical or analytical evidence suggestive of other eye diseases |
| 3. Bilateral ocular involvement (choroiditis, uveitis, inflammatory vitreous reaction, serous retinal detachment) |
| 4. Neurological and auditory findings (meningism, tinnitus, pleocytosis in cerebrospinal fluid) |
| 5. Dermatologic findings (alopecia, poliosis, vitiligo) |
| 6. Hypoxia |
| 7. Central nervous system depression |
| 8. Petechiae |
| Minor Criteria |
| 9. Tachycardia (>120 beats per minute) |
| 10. Fever (temperature >39°C) |
| 11. Unexplained anemia |
| 12. Thrombocytopenia (platelet count <150×109/L) |
Alopecia can be seen in 70% of cases within weeks or months after the onset of ocular symptoms. It resolves completely after a variable period. Alopecia and the poliosis traditionally reported by ophthalmologists were recently considered to be alopecia areata with subsequent growth of white hair.6 Vitiligo affects almost half of all cases; it is often symmetrical and the pigmentary changes may be permanent.
Early high-dose systemic corticosteroids are the treatment of choice in patients with active Vogt-Koyanagi-Harada disease. In cases of recurrent or corticosteroid-refractory disease, other immunosuppressive agents such as ciclosporin, cyclophosphamide, or azathioprine can be added to the treatment. A favorable response has been reported with adalimumab and rituximab in refractory cases.7 Prognosis is relatively benign, and although the most common complications are visual, total blindness is now rare. Patients may also experience personality disorders, psychosis, and deafness, as occurred in the Spanish painter Francisco de Goya when creating his famous black paintings.8
We are grateful to our colleagues from the dermatology and ophthalmology departments who participated in the diagnosis and management of the patients.
Please cite this article as: Hernández-Bel P, et al. Enfermedad de Vogt-Koyanagi-Harada. Una entidad poco conocida para el dermatólogo. Actas Dermosifiliogr. 2013;104:529-31.