A 70-year-old woman with a history of bilateral breast carcinoma was seen for a bluish lesion on the dorsum of the right foot that had appeared during adolescence. The patient reported the recent appearance of a more pigmented area in the distal portion of the lesion. She experienced no pain, itching, or other accompanying symptoms. She reported no trauma or any personal or family history of melanoma.
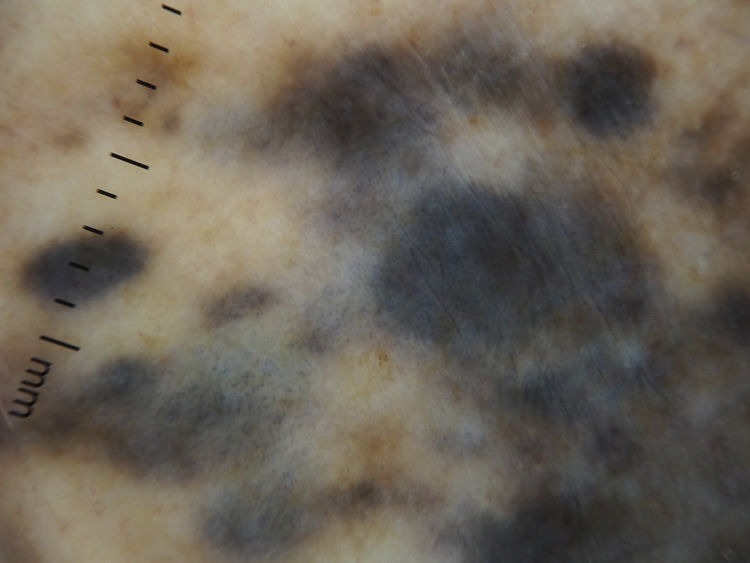
Physical ExaminationExamination revealed a linear plaque of 10 cm in diameter on the dorsum of the right foot consisting of multiple well-defined, bluish, rounded papules, one of which, located in the distal area of the lesion, measured 5 mm and had a blacker coloration (Fig. 1). Dermoscopy revealed multiple grouped areas of dark blue–gray pigmentation (Fig. 2). Neither the inguinal nor axillary lymph nodes were palpable.
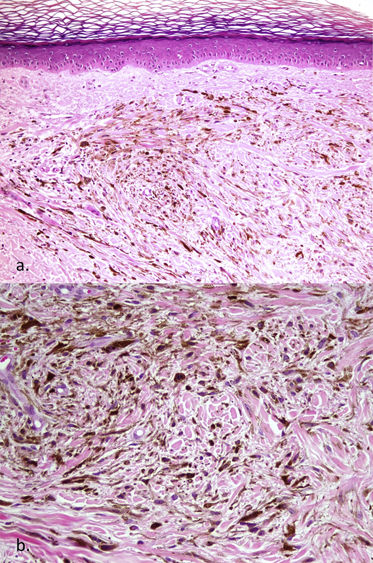
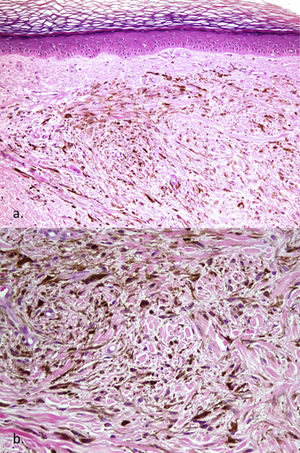
HistopathologyHistopathology showed a dermal proliferation of spindle-shaped melanocytes without cytological or architectural atypia, with marked pigmentation. These cells were accompanied by melanophages and penetrated the dermal collagen. The observed lesion exclusively affected the dermis. There was no evidence of nevic proliferation at the dermoepidermal junction, either in the form of theca cells or lentiginous proliferation. No mitotic figures were observed (Fig. 3).
What is your diagnosis?
DiagnosisAgminated or plaque-type blue nevus.
Clinical Course and TreatmentGiven the extension of the lesion and the absence of criteria indicating malignancy, it was decided to carry out regular monitoring.
CommentBlue nevi are dermal melanocytic proliferations that generally appear as small, dark-blue, solitary macules or papules. When these lesions group together, they tend to do so linearly, following a Blaschkoid or segmental distribution.1 The Latin term agmen means “army” and refers to this rare group of smooth or raised nevi clustered in a well-circumscribed area,2 independent of their linear or segmental distribution.
In general, dermal melanocytes disappear during the second half of gestation, but some remain in the dermis of the scalp, the sacral region, and the dorsal aspect of the distal extremities, locations at which blue nevi occur more frequently. The blue coloration of these nevi is the result of the Tyndall effect, caused by the refraction of light striking the dermal melanocytes.3 Although the pathogenesis of agminated or plaque-type blue nevus is unknown, isolated cases have been described after skin trauma or sunburn, suggesting that these factors may stimulate melanocyte proliferation.3,4 Moreover, somatic activating mutations have been recently detected in GNAQ and GNA11, genes in which mutations have been previously identified in non-agminated blue nevi. Although similar mutations in GNAQ and GNA11 have been detected in mucosal melanoma, such mutations are not by themselves sufficient to trigger degeneration to melanoma, and a second mutational event is required to induce malignancy. The presence of other mutations has also been described in other pigmented lesions with an agminated distribution (e.g. nevus spilus, intradermal nevus), reflecting post-zygotic expression of mosaic mutations.1
Four histological forms of blue nevus are described: common; cellular; combined; and epithelioid, which is associated with Carney syndrome5.
The differential diagnosis should include melanoma on blue nevus (malignant blue nevus), metastatic melanoma, argyria, and vascular malformations, and the diagnosis should be based on clinical and histological findings.5
Agminated blue nevus usually follows an indolent course. However, increases in size and the development of new local lesions are common, and require regular monitoring. Cases associated with other pigmented lesions (nevus spilus, lentigos),6 dermatomyositis,7 and Carney complex8 have been described, without establishing clinical significance.9
Given the benign nature of this lesion, treatment is not required in the absence of changes, and clinical monitoring is sufficient.
FundingThis work has not received any type of funding.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gracia-Darder I, Montis-Palos MC, Martínez MA. Placa azulada en el dorso del pie. Actas Dermosifiliogr. 2021;112:913–914.