Erythema nodosum (EN) is the most frequent panniculitis and, although it can be idiopathic, it presents multiple causal processes. We performedade a retrospective, observational and descriptive study about causes of EN in patients admitted to a third-level Spanish hospital over a period of 11 years, and we compared the results obtained with those published in other studies. We compared the analytical markers of inflammation between inflammatory and noninflammatory causes of EN. The final cohort was composed of 52 patients, with 20% of idiopathic cases, 34% of cases secondary to infections and another 34% of cases secondary to autoimmune diseases. There were no cases secondary to drugs or lymphomas. We did not observe significant differences in the analytical parameters of inflammation between inflammatory and noninflammatory cause of EN.
El Eritema Nodoso (EN) es la paniculitis más frecuente y, aunque puede ser idiopático, presenta múltiples procesos causales. Elaboramos un estudio retrospectivo, observacional y descriptivo de las causas de EN en pacientes ingresados en un hospital español de tercer nivel durante un período de 11 años, y comparamos los resultados obtenidos con los publicados en otros trabajos. Comparamos los marcadores analíticos de inflamación entre causas inflamatorias y no inflamatorias de EN. La cohorte final quedó compuesta por 52 pacientes, con un 20% de casos idiopáticos, un 34% de casos secundarios a infecciones y otro 34% de casos secundarios a enfermedades autoinmunes. No hubo casos secundarios a fármacos o linfomas. No observamos diferencias significativas en los parámetros analíticos de inflamación en función de causa inflamatoria o no inflamatoria de EN.
Erythema nodosum (EN) is the most common form of panniculitis. It manifests as nonulcerated, deep, painful erythematous-violaceous nodules with a diameter of between 1 and 10 cm. Although the lesions are preferentially located on the anterior aspect of the legs, they are observed at other sites. EN resolves spontaneously in 2 to 8 weeks without leaving residual lesions. It can recur and is usually accompanied by fever, general malaise, and polyarthralgia. It is more common in women than men and its incidence is highest in the second to fourth decade of life.1–3
EN is the result of a delayed type IV hypersensitivity reaction, which can be triggered by different antigens. Histopathologic findings vary according to time since onset. Findings for early-stage lesions include edema and hemorrhage in the septa of the subcutaneous tissue and a neutrophilic infiltrate distributed between collagen bundles. Late-stage findings, by contrast, include septal fibrosis with periseptal granulation tissue and an inflammatory infiltrate composed of lymphocytes, histiocytes, and multinucleated giant cells. A hallmark histopathologic feature of EN is Miescher radial granulomas, which are nodular aggregates of histiocytes surrounded by neutrophils and arranged radially around blood vessels. These aggregates are located at the interface between the affected septum and fat lobules. Vasculitis and fat necrosis are absent in EN, and despite the marked fibrosis, lesions resolve completely within several weeks.3,4
Although a significant proportion of EN cases (17%-72%) are idiopathic, an association has been demonstrated for infections (streptococcal pharyngitis, tuberculosis, and yersiniosis), autoimmune diseases (sarcoidosis, inflammatory bowel disease [IBD], and Behçet disease), drugs (oral contraceptives and drugs containing sulfa), and pregnancy. Paraneoplastic EN has also been reported in lymphoma and leukemia.1–3
Wherever possible, the underlying cause should be treated. Targeted treatment and rest usually result in spontaneous resolution within a few weeks. Analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) can be used for symptomatic relief, but should be avoided in patients with Crohn disease. Other symptomatic treatments include potassium iodide, colchicine, hydroxychloroquine, and corticosteroids (once an infectious cause has been ruled out).4
As EN has multiple etiologies, the most frequent causes in different series can vary by geographic location, time of year, and healthcare setting. The aim of this study was to describe the main causes of EN in patients admitted to a tertiary care hospital in Spain and to compare our results with those reported in other series. We also compared blood inflammatory markers between patients with an inflammatory versus a noninflammatory cause.
Patients and MethodsRetrospective, observational, descriptive study of patients hospitalized for EN at Hospital Universitario 12 de Octubre in Madrid, Spain between January 1, 2005 and December 31, 2015. The patients were identified from the hospital’s discharge records. The diagnosis of EN was based on clinical and, where available, histopathological criteria. Etiologic factors were identified in the patients’ medical records as per the following definitions:
- -
Streptococcal pharyngitis: compatible clinical findings for the 6 weeks prior to the diagnosis of EN based on a McIsaac score of 4 or 5,5 a positive antistreptolysin A (ASO) test, or detection of Streptococcus pyogenes in the pharyngeal or tonsillar exudate.
- -
Latent tuberculosis infection: a positive Mantoux test (induration > 5 mm in unvaccinated patients and > 15 mm in vaccinated patients) in the absence of a clinically active infection or detection of mycobacteria.
- -
Tuberculosis: compatible clinical findings with radiographic evidence of tuberculosis, microbiological detection of mycobacteria, or a positive Mantoux test.
- -
Other infections: compatible findings and microbiological confirmation.
- -
IBD: compatible clinical findings and histologic confirmation.
- -
Sarcoidosis: compatible clinical-radiographic findings with or without histologic confirmation.
- -
Behçet disease: diagnostic criteria of the International Study Group for Behcet’s Disease.6
- -
Other autoimmune diseases: compatible clinical and serological findings.
- -
Hematologic diseases: clinical and histologic confirmation.
- -
Pregnancy: pregnancy and absence of other causes.
- -
Drugs: use of a given drug before onset of EN and absence of other causes.
- -
Idiopathic: negative results for the diagnostic work-up for EN, which had to include at least a targeted history and physical examination focused on known causes of EN (including drugs), basic blood tests, an autoimmune study, a Mantoux test, and chest radiography.
For all patients, we recorded sex, age at diagnosis of EN, performance of skin biopsy, and blood inflammatory marker levels (leukocytes, erythrocyte sedimentation rate [ESR], and C-reactive protein [CRP]).
Statistical AnalysisCategorical variables were expressed as absolute and relative frequencies and quantitative variables as mean (SD). Inflammatory markers were compared between patients with an inflammatory versus a noninflammatory cause of EN using the nonparametric Mann–Whitney U test. Statistical significance was set at a P value of less than .05. The statistical analysis was performed in STATA 9.04 (University Edition).
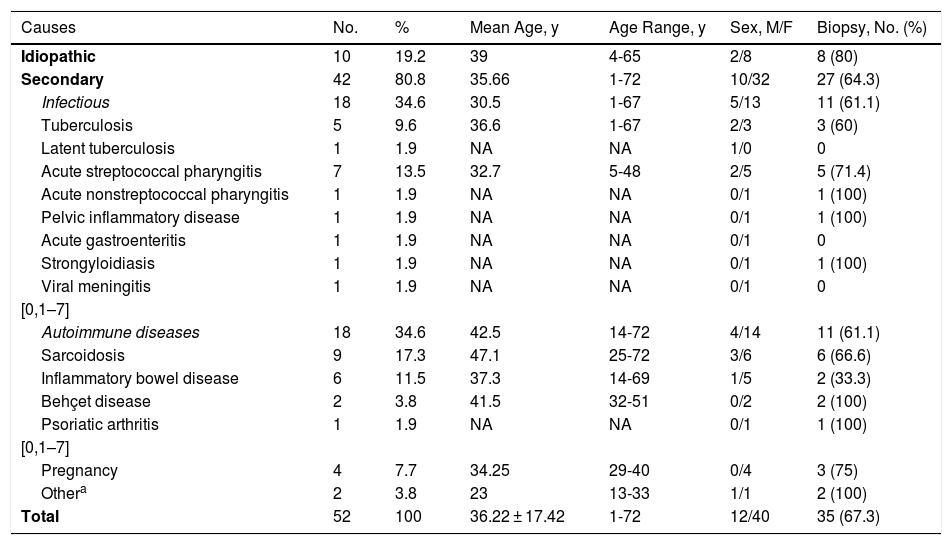
ResultsWe identified 116 patients with an initial diagnosis of EN, but 64 patients were excluded because of an incomplete medical history or diagnostic work-up for EN or because they were diagnosed outside the study period or with a condition other than EN. The final series therefore included 52 patients (76.9% female) with a mean age of 36.2 ± 17.4 years. The patients’ characteristics and the etiologic factors identified are summarized in Table 1. EN had been confirmed histologically in 35 patients (67.3%). There were 10 (19.2%) idiopathic cases, 18 cases (34.6%) associated with infection (streptococcal pharyngitis in 7 cases and tuberculosis in 5), 18 cases (34.6%) due to an autoimmune disease (sarcoidosis in 9 cases, IBD in 6, and Behçet disease in 2), and 4 cases (7.7%) due to pregnancy. Other common causes of EN, such as drugs, systemic lymphoma, yersiniosis, and systemic mycoses were not observed.
General Characteristics of Patients Hospitalized for a Diagnostic Work-up for Erythema Nodosum.
| Causes | No. | % | Mean Age, y | Age Range, y | Sex, M/F | Biopsy, No. (%) |
|---|---|---|---|---|---|---|
| Idiopathic | 10 | 19.2 | 39 | 4-65 | 2/8 | 8 (80) |
| Secondary | 42 | 80.8 | 35.66 | 1-72 | 10/32 | 27 (64.3) |
| Infectious | 18 | 34.6 | 30.5 | 1-67 | 5/13 | 11 (61.1) |
| Tuberculosis | 5 | 9.6 | 36.6 | 1-67 | 2/3 | 3 (60) |
| Latent tuberculosis | 1 | 1.9 | NA | NA | 1/0 | 0 |
| Acute streptococcal pharyngitis | 7 | 13.5 | 32.7 | 5-48 | 2/5 | 5 (71.4) |
| Acute nonstreptococcal pharyngitis | 1 | 1.9 | NA | NA | 0/1 | 1 (100) |
| Pelvic inflammatory disease | 1 | 1.9 | NA | NA | 0/1 | 1 (100) |
| Acute gastroenteritis | 1 | 1.9 | NA | NA | 0/1 | 0 |
| Strongyloidiasis | 1 | 1.9 | NA | NA | 0/1 | 1 (100) |
| Viral meningitis | 1 | 1.9 | NA | NA | 0/1 | 0 |
| [0,1–7] | ||||||
| Autoimmune diseases | 18 | 34.6 | 42.5 | 14-72 | 4/14 | 11 (61.1) |
| Sarcoidosis | 9 | 17.3 | 47.1 | 25-72 | 3/6 | 6 (66.6) |
| Inflammatory bowel disease | 6 | 11.5 | 37.3 | 14-69 | 1/5 | 2 (33.3) |
| Behçet disease | 2 | 3.8 | 41.5 | 32-51 | 0/2 | 2 (100) |
| Psoriatic arthritis | 1 | 1.9 | NA | NA | 0/1 | 1 (100) |
| [0,1–7] | ||||||
| Pregnancy | 4 | 7.7 | 34.25 | 29-40 | 0/4 | 3 (75) |
| Othera | 2 | 3.8 | 23 | 13-33 | 1/1 | 2 (100) |
| Total | 52 | 100 | 36.22 ± 17.42 | 1-72 | 12/40 | 35 (67.3) |
Abbreviations: F, female; M, male.
Secondary cases of EN were treated according to the cause identified. Symptomatic treatments included NSAIDS and/or paracetamol (25 patients, 48%) corticosteroids (17 patients, 32.7%), potassium iodide (9 patients, 17.3%), and colchicine (5 patients, 9.6%). We were unable to determine recurrences or time to resolution as this information was not available in the medical records.
On comparing inflammatory causes (infectious and autoimmune diseases) and noninflammatory causes, we observed no significant differences in mean values for leukocytes (10428 vs. 9964 leukocytes/mm3, P = .82), ESR (65.85 vs. 61.27 mm/h, P = .68), or CRP (6.97 vs. 8.63 mg/dL, P = .53).
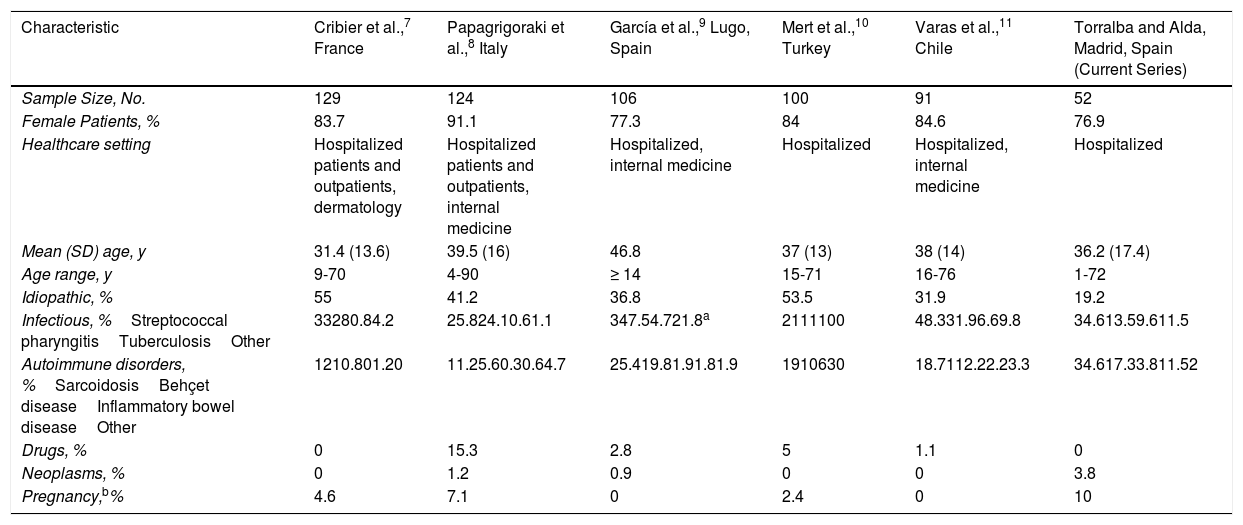
DiscussionA comparison of our results and those from other series is given in Table 2. The mean age of the patients in our series is similar to that reported elsewhere, but we observed a somewhat lower percentage of female patients. We also observed fewer idiopathic cases, perhaps because our patients were all hospitalized and therefore probably underwent a more exhaustive diagnostic work-up. The proportion of infectious cases is similar to that reported in other European studies,7–10 although lower than that observed by Varas et al.11 in Chile. The most common infections both in our series and others were streptococcal pharyngitis and tuberculosis. We observed a higher proportion of cases attributable to autoimmune diseases (in particular IBD and sarcoidosis), although the frequency of sarcoidosis was similar to that reported by García et al.9 in Spain. The proportion of cases due to Behçet disease was similar to other reports. Of note in our series was the absence of drug-induced EN and a higher proportion of cases associated with pregnancy and cancer.
Comparison of Demographic and Etiologic Characteristics of Patients From Different Series Who Underwent a Diagnostic Work-up for Erythema Nodosum.
| Characteristic | Cribier et al.,7 France | Papagrigoraki et al.,8 Italy | García et al.,9 Lugo, Spain | Mert et al.,10 Turkey | Varas et al.,11 Chile | Torralba and Alda, Madrid, Spain (Current Series) |
|---|---|---|---|---|---|---|
| Sample Size, No. | 129 | 124 | 106 | 100 | 91 | 52 |
| Female Patients, % | 83.7 | 91.1 | 77.3 | 84 | 84.6 | 76.9 |
| Healthcare setting | Hospitalized patients and outpatients, dermatology | Hospitalized patients and outpatients, internal medicine | Hospitalized, internal medicine | Hospitalized | Hospitalized, internal medicine | Hospitalized |
| Mean (SD) age, y | 31.4 (13.6) | 39.5 (16) | 46.8 | 37 (13) | 38 (14) | 36.2 (17.4) |
| Age range, y | 9-70 | 4-90 | ≥ 14 | 15-71 | 16-76 | 1-72 |
| Idiopathic, % | 55 | 41.2 | 36.8 | 53.5 | 31.9 | 19.2 |
| Infectious, %Streptococcal pharyngitisTuberculosisOther | 33280.84.2 | 25.824.10.61.1 | 347.54.721.8a | 2111100 | 48.331.96.69.8 | 34.613.59.611.5 |
| Autoimmune disorders, %SarcoidosisBehçet diseaseInflammatory bowel diseaseOther | 1210.801.20 | 11.25.60.30.64.7 | 25.419.81.91.81.9 | 1910630 | 18.7112.22.23.3 | 34.617.33.811.52 |
| Drugs, % | 0 | 15.3 | 2.8 | 5 | 1.1 | 0 |
| Neoplasms, % | 0 | 1.2 | 0.9 | 0 | 0 | 3.8 |
| Pregnancy,b% | 4.6 | 7.1 | 0 | 2.4 | 0 | 10 |
We found no significant differences in blood inflammatory markers between patients with inflammatory and noninflammatory causes of EN, coinciding with findings by García et al.9 but contrasting with those by Varas et al.11 and Mert et al.10 Misdiagnosis in patients in whom lesions were not biopsied is unlikely as EN lesions are highly characteristic.
In conclusion, multiple etiologic factors must be investigated in patients with EN. The fact that our patients were all hospitalized would seem to explain the lower percentage of idiopathic cases detected and the absence of common causes, such as drugs. Infections and autoimmune diseases were the most common causes of secondary EN in our series. We did not observe any differences in blood inflammatory markers between patients with inflammatory and noninflammatory causes of EN.
We believe that a reasonable approach to establishing the cause of EN in hospitalized patients would be to perform a targeted history and physical examination focusing on the main causes of EN, including drugs; a complete blood count including a routine biochemical workup, ESR, and CRP; an ASO test; simple chest radiography; and a Mantoux test. The need for serology testing to rule out infectious or autoimmune disease or the performance of other tests should be evaluated on a case-by-case basis according to symptoms.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Torralba-Morón Á and Alda-Bravo I. Causas de eritema nudoso en pacientes ingresados en un hospital español de tercer nivel. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2018.12.012