The location of cutaneous melanoma is associated with photoexposure.
ObjectivesTo retrospectively analyze changes in the location of cutaneous melanoma over the past 30 years.
Patients and methodsAll patients treated at our hospital for cutaneous melanoma from 1988 through 2017 were prospectively collected. Data obtained in cases diagnosed from 1988 through June 2006 were compared to those diagnosed from July 2006 through 2017.
ResultsA total of 1,937 patients (876 men and 1061 women; median age, 57 years; interquartile range 27) were diagnosed with primary cutaneous melanoma. The location of melanoma was head and neck (470 cases), trunk (745 cases), upper limbs (239 cases), and lower limbs (483 cases). From July 2006 through 2017 we detected an increase in the incidence of head and neck melanomas (19.9% vs 28.6%, p <0.001). A drop in the incidence of melanomas located in the lower extremities was also seen in women (39.8% vs 30.4%, p <0.001), and in the trunk men (57.5% vs 47.3%, p=0.003). In the multivariate analyses, only the decrease in melanomas located in lower extremities in women remained significant.
ConclusionThe increased incidence of head and neck melanomas in both sexes and the decrease in trunk melanomas in men can be attributed to the aging of our population. The reduction in the incidence of melanomas in the lower extremities in women could be associated with changes in photoexposure patterns. Analyzing the factors possibly associated with these changes would contribute to better understanding the pathogenesis of cutaneous melanoma for prevention purposes.
La localización del melanoma cutáneo está relacionada con el patrón de fotoexposición.
ObjetivosAnalizar retrospectivamente las variaciones en la localización del melanoma en los últimos 30 años.
Pacientes y métodosFueron recogidos prospectivamente todos los pacientes atendidos en nuestro hospital por melanoma cutáneo entre 1988 y 2017. Se analizaron los cambios de localización entre la primera y la segunda mitad del periodo.
ResultadosUn total de 1.937 pacientes (876 varones, 1.061 mujeres, edad mediana 57 años, rango intercuartílico 27) fueron diagnosticados de melanoma cutáneo. La localización fue cabeza y cuello en 470 casos, tronco en 745, miembros superiores en 239 y miembros inferiores en 483. En el segundo periodo aumentó en la proporción de melanomas en cabeza y cuello (19,9% vs. 28,6 p<0,001) y disminuyó la proporción de melanomas en las extremidades inferiores en mujeres (39,8% vs. 30,4%, p<0,001) y en el tronco en varones (57,5% vs. 47,3%, p=0,003). En análisis multivariante, únicamente la reducción en la proporción de melanomas en las extremidades inferiores en el sexo femenino mantuvo la significación estadística.
ConclusiónEl aumento en la proporción de melanomas en cabeza y cuello en ambos sexos y la disminución en el tronco en varones puede atribuirse al envejecimiento de nuestra población. La reducción en la proporción de melanomas localizados en las extremidades inferiores en las mujeres podría deberse a cambios en los patrones de fotoexposición. El análisis de los factores posiblemente asociados a estos cambios podría ayudar a comprender mejor la patogenia del melanoma cutáneo y mejorar su prevención.
It is well established that exposure to sunlight is one of the most important etiological factors for skin melanoma1. Areas of the skin that are chronically exposed to the sun have a higher risk of developing melanoma, especially lentigo maligna. However, for the most common form of melanoma in the Caucasian race (superficial spreading melanoma), the risk appears to be higher in areas of intermittent and intense sun exposure1. Multiple studies have detected differences in the location of melanoma between both sexes, which can be explained by the disparity in photoexposed regions of the skin in women compared to men2-8; nonetheless, a scarcity of studies have analyzed changes in the location of melanoma over the past decades.
Our objective was to evaluate the changes in the location of skin melanoma in our patients over the last 30 years and analyze the possible associated factors.
Patients and methodsAll patients treated for cutaneous melanoma at Hospital Universitari de Bellvitge, (Barcelona, Spain) from 1988 through 2017 were prospectively collected and included in the study. This is a teaching hospital providing tertiary care to a population of approximately one million people. With prior authorization from the ethics committee, the patients’ health records were reviewed to obtain the following clinical data: age, sex, and location of skin melanoma (head and neck, trunk, upper limbs, lower limbs). The histopathological data collected were the clinical-pathological type of skin melanoma (lentigo maligna-melanoma, superficial spreading melanoma, nodular melanoma, and acral lentiginous melanoma, as well as other types of skin melanoma; mucosal melanomas and melanomas of unknown origin were not included), and maximum depth of invasion (Breslow index). The maximum depth of invasion was stratified into melanoma in situ, T1 (Breslow ≤ 1mm), T2 (Breslow >1mm up to 2mm), T3 (Breslow >2mm up to 4mm), T4 (Breslow >4mm). The characteristics of the cases diagnosed from 1988 through June 2006 were compared with those diagnosed from July 2006 through 2017 to obtain 2 comparable populations of similar size.
Data obtained were analyzed with the SPSS program for Windows (SPSS Inc. Released 2008; Statistics for Windows, version 17.0; Chicago, SPSS Inc., United States). Categorical variables were compared using the chi-square test. Continuous variables were compared using the Student t-test when the normality of the variable distribution was confirmed; otherwise, non-parametric tests were used. Univariate and multivariate logistic regression was used to evaluate changes in the location of melanoma between the 2 analyzed periods of time and determine the possible influence of other variables. P values<0.05 were considered statistically significant.
ResultsA total of 1937 patients with skin melanoma were diagnosed during the analyzed period (876 men and 1061 women). The median age was 57 years (interquartile range [IQR], 27). Melanomas were found in the head and neck region in 470 cases (24.3%), trunk in 745 (38.7%), upper limbs in 239 (12.3%), and lower limbs in 483 cases (24.9%). The clinical-pathological type of melanoma was lentigo maligna-lentigo maligna melanoma in 344 cases (17.8%), superficial spreading melanoma in 1209 (62.4%), nodular melanoma in 184 (9.5%), acral lentiginous melanoma in 104 (5.4%), and less frequent or unclassifiable forms of melanoma in 96 cases (4.9%).
A total of 575 cases were melanomas in situ (29.7%) and 1362 cases, invasive melanomas (70.3%). Invasive melanomas corresponded to T1 in 662 cases, T2 in 302, T3 in 220, and T4 in 178. The median maximum depth of invasion (Breslow index) of invasive melanomas was 1.05mm (IQR, 1.78).
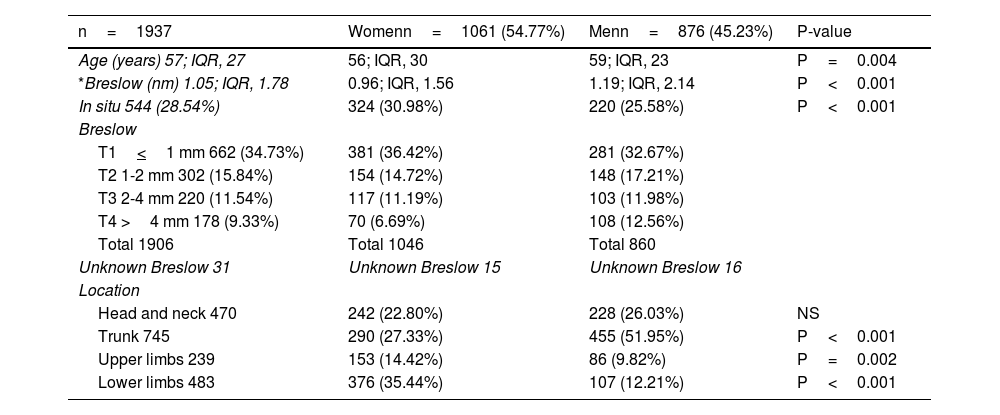
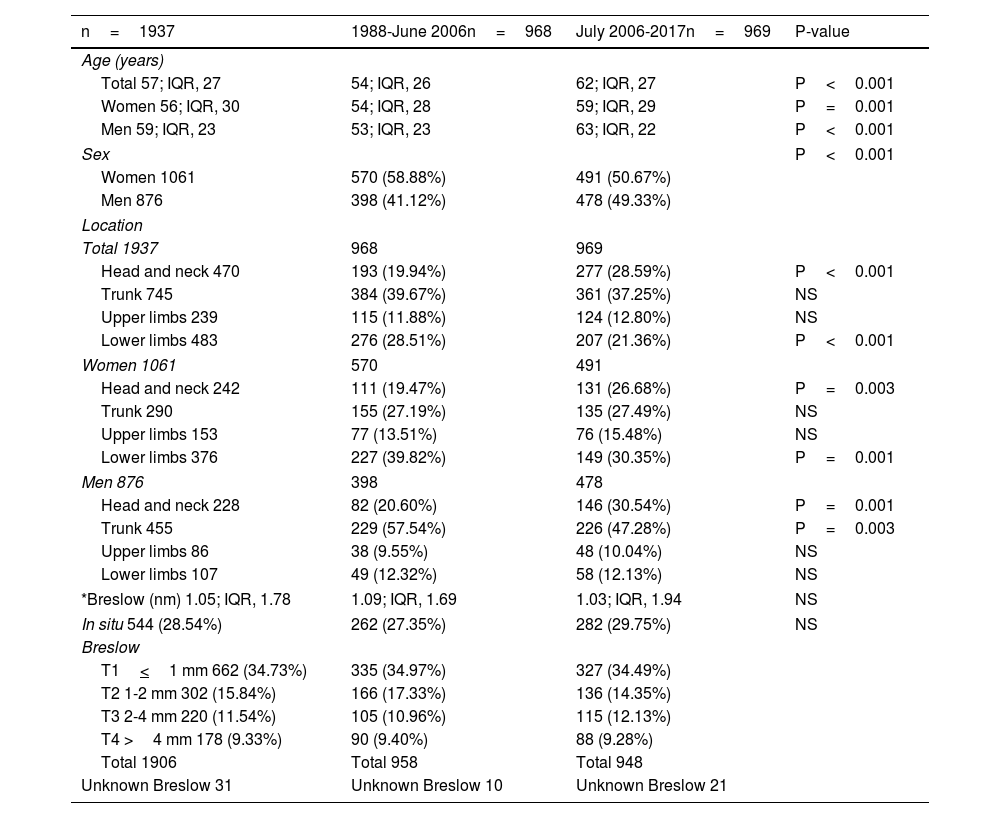
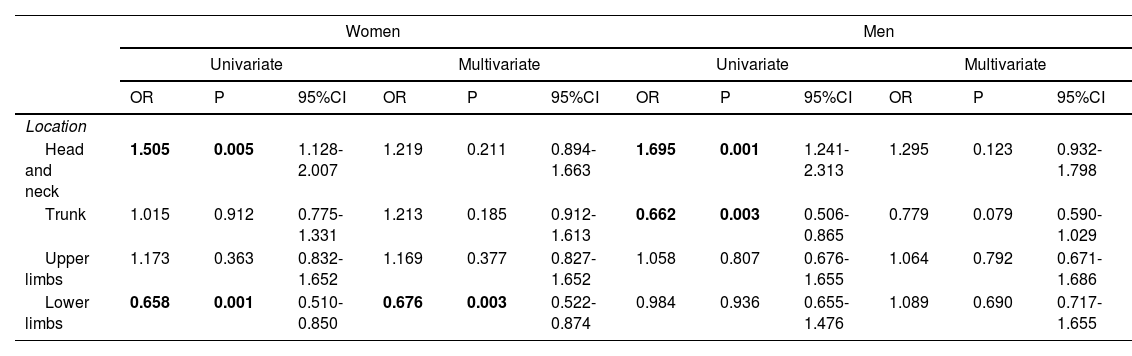
The comparison of the patients’ clinical-pathological characteristics between both sexes is detailed in Table 1. The comparisons between the data obtained within the first analyzed period (1988-2006) and data obtained within the second period (2006-2017) are shown in Table 2. Significant changes are seen between both periods in the proportion of women/men, the patients’ age, as well as in the number of lesions found in the head and neck region, and lower limbs. Stratifying by sex, significant increases in lesions on the head and neck in both sexes and decreases in the number of melanomas on the lower limbs in women and on the trunk in men were observed. A multivariate study was conducted for each sex, introducing as variables the anatomical location of melanoma and the patients’ age, while only the changes reported in the number of lesions found on the lower limbs in women remained statistically significant (Table 3).
Comparison of melanoma characteristics by sex.
| n=1937 | Womenn=1061 (54.77%) | Menn=876 (45.23%) | P-value |
|---|---|---|---|
| Age (years) 57; IQR, 27 | 56; IQR, 30 | 59; IQR, 23 | P=0.004 |
| *Breslow (nm) 1.05; IQR, 1.78 | 0.96; IQR, 1.56 | 1.19; IQR, 2.14 | P<0.001 |
| In situ 544 (28.54%) | 324 (30.98%) | 220 (25.58%) | P<0.001 |
| Breslow | |||
| T1<1 mm 662 (34.73%) | 381 (36.42%) | 281 (32.67%) | |
| T2 1-2 mm 302 (15.84%) | 154 (14.72%) | 148 (17.21%) | |
| T3 2-4 mm 220 (11.54%) | 117 (11.19%) | 103 (11.98%) | |
| T4 >4 mm 178 (9.33%) | 70 (6.69%) | 108 (12.56%) | |
| Total 1906 | Total 1046 | Total 860 | |
| Unknown Breslow 31 | Unknown Breslow 15 | Unknown Breslow 16 | |
| Location | |||
| Head and neck 470 | 242 (22.80%) | 228 (26.03%) | NS |
| Trunk 745 | 290 (27.33%) | 455 (51.95%) | P<0.001 |
| Upper limbs 239 | 153 (14.42%) | 86 (9.82%) | P=0.002 |
| Lower limbs 483 | 376 (35.44%) | 107 (12.21%) | P<0.001 |
NS, not significant.
Comparison of melanoma characteristics from 1988 through 2006 and from 2006 through 2017.
| n=1937 | 1988-June 2006n=968 | July 2006-2017n=969 | P-value |
|---|---|---|---|
| Age (years) | |||
| Total 57; IQR, 27 | 54; IQR, 26 | 62; IQR, 27 | P<0.001 |
| Women 56; IQR, 30 | 54; IQR, 28 | 59; IQR, 29 | P=0.001 |
| Men 59; IQR, 23 | 53; IQR, 23 | 63; IQR, 22 | P<0.001 |
| Sex | P<0.001 | ||
| Women 1061 | 570 (58.88%) | 491 (50.67%) | |
| Men 876 | 398 (41.12%) | 478 (49.33%) | |
| Location | |||
| Total 1937 | 968 | 969 | |
| Head and neck 470 | 193 (19.94%) | 277 (28.59%) | P<0.001 |
| Trunk 745 | 384 (39.67%) | 361 (37.25%) | NS |
| Upper limbs 239 | 115 (11.88%) | 124 (12.80%) | NS |
| Lower limbs 483 | 276 (28.51%) | 207 (21.36%) | P<0.001 |
| Women 1061 | 570 | 491 | |
| Head and neck 242 | 111 (19.47%) | 131 (26.68%) | P=0.003 |
| Trunk 290 | 155 (27.19%) | 135 (27.49%) | NS |
| Upper limbs 153 | 77 (13.51%) | 76 (15.48%) | NS |
| Lower limbs 376 | 227 (39.82%) | 149 (30.35%) | P=0.001 |
| Men 876 | 398 | 478 | |
| Head and neck 228 | 82 (20.60%) | 146 (30.54%) | P=0.001 |
| Trunk 455 | 229 (57.54%) | 226 (47.28%) | P=0.003 |
| Upper limbs 86 | 38 (9.55%) | 48 (10.04%) | NS |
| Lower limbs 107 | 49 (12.32%) | 58 (12.13%) | NS |
| *Breslow (nm) 1.05; IQR, 1.78 | 1.09; IQR, 1.69 | 1.03; IQR, 1.94 | NS |
| In situ 544 (28.54%) | 262 (27.35%) | 282 (29.75%) | NS |
| Breslow | |||
| T1<1 mm 662 (34.73%) | 335 (34.97%) | 327 (34.49%) | |
| T2 1-2 mm 302 (15.84%) | 166 (17.33%) | 136 (14.35%) | |
| T3 2-4 mm 220 (11.54%) | 105 (10.96%) | 115 (12.13%) | |
| T4 >4 mm 178 (9.33%) | 90 (9.40%) | 88 (9.28%) | |
| Total 1906 | Total 958 | Total 948 | |
| Unknown Breslow 31 | Unknown Breslow 10 | Unknown Breslow 21 | |
NS, not significant.
Comparison of the risk for developing melanoma in different locations in women and men from 1988 through 2006 and from 2006 through 2017 using logistic regression.
| Women | Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | |||||||||
| OR | P | 95%CI | OR | P | 95%CI | OR | P | 95%CI | OR | P | 95%CI | |
| Location | ||||||||||||
| Head and neck | 1.505 | 0.005 | 1.128-2.007 | 1.219 | 0.211 | 0.894-1.663 | 1.695 | 0.001 | 1.241-2.313 | 1.295 | 0.123 | 0.932-1.798 |
| Trunk | 1.015 | 0.912 | 0.775-1.331 | 1.213 | 0.185 | 0.912-1.613 | 0.662 | 0.003 | 0.506-0.865 | 0.779 | 0.079 | 0.590-1.029 |
| Upper limbs | 1.173 | 0.363 | 0.832-1.652 | 1.169 | 0.377 | 0.827-1.652 | 1.058 | 0.807 | 0.676-1.655 | 1.064 | 0.792 | 0.671-1.686 |
| Lower limbs | 0.658 | 0.001 | 0.510-0.850 | 0.676 | 0.003 | 0.522-0.874 | 0.984 | 0.936 | 0.655-1.476 | 1.089 | 0.690 | 0.717-1.655 |
On univariate analysis, a significant increase in the risk of developing melanoma on the head and neck was observed in both sexes, as well as a decrease on women's lower limbs and men's trunks. On multivariate analysis, patient age was introduced as a cofactor, and only the decrease in the proportion of melanomas reported on women's lower limbs remained statistically significant. The loss of significance in the risk of developing melanoma on the head and neck in both sexes and on men's trunks can, therefore, be attributed to changes in the patients’ age.
Significant results are highlighted in bold.
Relative risk for developing melanoma in each location in the 2nd vs the 1st analyzed periods.
The location of skin melanoma has changed in our population over the past few decades. The number of melanomas found in the head and neck region has increased in both sexes, and the number of melanomas located on the lower limbs has decreased in the female population.
Aside from the clinical-pathological type of melanoma, the anatomical location of skin melanoma is influenced by various factors. There are significant differences in the location of melanoma across different ethnicities; for example, the trunk is the anatomical region most widely affected among Caucasians,7,9 while in the Japanese population, the most common location is the lower limbs,10 and in the black race, the most widely affected location is the soles of the feet11. Regarding the patients’ age, older individuals exhibit more melanomas in the head and neck region vs younger patients.7,9 Regarding the impact sex has on the location of melanoma, the most common location is the trunk in men and the lower limbs in women.2-8 In the present study, with a predominantly Caucasian population, the most common location in men is also the trunk (52% of men from our series exhibited trunk melanomas), while in women the most common location is the lower limbs (35.4% of our female patients developed lower limb melanomas). These differences can be explained by greater intermittent and intense sun exposure on women's lower limbs and men's trunks6. Regarding age, we also found that the median age of our patients with head and neck melanomas was significantly higher vs patients with trunk and limb melanomas (70 years [IQR 20] vs 54 years [IQR 25], P<0.001), which can be attributed to a higher cumulative dose of UV radiation in the head and neck region of older patients.
Few studies have analyzed changes in the location of skin melanoma over time. Among of them, one conducted from 1966 through 1987 found fewer melanomas on women's lower limbs.12 Another similar study comparing the location of melanomas in the 1970s with those of 2004 also found fewer lesions on women's lower limbs, and, additionally, a 2004 increase in the number of lesions found on men's head and neck.13 Finally, a study conducted in Spain also saw an increase in the number of melanomas found on the trunk followed by a decrease in the number of melanomas found on the lower limbs from 1983 to 1990, and from 1991 through 2001, although changes based on the patients’ sex were not analyzed.14 In the present study, we compared the location of skin melanoma from 1988 to 2006, and from 2006 through 2017 and saw a significant increase in the number of lesions located on the head and neck within the second period, which in our study can be seen in both sexes (men, 30.5% vs 20.6%, P=0.001; women, 26.7% vs 19.5%, P=0.003). Similarly, within the second period, we found a significant decrease in the number of lesions affecting men's trunks (47.3% vs 57.5%, P=0.003) and women's lower limbs (30.6% vs.39.8%, P=0.001). The increase in the number of lesions found in the head and neck region may be due to the aging of our population, with the corresponding increase in cumulative chronic sun exposure, which obviously affects both sexes.9,15 The decrease in the number of lesions located on men's trunks could also be due to population aging, with a corresponding increase in the number of lesions found on the head and neck. Using multivariate logistic regression, our analysis confirmed that these changes reported in the location of skin melanoma between the 2 analyzed periods in the head and neck region in both sexes and on men's trunk may be associated with changes in the patients’ age. However, the lower proportion of lesions found on women's lower limbs during the second period remained significant on the multivariate analysis after introducing age as a cofactor. This decrease in the number of melanomas on women's lower limbs could be due to less sun exposure on the legs resulting from changes in photoexposure patterns.
Bowen's disease, squamous cell carcinoma, basal cell carcinoma, and melanoma are more frequently located on women's lower limbs vs men, due to the greater exposure of women's lower limbs to UV solar radiation because of their dressing habits16. Since the 1940s, changes in dressing habits in Western Europe led to significant sun exposure of women's legs as they started wearing knee-length skirts12. In the 1950s and 1960s, most women's lower limbs were especially exposed year-round to UV solar radiation, as the stockings they used were not protective enough vs UV solar radiation12,16. Since the 1970s, women's clothing has diversified, and the use of long skirts and pants has increased, which is why some authors believe that since then, the exposure of legs to UV solar radiation has decreased, and therefore, these garments may be providing effective protection vs solar radiation on the lower limbs12.
The main limitation of our study is that it was a retrospective observational analysis conducted in a single health care center. Additionally, although our subjective impression is that changes in women's clothing are clearly related to the decrease in melanomas on women's lower limbs, we cannot confirm this experimentally.
In conclusion, our findings reveal changes in the location of primary skin melanoma in recent decades. The number of melanomas located in the head and neck region is increasing in both sexes, probably due to the aging population. The most significant change we saw is fewer melanomas on women's lower limbs, possibly due to changes in the photoexposure patterns of our population. If these changes are confirmed, analyzing the possibly associated factors would help better understand the pathogenesis of skin melanoma and improve prevention.
Conflicts of interestNone declared.