This review of the literature on palmoplantar hypokeratosis, a process that was first indentified only 10 years ago, discusses the current state of our understanding, the therapeutic options available, and the debate about etiology. Forty-four publications reporting 69 cases were found. Palmar or plantar hypokeratosis occurs mainly in women (76.8%) and age at the time of a first visit to a physician ranges from 42 to 84 years. Most cases present between the ages of 51 and 70 years. The majority of patients have had solitary lesions usually located on the right palm, particularly in the regions of the thenar (in 44/79 lesions [55.7%]) or hypothenar eminences (in 11/79 lesions [13.9%]). In only 8 cases was there a history of prior trauma at the site. Studies using polymerase chain reaction techniques to identify human papillomavirus involvement were negative in most cases. These hypokeratotic lesions are localized epidermal depressions formed by an abrupt thinning of the stratum corneum, providing a singular histopathologic feature. This condition can currently be considered a localized keratinization disorder affecting zones where there is a thick stratum corneum. The precipitating cause is unknown and a definitive treatment remains to be found. The mechanism would be the localized failure of a clone of keratinocytes during differentiation toward normal palmoplantar hyperkeratinization.
Se revisa el estado actual de un nuevo proceso y los avances que han ido apareciendo en la literatura respecto a su estudio, posibilidades terapéuticas y controvertida etiología, tras justo una década de su descripción inicial. Hemos encontrado 44 publicaciones al respecto, con 69 casos. Predomina en mujeres (76,8%), con edades entre los 42 y 84 años para toda la casuística en el momento de la consulta, siendo el rango más frecuente de aparición de las lesiones entre los 51 y 70 años. La gran mayoría de las veces fueron lesiones únicas y se localizaron predominantemente en la palma derecha, preferentemente en la región tenar, con 44/79 lesiones (55,7%) y luego en la hipotenar, con 11/79 lesiones (13,9%). Solo en 8 casos se obtuvo el antecedente de un traumatismo previo. Los estudios mediante PCR en búsqueda de papiloma virus humano han sido negativos la gran mayoría de las veces. Las lesiones consistieron en una depresión focalizada de la epidermis producida por una brusca disminución de espesor de la capa córnea, delimitando un singular concepto histolopatológico. En la actualidad puede ser considerada como un trastorno focalizado de la queratinización, que afecta zonas con un estrato córneo grueso, cuya causa precipitante es desconocida y su tratamiento definitivo aún por dilucidar. Se produciría por un fallo clonal localizado de los queratinocitos hacia una diferenciación hiperqueratósica normal, de tipo palmo-plantar.
Increased thickness of the corneal layer of the skin, or hyperkeratosis, is described in possibly all the analytical indices of dermatopathology and dermatology texts. In contrast, the term circumscribed palmar or plantar hypokeratosis, brought into usage a decade ago to describe an abrupt reduction in the thickness of the corneal layer in a circumscribed area of the palm or sole, is much less common.1 For the origin of this term we must go back to the year 2002, when it was used to describe a series of 10 patients from Germany, Chile, and Spain, reported by Pérez et al.2
Since that time, further cases with identical clinical and histopathologic characteristics have been reported in other countries, including Austria, Korea, United States, France, Italy, Japan, Malta, New Zealand, and Peru, leading gradually to the characterization of a new entity.
The purpose of this article has been to review the advances that have been made in this disease a decade after its first description, with impartial contributions from different countries across the globe, by professionally independent authors. Our aim has been to describe the current state of knowledge of the disease and to review the literature on advances in research into the disease, on the therapeutic options available, and on the debate about its etiology.
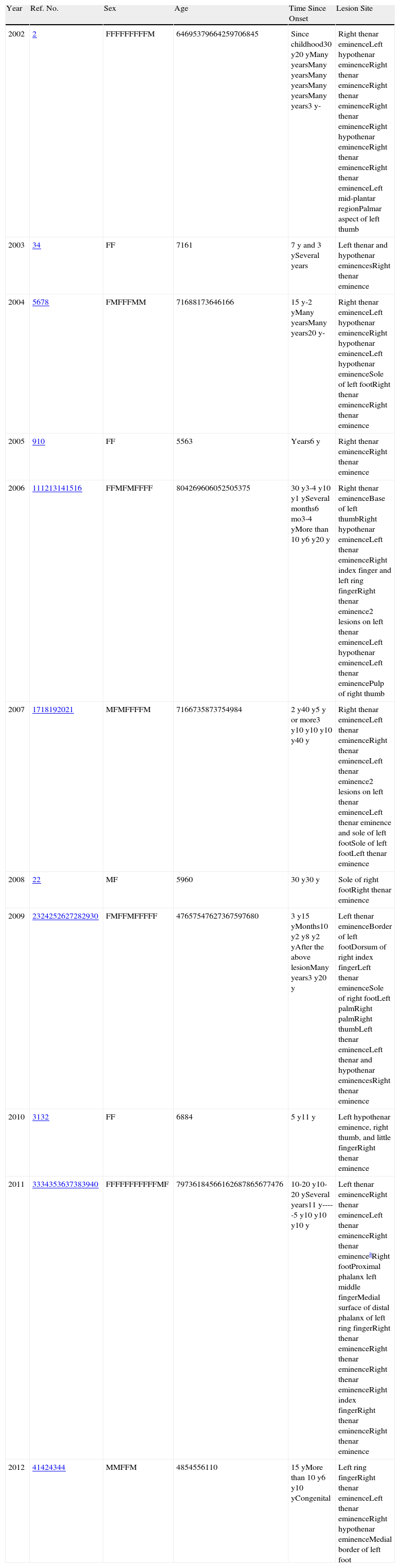
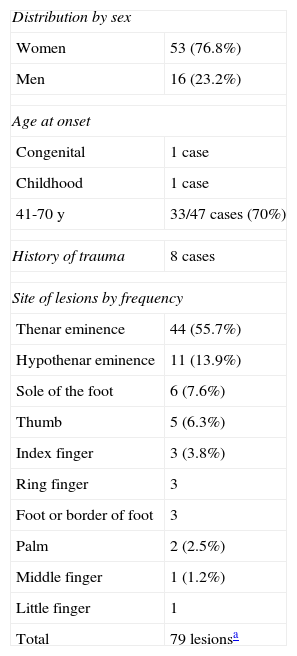
Clinical PresentationA search performed in a number of databases at the time this article was being written revealed 44 papers on circumscribed palmar or plantar hypokeratosis. Sixty-nine cases have now been reported.2–44 Their clinical characteristics are listed in Table 1 and are summarized in Table 2. This is an acquired disorder that is more common in women, with a female to male ratio of 3.3 to1, and it has been reported in patients aged between 42 and 84 years (mean age, 64.6 years) at the time of first consultation (one outlying case with lesions present from birth44 was excluded from this calculation). In a large majority of cases (60 patients) the lesions were single; there were only 8 cases with 2 lesions,3,11,13,20,21,27,29 one with 3 lesions,31 and an exceptional case with 13 lesions in a linear distribution21 (also excluded from the calculations as it was an outlier). Most lesions were located on the right palm, mainly affecting the thenar region (44 of 79 lesions). Lesions affecting the digits have been detected in isolated cases,2,11,16,24,27,31,34,38,41 most commonly on the thumb,2,11,16,27,31,34 but in 1 case on the dorsum of the index finger.24 Lesions have also been reported on the palm,26 on the dorsum or border of the feet,24,34,44 and on the sole.2,7,21,22,26 The mean duration of lesions was 12.8 years, with an approximate range of 1 to 50 years; this could not be exact as 1 patient of 64 years of age2 had developed lesions as a child and these were arbitrarily determined to have appeared at 14 years of age; the range was calculated on the basis only of those patients who stated the duration of the lesions in years or in whom this could be estimated.
Clinical Characteristics of 69 Cases of Circumscribed Palmar or Plantar Hypokeratosis, Listed According to the Year of Publication.
| Year | Ref. No. | Sex | Age | Time Since Onset | Lesion Site |
| 2002 | 2 | FFFFFFFFFM | 64695379664259706845 | Since childhood30 y20 yMany yearsMany yearsMany yearsMany yearsMany years3 y- | Right thenar eminenceLeft hypothenar eminenceRight thenar eminenceRight thenar eminenceRight thenar eminenceRight hypothenar eminenceRight thenar eminenceRight thenar eminenceLeft mid-plantar regionPalmar aspect of left thumb |
| 2003 | 34 | FF | 7161 | 7 y and 3 ySeveral years | Left thenar and hypothenar eminencesRight thenar eminence |
| 2004 | 5678 | FMFFFMM | 71688173646166 | 15 y-2 yMany yearsMany years20 y- | Right thenar eminenceLeft hypothenar eminenceRight hypothenar eminenceLeft hypothenar eminenceSole of left footRight thenar eminenceRight thenar eminence |
| 2005 | 910 | FF | 5563 | Years6 y | Right thenar eminenceRight thenar eminence |
| 2006 | 111213141516 | FFMFMFFFF | 804269606052505375 | 30 y3-4 y10 y1 ySeveral months6 mo3-4 yMore than 10 y6 y20 y | Right thenar eminenceBase of left thumbRight hypothenar eminenceLeft thenar eminenceRight index finger and left ring fingerRight thenar eminence2 lesions on left thenar eminenceLeft hypothenar eminenceLeft thenar eminencePulp of right thumb |
| 2007 | 1718192021 | MFMFFFFM | 7166735873754984 | 2 y40 y5 y or more3 y10 y10 y10 y40 y | Right thenar eminenceLeft thenar eminenceRight thenar eminenceLeft thenar eminence2 lesions on left thenar eminenceLeft thenar eminence and sole of left footSole of left footLeft thenar eminence |
| 2008 | 22 | MF | 5960 | 30 y30 y | Sole of right footRight thenar eminence |
| 2009 | 2324252627282930 | FMFFMFFFFF | 47657547627367597680 | 3 y15 yMonths10 y2 y8 y2 yAfter the above lesionMany years3 y20 y | Left thenar eminenceBorder of left footDorsum of right index fingerLeft thenar eminenceSole of right footLeft palmRight palmRight thumbLeft thenar eminenceLeft thenar and hypothenar eminencesRight thenar eminence |
| 2010 | 3132 | FF | 6884 | 5 y11 y | Left hypothenar eminence, right thumb, and little fingerRight thenar eminence |
| 2011 | 3334353637383940 | FFFFFFFFFFFMF | 79736184566162687865677476 | 10-20 y10-20 ySeveral years11 y-----5 y10 y10 y10 y | Left thenar eminenceRight thenar eminenceLeft thenar eminenceRight thenar eminenceaRight footProximal phalanx left middle fingerMedial surface of distal phalanx of left ring fingerRight thenar eminenceRight thenar eminenceRight thenar eminenceRight index fingerRight thenar eminenceRight thenar eminence |
| 2012 | 41424344 | MMFFM | 4854556110 | 15 yMore than 10 y6 y10 yCongenital | Left ring fingerRight thenar eminenceLeft thenar eminenceRight hypothenar eminenceMedial border of left foot |
Summary of the Clinical Presentation of the 69 Cases of Circumscribed Palmar or Plantar Hypokeratosis.
| Distribution by sex | |
| Women | 53 (76.8%) |
| Men | 16 (23.2%) |
| Age at onset | |
| Congenital | 1 case |
| Childhood | 1 case |
| 41-70 y | 33/47 cases (70%) |
| History of trauma | 8 cases |
| Site of lesions by frequency | |
| Thenar eminence | 44 (55.7%) |
| Hypothenar eminence | 11 (13.9%) |
| Sole of the foot | 6 (7.6%) |
| Thumb | 5 (6.3%) |
| Index finger | 3 (3.8%) |
| Ring finger | 3 |
| Foot or border of foot | 3 |
| Palm | 2 (2.5%) |
| Middle finger | 1 (1.2%) |
| Little finger | 1 |
| Total | 79 lesionsa |
It is interesting to observe that the lesions had been present for a long period before consultation in the large majority of patients, possibly because they were considered banal by the patients themselves. The onset of lesions occurred most commonly between 61 and 70 years of age (13 cases), followed in decreasing frequency by the intervals of 51 to 60 years (12 cases), 41 to 50 years (8 cases), and 31 to 40 years (6 cases); these calculations were based only on the 47 cases in which the figures were known or could be accurately estimated. Some patients reported a history of trauma to the area, in particular burns,5,21,41 but also trauma from gardening or frequent writing,11 a bird peck,17 1 minor trauma,19 or long-standing practice of embroidery,32 as a possible trigger, but the large majority of patients reported no history of trauma and were unaware what could have triggered the lesions.
The clinical appearance of the lesions was almost identical in all cases, with a well-defined, round or oval depression on the palm (Fig. 1) or sole (Fig. 2), with reddish discoloration, and a slightly scaly border. The size of the lesions varied between a few millimeters11,21,37,43 and 5.5cm,10 but mostly measured around 1.5cm. The lesions were typically asymptomatic, although some patients described the skin as being more delicate and sensitive in the area of the lesion.
Based on the appearance of the lesions, the main differential diagnoses are Mibelli porokeratosis, Bowen disease, and the base of a blister in the erosion stage; pitted keratolysis may also occasionally be considered.
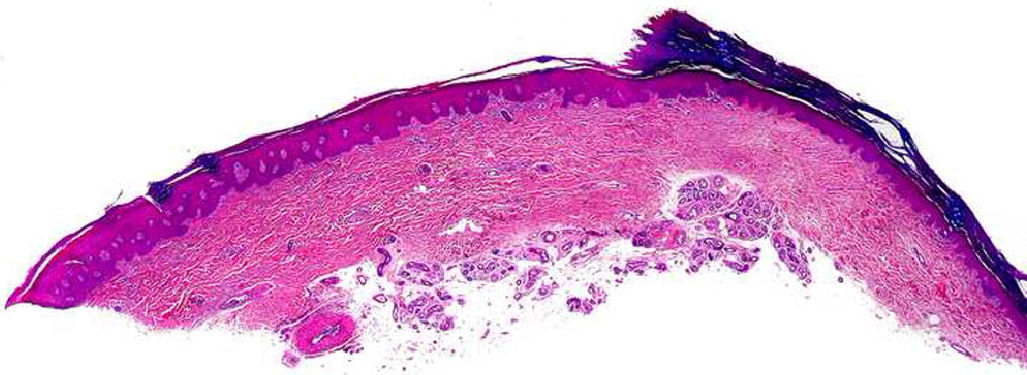
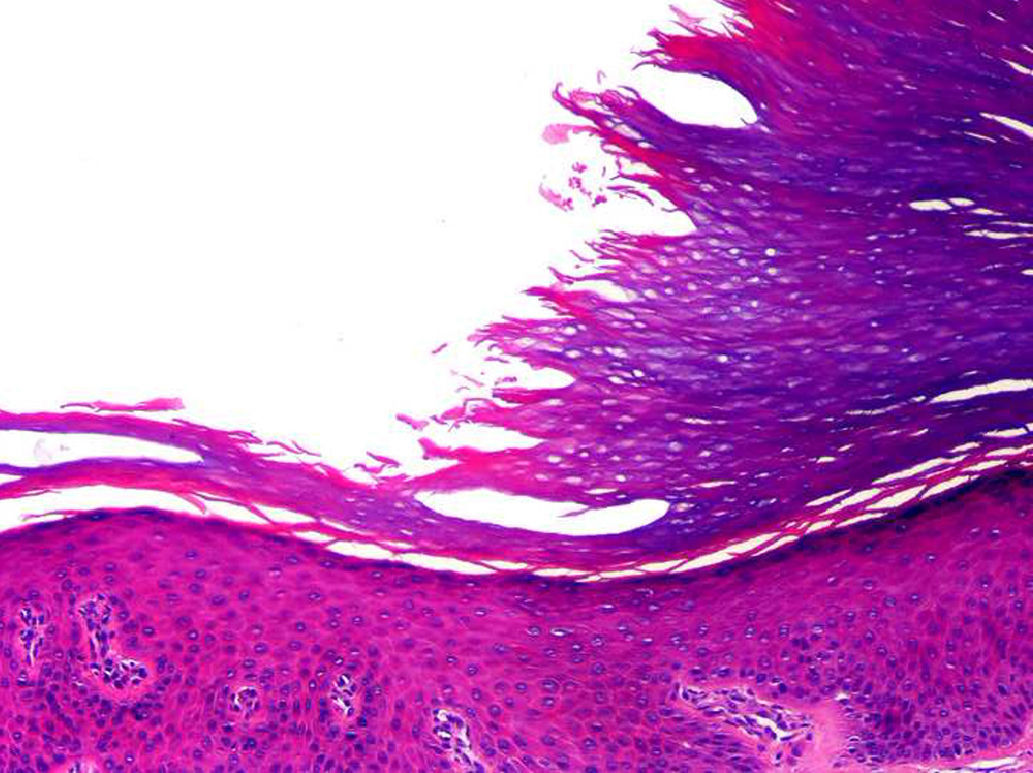
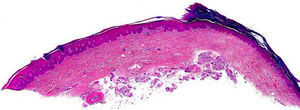
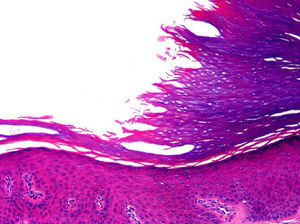
HistopathologyThe histopathology findings of the lesions have been practically identical in all patients. There is a depression of the epidermis caused by a reduction in the thickness of the corneal layer, with borders that are very well-defined. The transition between the normal and the affected epidermis is abrupt, with a marked step from the normal corneal layer, which is usually thick on the palms and soles, to the thin corneal layer of the lesion (Fig. 3). The thinning of the corneal layer is typically associated with slight thinning of the granular layer, causing the hypokeratosis to lie over an area of hypogranulosis. However, the corneocytes in the lesion show normal keratinization, giving rise to an orthokeratotic corneal layer with a multilayered structure and basophilic coloration, and the underlying keratinocytes show no noticeable morphological abnormalities.
In some cases the corneocytes at the transition between the normal corneal layer of the adjacent healthy skin and the thinned corneal layer of the lesion have a smooth and more eosinophilic appearance than the corneocytes immediately adjacent to the lesion (Fig. 4). Serial sections of the lesion stained with periodic acid-Schiff have revealed no signs of parakeratosis or cornoid lamella, which constitute the fundamental histopathological criteria for excluding porokeratosis, nor has it been possible to demonstrate continuity of alterations between the step in the epidermis and any of the underlying intraepidermal structures. Furthermore, the acrosyringia within the lesion are also involved in the alterations, as the corneal layer covering acrosyringia in the area of the lesion is not as thick as the corneal layer covering these structures in the adjacent healthy skin. In the lesions located in the thenar region of the palm, the underlying papillary dermis shows a degree of elastosis that varies between patients, but associated inflammatory infiltrates are not usually observed. It would therefore appear that the erythematous color of the lesions is because the atrophy of the corneal layer leads to greater transparency of the affected epidermis, and the greater proximity of the dermal vessels is what causes the erythema.
Histopathological Differential DiagnosisThe most important histopathological differential diagnosis of circumscribed palmar or plantar hypokeratosis is Mibelli porokeratosis affecting the palms or soles. However, porokeratosis lesions show no reduction in the thickness of the stratum corneum and the transition between healthy and lesional skin is marked by the inclined column of parakeratosis that forms the cornoid lamella. There is focal loss of the granular layer beneath the cornoid lamella and the underlying epidermal keratinocytes appear disorganized and show faulty maturation, with pyknotic nuclei and scattered areas of dyskeratosis. The lesions of porokeratosis usually present a lymphohistiocytic infiltrate with occasional melanophages in the dermis immediately underlying the cornoid lamella.
Electron MicroscopyDisruption or fragmentation of corneocytes within their cytoplasm has been detected, though intercellular adhesion was maintained at the borders of the lesion where the change in thickness of the corneal layer occurs; this may indicate that the condition develops due to fragility of the affected corneocytes and not due to a failure of cell adhesion.20 Vacuolar changes have also been observed in the corneocytes at the deep margin of the areas of hypokeratosis.20
One study has provided evidence of decreased keratinocyte maturation, with thinning of the granular layer in the area of the union between lesional and normal skin.22 However, another article described a failure in both keratinocyte and corneocyte adhesion—possibly induced by an abnormal production of Odland bodies—caused by external factors that provoke a segregation of plugs of broken down corneodesmosomes from the external layer of corneocytes37; in that same study it was suggested that there may be 2 forms of hypokeratosis, one caused by disorders of corneocyte adhesion and the other by corneocyte fragility, with no change in the adhesion structures.20 Another electron microscopy study, performed after clinical improvement had been achieved with long-term treatment with topical calcipotriol, showed preservation of desmosomes and bundles of keratin in the basal layer, but these structures were somewhat disperse and disordered in the granular layer, with a reduction in keratohyaline granules and an increase in cytoplasmic lipid droplets in comparison with normal skin.45
ImmunohistochemistryThe first publication on the immunohistochemistry of circumscribed palmar or plantar hypokeratosis19 and a subsequent study34 revealed increased expression of the p53 tumor suppressor gene and of the MIB-1 (Ki-67) cell proliferation marker in the affected area. In another case neither finding could be confirmed,26 though MIB-1 has been shown to be positive in other studies.20,23 These latter studies also revealed positive staining for antipancytokeratin antibodies [AE1/AE3] on the suprabasal lesional keratinocytes and for anticytokeratin 16, associated with a reduced expression of cytokeratin 2e.20 These findings would suggest a reactive proliferation triggered by some type of irritation secondary to loss of the corneal layer, or by altered keratinization.20 The antipancytokeratin antibodies [AE1/AE3] were also elevated in another study of a patient with multiple lesions, with increased but variable expression of cytokeratin K16 depending of the site of the lesion; cytokeratin K9 levels were reduced but also showed variations depending on the site of the lesion.31 In another report, cytokeratins K16 and K6 were weakly positive in a case of palmar hypokeratosis but negative in a case with plantar involvement.26 In that same study, a reduction in the expression of cytokeratin K9 and of connexin Cx26 was detected in the plantar lesion, with no variation in the levels in the keratinocytes of the acrosyringia, and both markers were normal in a case with a palmar lesion.26 These findings have led to the suggestion that there are at least 2 subtypes of hypokeratosis, depending on the site of the lesions, the presence of erythema, and the levels of cytokeratin K9 and connexin Cx26 expression. In the case of plantar lesions, the condition develops due to a failure of the lesional keratinocytes to undergo plantar-type keratinization, and they show regression towards interfollicular-type differentiation, as occurs on the trunk.26 In another study pancytokeratin AE1/AE3 was found to be positive, with reduced expression of cytokeratin K2e and K9, but an absence of changes in the expression of cytokeratin K16 or Ki-67.33
The immunohistochemical expression of claudin-1 has been studied in some cases of circumscribed palmar hypokeratosis, observing a marked reduction or absence of this protein (which forms part of the junctional complex between keratinocytes) in the lesional skin compared with the adjacent healthy skin; there was widespread intercellular expression of this protein in the healthy skin. Unfortunately, these findings have not been demonstrated in all cases studied (Requena L, unpublished data).
Additional TestsDermoscopyThe dermoscopic findings were first described by Ishiko et al.20 Without oil immersion, stepped desquamation was observed at the margin of the lesional. With oil immersion, a homogeneous erythema can be seen, with scattered with tiny white spots with a regular distribution. These findings have been confirmed by other authors.26,43 The histopathological correlation of these findings has also been defined; the stepped desquamation at the periphery of the lesion corresponds to stepped thinning of the corneal layer towards the center of the lesion,43 and the white spots on the erythema correspond to the acrosyringia.20,43 It has been suggested that the erythema may be due not only to vessels becoming visible because of transparency of the thin corneal layer, but also to the presence of dilated dermal capillaries.11,43
Polymerase Chain ReactionThe possibility of human papillomavirus (HPV) infection as an etiological cause of this disorder was investigated using the polymerase chain reaction (PCR) in 2 of the first 10 cases, with negative results.2 The presence of histological findings such as acanthosis, large keratohyaline granules, and tortuous capillaries led Boer and Falk12 to consider this etiology. Those authors demonstrated the presence of HPV4 in their only patient and suggested that circumscribed hypokeratosis is a rare clinical manifestation of common warts located on the palms or soles. HPV-6 has also been detected, in this case in a 49-year-old patient with a plantar lesion diagnosed as circumscribed hypokeratosis 10 years earlier.21 In her childhood the patient had undergone laser treatment for common warts at the same site. HPV infection has subsequently been investigated on several occasions, with exhaustive analysis of high- and low-risk nongenital and genital HPV in some studies,22 with negative results in all cases.15,20,21,24,31,32,34,36,41
PCR analysis for bacterial genes has revealed no differences in the bacteria present on healthy skin and on the lesions.20
TreatmentAt the present time there is no specific treatment for circumscribed palmar or plantar hypokeratosis. It typically has a prolonged clinical course and there has been only 1 report of a case that has undergone spontaneous resolution after 2 years.11 Complete surgical excision of the altered skin can be an option in small lesions, but in larger lesions it can be associated with technical difficulties or a poor outcome.7,9,15,21,31,41 Other therapeutic modalities are therefore preferred, as it is apparently a benign condition. Cryotherapy with liquid nitrogen was beneficial in 1 case, with no recurrence during follow-up of 1 year; in the opinion of those authors,17 the efficacy of the technique may be due to the destruction of an abnormal clone of keratinocytes and repopulation with normal epidermal cells. In another case cryotherapy was ineffective.24 Photodynamic therapy, used in 1 case, only achieved a partial reduction in the size of the lesion, though it was postulated that this could be useful as an initial therapy, prior to complete surgical excision.19
Regarding topical treatments, the use of corticosteroids has not been beneficial in any case,9,10,17,21,26,27,33,35 including when they are used in combination with topical retinoids.3 One patient, after treatment with 5-fluorouracil once or twice a day for 9 months, achieved resolution of a lesion on the index finger, with no subsequent recurrence after follow-up of more than 4 years38; however, no previous biopsy was reported. The same patient subsequently developed 3 new lesions, 2 on the thenar eminences and 1 on the middle finger; she was treated in the same way, with no improvement in the lesion on the finger and with a transitory improvement in the thenar lesions after 18 months of treatment, but with recurrence 3 months after stopping treatment. On that occasion, biopsy of 1 of the thenar lesions showed the specific findings of circumscribed hypokeratosis.38 There was no improvement after the use of topical 5-fluorouracil in 2 other patients.21,24 Topical calcipotriol was effective in 1 case, with complete regression after prolonged use for more than 4 years; the patient presented a slow but progressive improvement of a lesion that had been present and stable in size and shape for around 30 years.45 The changes were documented photographically. Towards the end of the period of therapy, tacalcitol was prescribed as calcipotriol was unavailable. This produced irritation of the lesion and a transitory deterioration that improved on the reinitiation of calcipotriol (Urbina F, unpublished data). Despite this promising outcome, topical calcipotriol has not been reported to be effective in other publications, although it was only used for a few months.9,10,20,21,25,28,34 Other topical therapies that have not been shown to be useful include 10% urea, vitaminA, tacrolimus, maxacalcitol,20 salicylic acid, 0.05% isotretinoin,2 ketoconazole,42 imiquimod,24 antibiotics,26 hydrocolloid dressings,32,34 and tazarotene.28
DiscussionAlthough the term hypokeratosis had been used previously (in only a single case) to describe atrophic epidermal lesions on the palms and soles, possibly in the context of mesoectodermal dysplasia associated with various other alterations in a child,46 it has become accepted as the name for the condition we discuss in this paper, giving rise to a particular histopathological concept and defining a new entity with distinctive characteristics. Some authors have suggested using the term acral hypokeratosis,7,21,24,44 a good term but one that, unfortunately, implies other acral or distal areas such as the nose and ears, which are not in any way involved in this condition as, to date, it has mainly affected the palms and soles.
The histogenesis of the lesion is unknown. Studies using PCR to investigate the presence of material from the HPV genome have been negative in practically all cases, except for 2 patients in whom DNA from HPV4 and HPV6 was identified in the skin lesions.12,21
Immunohistochemical studies have revealed an abnormal immunophenotype of cytokeratin expression in the skin lesions20 on comparison with the adjacent normal epidermis. This would suggest that the condition is actually a disorder of epidermal keratinization rather than a lesion induced by trauma, as has been proposed by some authors.5,11,17,19,21,32,41 The existence of a case of congenital circumscribed palmar hypokeratosis would also support this being a disorder of keratinization rather than an acquired traumatic disorder.44
There is a report of a case in which circumscribed palmar hypokeratosis was associated with disseminated superficial actinic porokeratosis; this relationship may have been purely coincidental or it may indicate a common etiological and pathogenic origin, in which clones of abnormal keratinocytes could induce one or both conditions in genetically predisposed individuals.36
Although circumscribed hypokeratosis has shown a benign behavior to date, with no reports of malignant change despite its prolonged clinical course in many cases, there has been a recent report of its association with actinic keratosis arising within an area of hypokeratosis in a patient with prolonged exposure to sunlight and with no history of exposure to arsenic.34 The authors concluded that the thinning of the corneal layer would make the underlying keratinocytes more susceptible to photocarcinogenesis and they alerted us to a possible premalignant nature of the disorder and recommended appropriate follow-up.34
ConclusionBased on the findings of various studies performed during the decade after the first description of circumscribed palmar or plantar hypokeratosis, the condition may currently be considered to be a focal, noninflammatory disorder of keratinization that affects areas with a thick stratum corneum. The precipitating cause is unknown and its definitive treatment still remains to be defined. It occurs due to localized, clonal keratinocyte failure, with an alteration of differentiation into a normal hyperkeratotic epidermis of the palmoplantar type. Other important questions remain concerning its apparent inexistence up to 10 or however many years ago and why it has appeared gradually in various areas of the world, if we do not consider publication for novelty.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
To Professor Evaristo Sánchez Yus of Madrid, Spain, who fittingly proposed the name of palmar hypokeratosis for the condition after studying the first histopathology slides.
Please cite this article as: Urbina F, Pérez A, Requena L, Rütten A. Hipoqueratosis circunscrita palmar o plantar. Conocimientos y controversias tras 10 años de su descripción. Actas Dermosifiliogr. 2014;105:574–582.