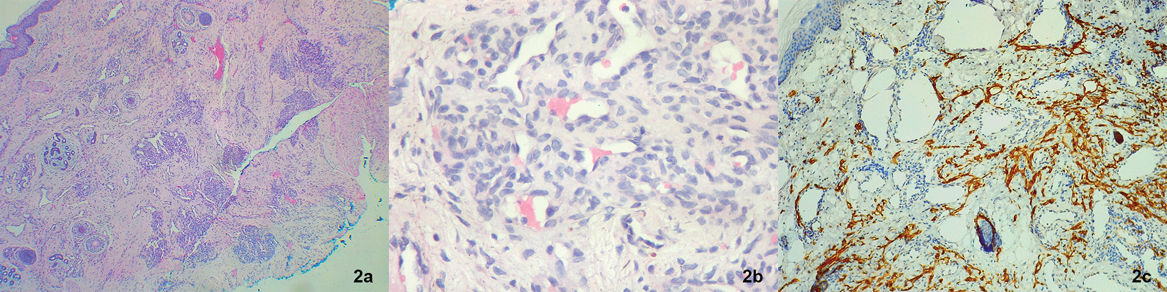
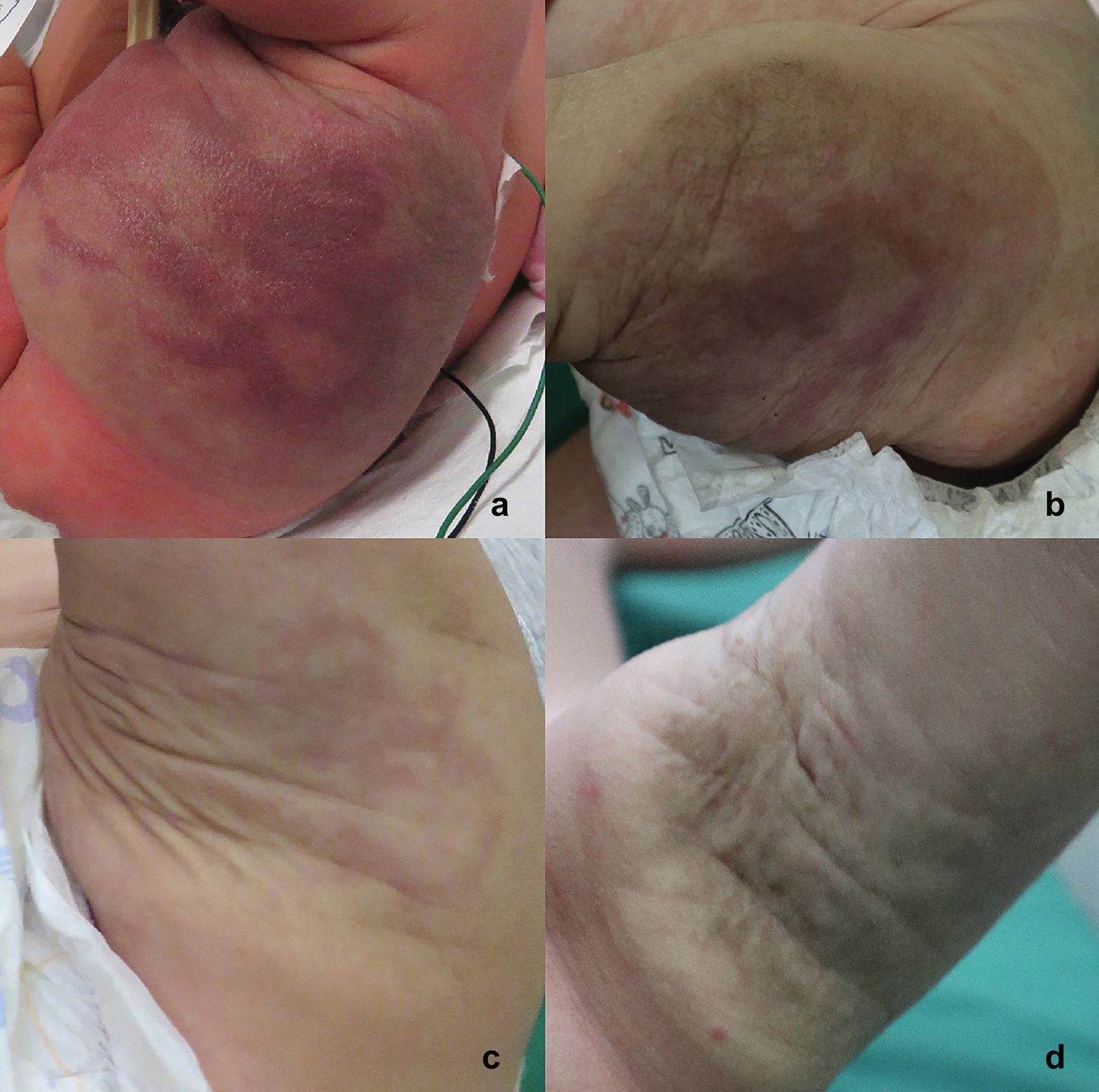
A full-term newborn—the result of a monitored, uncomplicated pregnancy—was evaluated at 3 days of life for a congenital vascular tumor located on her left lower limb, with no other relevant medical history. Physical examination revealed a soft 8cm×6cm erythematous–violaceous tumor with a purpuric center, along with peripheral pale halo, and areas of hypertrichosis on the left thigh (Fig. 1). Doppler ultrasound of the lesion showed increased thickness and echogenicity of subcutaneous tissue, with dilated vascular images extending into the muscle plane. Doppler echocardiography revealed no signs of cardiac overload. Blood test showed a normal hematological profile, and abdominal and brain ultrasounds were unremarkable. Histopathological examination of the tumor revealed a proliferation of spindle-shaped cells arranged in nodules, outlining the capillaries. While some of these nodules were surrounded by crescent-shaped larger vessels, others were arranged in solid islands. Immunohistochemical staining tested positive for D2-40, CD31, and WT1, but negative for GLUT1 (Fig. 2).
What is your diagnosis?
DiagnosisTufted angioma/Kaposiform hemangioendothelioma.
Course of the disease and commentaryThe clinical and pathological findings confirmed the diagnosis of tufted angioma/kaposiform hemangioendothelioma (TA/KHE). Over time, the lesion progressively decreased in size (Fig. 3), with no associated hematological abnormalities at the 11-month follow-up. Consequently, a strict interdisciplinary clinical follow-up with pediatricians, dermatologists, and radiologists was adopted, without pharmacological treatment.
Tufted angioma (TA) and kaposiform hemangioendothelioma (KHE) are rare vascular tumors categorized by the International Society for the Study of Vascular Anomalies (ISSVA) as benign and locally aggressive, respectively. Due to their similar histopathological characteristics and potential to develop the Kasabach–Merritt phenomenon (KMP), some authors consider them part of the same disease spectrum.1
TA/KHE has been associated with a slightly male predominance2,3 and has been linked to genetic mutations in the GNAQ family and, in some cases, GNA14 mutations.4
TAs typically present as erythematous–violaceous plaques or tumors in children and young adults, with rare congenital presentation.1,5 They can be associated with hyperhydrosis or hypertrichosis and are commonly located on the lower limbs. Some lesions—especially congenital cases—undergo spontaneous regression,1,5,6 as observed in our patient. KHE show as erythematous–violaceous plaques or tumors that may involve superficial or deep skin layers, behaving as locally aggressive tumors capable of affecting deeper tissues.1,7 These are mainly found on the extremities and less commonly on the trunk, retroperitoneum, head and neck, mediastinum, and organs such as the thymus and spleen.2,3,7 They usually occur within the first year of life. Approximately half of KHE cases are evident at birth.2,3 Complications are more common in KHE and include KMP, pain, functional limitation, lymphedema, and compression of vital structures such as the airway.2,3 KMP occurs in up to 70% of KHE cases and 10% of TA cases3,7 and is characterized by severe thrombocytopenia and consumptive coagulopathy, which can be life-threatening.2,3,7 Risk factors include early age (<6 months), trunk location, lesions>5cm, and deep involvement,3 as in our patient. Diagnosis is based on clinical presentation and confirmed through histopathological examination.2 Histology reveals spindle-shaped endothelial cells forming well-demarcated, rounded nodules aligned to create lymphatic channels and crescent-shaped vascular structures. This appearance—known as the “cannonball pattern”—is characteristic of TA. In KHE, these spindle cells form solid sheets.2,6
Immunohistochemistry shows positivity for vascular endothelial (CD31 and CD34) and lymphatic markers (D2-40, LYVE-1, Prox-1, and VEGFR-3) but negativity for GLUT1.2,6 Differential diagnoses include infantile hemangioma, congenital hemangioma, venous malformations, and kaposiform lymphangiomatosis, among others.2 Treatment of TA/KHE depends on lesion size, depth, disease progression, and presence of complications. Therapeutic options include surgical procedures, pharmacological treatment,7 and sometimes clinical observation. Pharmacological treatments may include corticosteroids, vincristine, and sirolimus (0.8mg/m2/day orally, targeting plasma levels of 5–10μg/dL without coagulopathy or 10–15μg/dL with coagulopathy).2,6–8
Conflicts of interestNone declared.