Vaccination is an essential measure in preventive medicine. However, it is not free from complications, since it can lead to adverse reactions, although these are mainly mild, transient, and self-limiting1. The reactions are rarely persistent, with most cases involving a hypersensitivity reaction to aluminum2,3.
We report the cases of 2 girls (age, 2 and 3 years) and a boy (8 years) who experienced persistent cutaneous reactions after vaccination (Table 1). All 3 patients developed nodules at the injection site, and in 1 case, the reaction was accompanied by eczema and hypertrichosis, which had first appeared more than 1 year previously (Fig. 1)4. The vaccinations had been administered according to the corresponding schedule, and the clinical picture was associated with the vaccines included in the schedule. Given that the clinical suspicion included other conditions in 2 cases, diagnosis was based on skin biopsy, which revealed findings typical of this type of reaction (histiocytes with granular cytoplasm) (Fig. 2). All 3 patients underwent patch testing with aluminum chloride 2% in petrolatum (Chemotechnique), which yielded positive readings at 72 and 168 hours (Fig. 3).
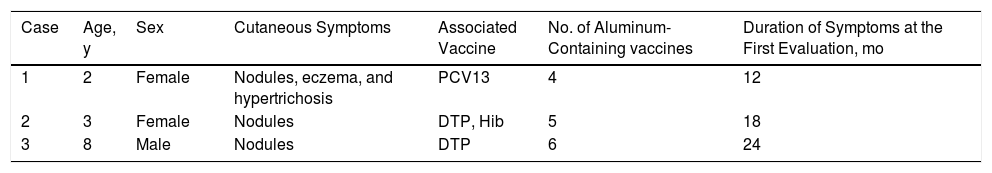
Summary of Cases of Contact Allergy to Aluminum.
| Case | Age, y | Sex | Cutaneous Symptoms | Associated Vaccine | No. of Aluminum-Containing vaccines | Duration of Symptoms at the First Evaluation, mo |
|---|---|---|---|---|---|---|
| 1 | 2 | Female | Nodules, eczema, and hypertrichosis | PCV13 | 4 | 12 |
| 2 | 3 | Female | Nodules | DTP, Hib | 5 | 18 |
| 3 | 8 | Male | Nodules | DTP | 6 | 24 |
Abbreviations: DPT, diphtheria, pertussis, tetanus; Hib: Haemophilus influenzae b; PCV, pneumococcal conjugate vaccine.
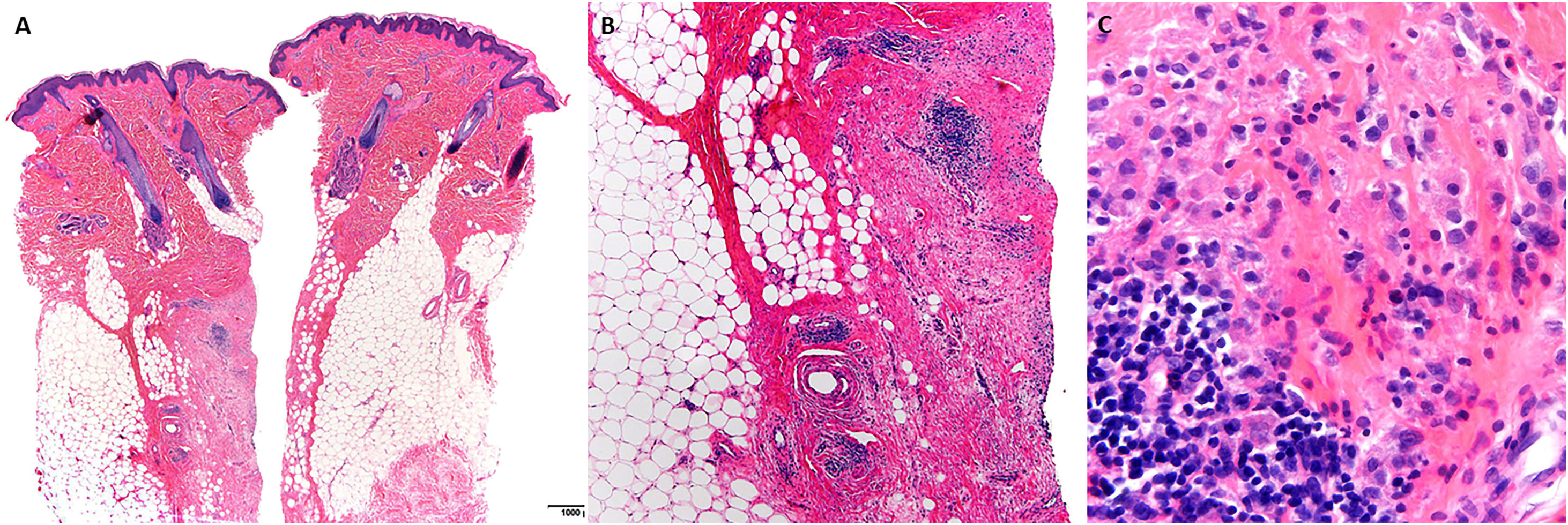
Skin biopsy from one of the case reports. A, Normal epidermis, with lesions mainly in the dermis and subcutaneous cellular tissue (hematoxylin-eosin, ×4). B, Areas of sclerosis, together with follicular lymphoid hyperplasia and histiocytic infiltrate (hematoxylin-eosin, ×4). C, Histiocytes with granular cytoplasm (hematoxylin-eosin, ×20).
Aluminum compounds have been used as adjuvants in vaccines for more than 80 years to boost the immune response to the antigen. Administration of vaccines can lead to cutaneous lesions, mostly in the form of pruritus or subcutaneous nodules; areas of hypertrichosis or eczema are less common. The reactions persist in 0.5%–6% of cases, mainly because of a type IV hypersensitivity reaction to aluminum hydroxide. Patch testing with aluminium hydroxide 2% is positive in 77%–95% of children with persistent reactions, thus demonstrating the presence of contact allergy to the metal5.
Various histologic patterns have been described (panniculitis, pseudolymphomatous, granuloma annulare–like), although the characteristic finding is histiocytes with a granular cytoplasm. Nevertheless, given the high sensitivity of patch testing, skin biopsy is not considered essential for diagnosis5,6.
The lesions generally appear at 12–18 months of life, mostly after several vaccinations (usually after the third) and with subcutaneous vaccines. It is thought that, at the subcutaneous level, aluminum comes into contact with dendritic cells, thus triggering a hypersensitivity reaction. The reactions usually occur 2.5 months after the vaccination, although reports indicate that this interval can vary from 2 weeks to 13 months. The duration of symptoms also varies widely, from months to up to 10 years5.
Children who are sensitized to aluminum can experience contact dermatitis when exposed to objects that contain it (e.g., deodorants, toothpaste, pigments used in tattoos). However, some studies show that contact allergy to aluminum can diminish or disappear over time, with negative results in up to 77% of cases 7 years after the initial positive patch test reading7.
Aluminum-containing vaccines should be replaced by aluminum-free vaccines in patients with contact dermatitis to aluminum. However, since not all vaccines have an aluminum-free version, the patient should receive a deep intramuscular injection to reduce the risk of new lesions in cases where no substitute is available. In general terms, the benefits of vaccines outweigh potential complications; therefore, the appearance of the lesions does not justify nonadherence to the vaccination schedule. Similarly, given that aluminum is also a standard adjuvant in subcutaneous allergen-specific immunotherapy, contact allergy to aluminum is a relative contraindication.
It is essential to be aware of the cutaneous complications associated with administration of vaccines. Consequently, in the case of a persistent reaction after administration, we should consider the presence of contact allergy to aluminum. A suggestive clinical history, together with positive patch tests results, should be sufficient to confirm the diagnosis. Early diagnosis will prevent parental anxiety and other, unnecessary and invasive procedures.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tous Romero F, Palencia Pérez SI, Rodríguez Peralto JL, Ortiz de Frutos FJ. Alergia de contacto a aluminio tras vacunación: presentación de tres casos. Actas Dermosifiliogr. 2021;112:930–932.