Contact dermatitis is a common reason for consultation in dermatology. Sensitization levels and frequency, however, vary from one population to the next. The aim of this study was to review patch test results showing sensitization to allergens in the Spanish standard series in the Canary Islands, where a large proportion of the population works in tourism.
Material and methodsRetrospective, descriptive study of data from the dermatology department's contact dermatitis unit at Complejo Hospitalario Universitario Insular in Las Palmas de Gran Canaria, Spain. We studied results recorded for patients patch tested with the Spanish standard series between January 2005 and June 2018.
ResultsData for 1568 patients were studied; 71.6% were women, and overall rates of atopy (14.2%) and occupational dermatitis (15.8%) were low. Most patients with a positive test (65.2%) were older than 40years. The main allergens eliciting positive reactions were nickel (36.5%), methylchloroisothiazolinone/methylisothiazolinone (11.9%), methylisothiazolinone (11.8%), paraphenylenediamine (7.5%), and potassium dichromate (6.3%).
ConclusionsContact sensitization rates were higher than those reported elsewhere in Spain for most of the allergens studied. The differences were particularly notable for nickel, methylchloroisothiazolinone/methylisothiazolinone, and paraphenylenediamine.
El eccema de contacto es un motivo frecuente de consulta. El grado y la frecuencia de sensibilización a alérgenos varían dependiendo de la población de referencia atendida. Revisamos los resultados de sensibilización a alérgenos de la Batería Estándar Española en una población dedicada mayoritariamente al sector turístico (Islas Canarias).
Material y métodosEstudio descriptivo retrospectivo tomando la base de datos de la Unidad de Dermatitis de Contacto del Servicio de Dermatología del Complejo Hospitalario Universitario Insular de Las Palmas de Gran Canaria, incluyéndose pacientes parcheados con la Batería Estándar Española desde enero de 2005 hasta junio de 2018. Se recogieron edad, sexo, atopia, localización, positividades y relevancia.
ResultadosSe estudiaron 1.568 pacientes; 71,6% fueron mujeres, con una baja proporción de atopia (14,2%) y dermatitis ocupacional (15,8%). La mayoría fueron mayores de 40 años (65,2%). Los alérgenos positivos más frecuentes fueron níquel (36,5%), metilcloroisotiazolinona/metilisotiazolinona (11,9%), metilisotiazolinona (11,8%), parafenilendiamina (7,5%) y dicromato potásico (6,3%).
ConclusionesEn la población estudiada se observa una mayor frecuencia de sensibilización respecto al resto de España para la mayoría de los alérgenos, siendo estas diferencias especialmente llamativas en el caso del níquel, de la metilcloroisotiazolinona/metilisotiazolinona y de la parafenilendiamina.
Contact dermatitis affects up to 20% of the population1 and is a common reason for visiting the dermatologist. Allergic contact dermatitis may be clinically indistinguishable from irritant contact dermatitis and endogenous contact dermatitis. Therefore, patch testing is essential when confirming a diagnosis.2 Patch tests group allergens in series according to the type of exposure.3 The standard series brings together the allergens that most frequently lead to sensitization, either at the national or the international level.4,5 Contact dermatitis guidelines recommend using the standard series—in our case, the Spanish standard series—on all patients who undergo patch testing, which should be completed with specific series.
In Spain, the Spanish Contact Dermatitis and Skin Allergy Research Group (Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea [GEIDAC]) has been responsible for creating and updating the Spanish standard series for more than 40years.4,6 This dynamic series is updated according to the frequency of sensitization to allergens assessed by GEIDAC. The most recent update was in 2016. This included methylisothiazolinone, diazolidinyl urea, and imidazolidinyl urea and removed clioquinol, thiomersal, mercury, and primin.6 It was previously modified in 2012 by replacing Euxyl K400 with methyldibromo glutaronitrile. Also added were phenoxyethanol, primin, fragrance mix II, and lyral,7 with respect to the previous modification in 2001, when Euxyl K400, budesonide, and tixocortol pivalate were added.
Given that it is impossible and ethically questionable to perform patch testing on the whole population, almost all epidemiology studies are based on the frequency of sensitization in patients assessed in contact dermatitis units.8,9 Obviously, this epidemiological approach assumes that the data may not be homogeneous and will differ according to the center they come from. The MOAHLFA index (Male, Occupational dermatitis, Atopy, Hand, Leg, Face, Age>40) for each study population can be used to determine whether samples from different geographical areas are comparable. This indicator expresses in percentage terms the epidemiological characteristics of the study population that could affect the results of patch testing a priori.10,11
The frequency of sensitization reported for allergic contact dermatitis caused by allergens from the standard series varies depending on the population that visits the unit, the selection criteria set for patch testing patients, and the percentage of patients treated for occupational exposure.3 Complejo Hospitalario Universitario Insular Materno Infantil (CHUIMI) belongs to the Health Service of the Canary Islands and is the dermatology reference center for south Gran Canaria. The center serves a population of around 400000 persons, many of whom work in the tourist industry.
Given that the description and the epidemiological follow-up of the sensitizers found in each unit represent the most valid approach for determining the main types of sensitization,3 we believe the results of CHUIMI should be reviewed over a long period. Similarly, data analysis is one of the main quality assurance criteria in our unit. The objective of the present study was to analyze the results for the Spanish standard series at CHUIMI from 2005 and 2018 and to compare them with widely available public data and data from other centers.6,12,13
Material and MethodsWe performed a retrospective descriptive study using the database of the Contact Dermatitis Unit of the Dermatology Department of CHUIMI, Las Palmas de Gran Canaria, Spain and Access Office, Version 2007. The study was approved by the Research Ethics Committee of the Canary Islands Health Service on April 7, 2020. The data collected were age, sex, personal history of atopic dermatitis, site affected, profession, positive readings at 96hours, and relevance of the positive findings.
We included patients who underwent patch testing with the standard Spanish series between January 2005 and June 2018. Patch testing was with the True Test series (SmartPractice Denmark ApS) and additional allergens according to the GEIDAC guidelines.6,13 Thereafter, testing was with the Spanish standard series from Allergeaze (MartiTor Alergia S.L.). The allergens from the last update of the standard series were used from January 1, 2016 onward. In order to ensure continuity over time, Euxyl K400 and methyldibromo glutaronitrile were considered statistically similar, as were quinoline mix and clioquinol.
The patch tests were performed according to the guidelines of the European Society of Contact Dermatitis (ESCD).2 Readings were taken at 48 and 96hours in all cases, and a late reading was taken in patients suspected of having allergy to corticosteroids. Patients were asked to return at 168hours if they developed late positive results. We took into account positive results (+, ++, or +++), and relevance was established based on the patient's symptoms and history of allergen exposure.
In the statistical analysis, we used the Pearson χ2 test to compare proportions and calculated the 95% CI for the difference in proportions. P values<.05 were considered statistically significant. Age and sex were adjusted for the scale of the European Surveillance System on Contact Allergies, as follows: woman aged under 40years, 32.5%; woman older than 40years, 32.5%; man under 40years: 32.5%; and man older than 40years, 32.5%. The statistical analysis was performed using R Core Team 2020, Version 4.0.2.
ResultsWe included 1568 patients, of whom 71.6% were women. Few patients had occupational dermatitis or atopy (Table 1).
Sex- and Age-Adjusted MOAHLFA Index.
| MOAHLFA parameter | No. (%) | % Standardized by sex/age (95% CI) |
|---|---|---|
| Male | 28.4% (445) | |
| Occupational | 15.8% (246) | 17.3% (15.4–19.2%) |
| Atopy | 14.2% (222) | 15.7% (13.9–15.6%) |
| Hand | 34.1% (534) | 36.1% (33.7–38.5%) |
| Legs | 18.1% (286) | 18.1% (16.2–20%) |
| Face | 35.2% (555) | 32.5% (30.2–34.9%) |
| Age>40 y | 65.2% (1023) |
The most frequent sensitizations were for nickel (36.5%), methylchloroisothiazolinone/methylisothiazolinone (MCl/MI) (11.9%), methylisothiazolinone (11.8%), paraphenylenediamine (7.5%), and potassium dichromate (6.3%). These allergens were also associated with the highest frequency of present relevance. The positive results and relevance are shown in Table 2. Given the variability in the criteria used to assign relevance, this parameter was not taken into consideration for the discussion of the most frequent allergens.
Positive Results and Present Relevance.
| Allergen | No. (%) | Relevance, No. (%) |
|---|---|---|
| Nickel | 572/1568 (36.5) | 124/1568 (7.9) |
| MCl/MI | 187/1568 (11.9) | 110/1568 (7) |
| Methylisothiazolinoneb | 62/524 (11.8) | 42/524 (8) |
| Paraphenylenediamine | 118/1568 (7.5) | 77/1568 (4.9) |
| Potassium dichromate | 98/1568 (6.3) | 60/1568 (3.8) |
| Cobalt chloride | 91/1568 (5.8) | 29/1568 (1.8) |
| MDBGN/Euxyl K400 | 58/1568 (3.7) | 11/1568 (0.7) |
| Fragrance mix IIa | 19/524 (3.6) | 13/524 (2.5) |
| Fragrance mix I | 48/1568 (3.1) | 30/1568 (1.9) |
| Carba mix | 45/1568 (2.9) | 12/1568 (0.8) |
| Thiuram mix | 43/1568 (2.7) | 17/1568 (1.1) |
| Balsam of Peru | 41/1568 (2.6) | 12/1568 (0.8) |
| P-tert-Butylphenol formaldehyde resin | 38/1568 (2.4) | 18/1568 (1.2) |
| Colophony | 31/1568 (2) | 13/1568 (0.8) |
| Formaldehyde | 27/1568 (1.7) | 9/1568 (0.6) |
| Lyrala | 9/524 (1.7) | 6/524 (1.2) |
| Mercaptobenzothiazole | 22/1568 (1.4) | 15/1568 (1) |
| Caine mix | 21/1568 (1.3) | 5/1568 (0.3) |
| IPPD/Black rubber mix | 20/1568 (1.3) | 9/1568 (0.6) |
| Epoxy resin | 18/1568 (1.2) | 5/1568 (0.3) |
| Mercapto mix | 16/1568 (1) | 11/1.568 (0.7) |
| Wool alcohols | 15/1568 (1) | 10/568 (0.6) |
| Ethylenediamine dichloride | 14/1568 (0.9) | 6/1568 (0.4) |
| Quaternium-15 | 12/1568 (0.8) | 3/1568 (0.2) |
| Neomycin sulfate | 10/1568 (0.6) | 1/1568 (0.1) |
| Budesonide | 3/524 (0.6) | 0/524 (0) |
| Phenoxyethanola | 2/524 (0.4) | 1/524 (0.2) |
| Imidazolidinyl ureab | 2/524 (0.4) | 1/524 (0.2) |
| Parabens mix | 4/1568 (0.3) | 1/1568 (0.1) |
| Diazolidinyl ureab | 1/524 (0.2) | 0/524 (0) |
| Lactone mix | 1/1568 (0.1) | 1/1568 (0.1) |
| Tixocortol pivalate | 1/1568 (0.1) | 1/1568 (0.1) |
| Thiomersalc | 65/1190 (5.5) | 6/1190 (0.5) |
| Mercuryc | 29/1190 (2.4) | 1/1190 (0.1) |
| Primina,c | 3/517 (0.6) | 1/517 (0.2) |
| Clioquinol/quinoline mixc | 4/1190 (0.3) | 2/1190 (0.2) |
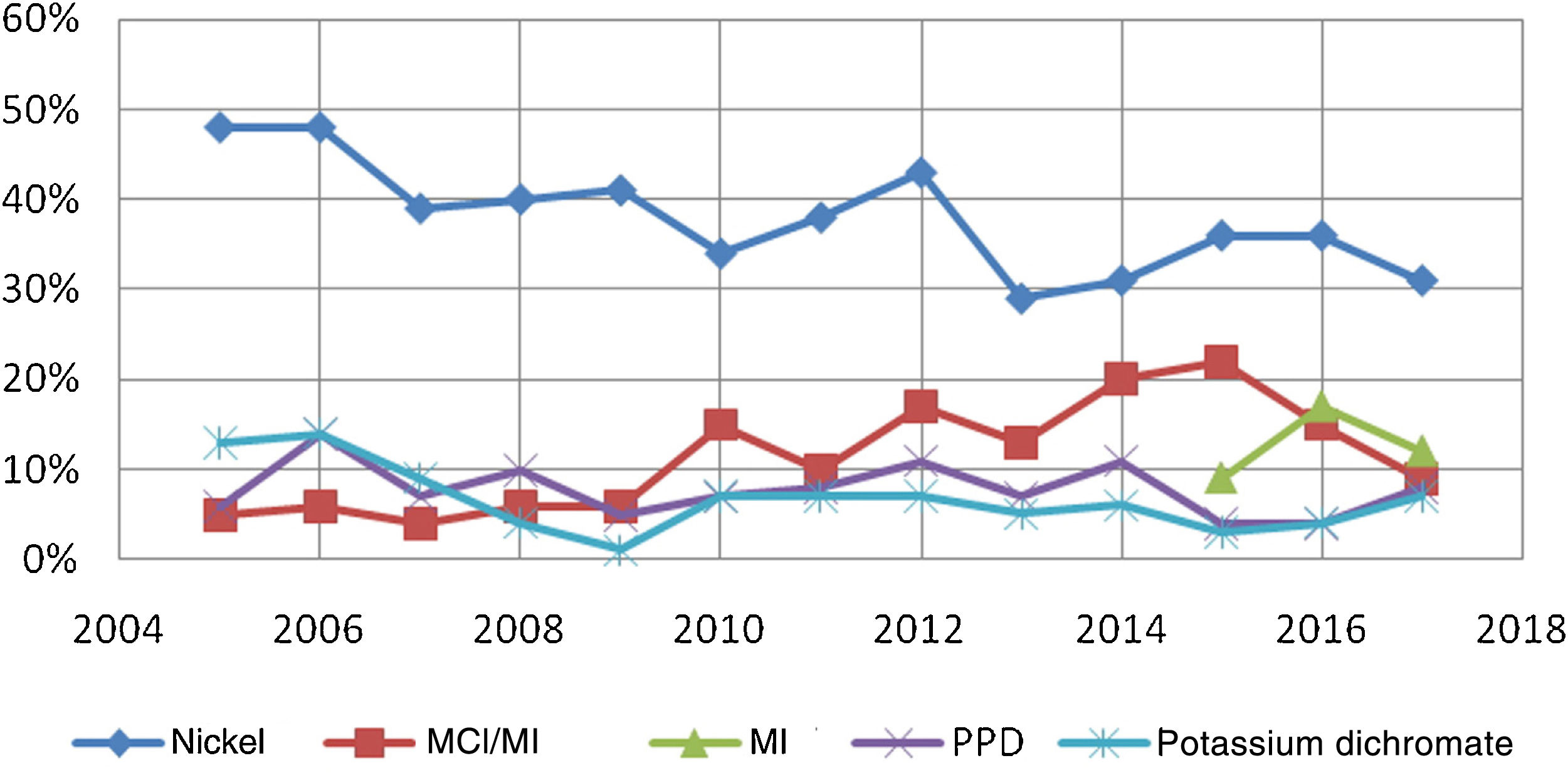
Fig. 1 shows changes in sensitization to the 5 most common allergens over time.
DiscussionOur study showed the frequency of sensitization to allergens from the Spanish standard series among the population of the south of Gran Canaria, an island that is characterized by a subtropical climate, European population, and a local economy based on the tourist industry.
Our search of the Spanish medical literature revealed 3 studies that analyzed the Spanish series during the same period: 1 performed in Marbella between 2005 and 201012 and 2 multicenter studies performed in 200813 and 2012.6 It is important to note that the population of the latter multicenter study includes the patients assessed in the present study. A key finding of these studies was the greater frequency of sensitization in the sample from CHUIMI. This is more noticeable for the most common allergens, such as nickel, MCl/MI, methylisothiazolinone, and paraphenylenediamine (Table 3). The difference in the percentage of patients sensitized could be explained by epidemiological differences in the MOAHLFA index (Table 4), especially the higher percentage of women in the sample studied, which increases the frequency of sensitization for most of the allergens.1 Another epidemiological peculiarity of the study population is that many people work in the tourist sector—with high seasonal variations in winter—and the care provided is for common illnesses in the Canary Islands Health Service. The greater frequency of “block” sensitization could also be explained by the working method14 of the Dermatology Department of CHUIMI, where new histories are taken irrespective of whether the referral is by a dermatologist or other specialist, with patch testing recommended at the discretion of the person in charge of the unit. Therefore, we calculate that two-thirds of the patients referred eventually undergo patch testing. However, the high percentage of patients with a positive result and the low percentage of patients with present relevance are striking (Table 5).
Comparison With Studies Performed Elsewhere in Spain.
| Allergen | GC 2005–2018 | Marbella 2005–201012 | Spain 200813 | Spain 20126 |
|---|---|---|---|---|
| Nickel | 36.5% | 25.9% | 25.4% | 25.3% |
| MCl/MI | 11.9% | 3.7% | 2.8% | 8.4% |
| Methylisothiazolinoneb | 11.8% | – | – | 5.2% |
| Paraphenylenediamine | 7.5% | 3.5% | 4.2% | 4.5% |
| Potassium dichromate | 6.3% | 7.6% | 5.8% | 5% |
| Cobalt chloride | 5.8% | 4.5% | 5.2% | 5.3% |
| MDBGN/Euxyl K400 | 3.7% | – | – | 2.1% |
| Fragrance mix IIa | 3.6% | – | – | 2.9% |
| Fragrance mix I | 3.1% | 3.8% | 5% | 4.4% |
| Carba mix | 2.9% | 2.7% | 1.5% | 2% |
| Thiuram mix | 2.7% | 2.4% | 2.2% | 1.7% |
| Balsam of Peru | 2.6% | 0.7% | 5.1% | 2.5% |
| P-tert-Butylphenol formaldehyde resin | 2.4% | 3% | 0.7% | 1.5% |
| Colophony | 2% | 1.9% | 1.2% | 1.4% |
| Formaldehyde | 1.7% | 0.6% | 2.6% | 1.4% |
| Lyrala | 1.7% | – | – | 1.2% |
| Mercaptobenzothiazole | 1.4% | 0.6% | 0.9% | 0.4% |
| Caine mix | 1.3% | 1.9% | 1.7% | 1.5% |
| IPPD/Black rubber mix | 1.3% | 1.7% | 1.2% | 0.8% |
| Epoxy resin | 1.2% | 0.8% | 0.7% | 1.1% |
| Mercapto mix | 1% | 0.4% | 1.6% | 0.6% |
| Wool alcohols | 1% | 0.7% | 0.7% | 0.6% |
| Ethylenediamine dichloride | 0.9% | 1.3% | 1.1% | 0.9% |
| Quaternium-15 | 0.8% | 1.3% | 1.3% | 1% |
| Neomycin sulfate | 0.6% | 0.5% | 1.2% | 0.9% |
| Budesonide | 0.6% | 0.5% | 1.4% | 0.6% |
| Phenoxyethanola | 0.4% | – | – | 0.4% |
| Imidazolidinyl ureab | 0.4% | 0% | – | 0.5% |
| Parabens mix | 0.3% | 0.1% | 0.3% | 0.4% |
| Diazolidinyl ureab | 0.2% | 0.2% | – | 0.6% |
| Lactone mix | 0.1% | 0% | 0.2% | 0.5% |
| Tixocortol pivalate | 0.1% | 0.8% | 0.2% | 0.6% |
| Thiomersalc | 5.5% | 5.1% | 3.8% | 4.4% |
| Mercuryc | 2.4% | 2.4% | 2.5% | 3% |
| Primina,c | 0.6% | – | – | 0.1% |
| Clioquinol/quinoline mixc | 0.3% | 0.2% | 0.5% | 0.1% |
Comparison of the MOAHLFA Indices.
| Gran Canaria 2005–2018 | Marbella 2005–201012 | Gran Canaria-MarbellaP value (95% CI) | Spain 200813 | Gran Canaria-Spain 2008P value (95% CI) | Spain 201230 | Gran Canaria-Spain 2012P value (95% CI) | |
|---|---|---|---|---|---|---|---|
| Male | 28.4% | 36.7% | <.001 (−0.12 to 0.04) | 36.3% | <.001 (−0.12 to −0.04) | 35.9% | <.001 (−0.1 to −0.05) |
| Occupational | 15.7% | 18.8% | .056 (−0.06 to 0) | 14.6% | .485 (−0.02 to 0.04) | 10.4% | <.001 (0.03–0.07) |
| Atopy | 14.2% | 15.9% | .291 (−0.05 to 0.01) | 10.9% | <.05 (0.01–0.06) | 18.3% | <.001 (−0.06 to −0.02) |
| Hand | 34.1% | 36.1% | .334 (−0.06 to 0.02) | 28.7% | <.05 (0.02–0.09) | 26.8% | <.001 (0.04–0.1) |
| Legs | 18.2% | 9.8% | <.001 (0.06–0.11) | 9.3% | <.001 (0.06–0.12) | 12.2% | <.001 (0.04–0.08) |
| Face | 35.4% | 13.9% | <.001 (0.18–0.25) | 15.2% | <.001 (0.17–0.23) | 26.6% | <.001 (0.06–0.12) |
| Age > 40 | 65.2% | 59.8% | <.05 (0.01–0.1) | 65.5% | .901 (−0.04 to 0.03) | 62.3% | <.05 (0–0.06) |
Given that a contact allergen is included in the standard series if its frequency of sensitization is greater than 0.5%–1%,3,6 the data reported by CHUIMI support the 2016 update of the Spanish standard series, highlighting methylisothiazolinone and fragrance mix II, which are in the “top 10” of the updated series. Similarly, it seems reasonable to include lyral (2%), but not diazolinidyl urea, imidazolidinyl urea, or phenoxyethanol, whose frequency in the present study was 0.4%. As for the allergens removed from the series, the elimination of clioquinol seems justified. Both thiomersal and mercury had a high frequency of sensitization; however, they were withdrawn from the standard series because they have been prohibited in Europe since 2005 and have scarce clinical relevance. Primin was withdrawn because it is infrequent in Spain.6
Below, we discuss the 5 most common allergens in the series: nickel, MCl/MI, methylisothiazolinone, paraphenylenediamine, and potassium dichromate.
NickelNickel is a metal belonging to the alloy group, and its salts cause dermatitis. Release of nickel and subsequent penetration of the skin are favored by sweating. Patients generally become sensitized at an early age through earrings.12 The prevalence of sensitization to nickel has traditionally been greater in Spain than in Europe.15 A European regulation on release of nickel from jewelry was drafted in 1994, although it did not come into force until 2001. Fig. 1 shows the progressive decrease in sensitization among the study population. However, consistent with data reported elsewhere, the percentage of patients with present relevance remains high.16
The greater frequency of sensitization in the present sample may be explained mainly by the higher percentage of women.1,15 A study performed in the population of Tenerife17 also shows a very high frequency of sensitization; therefore, in addition to sex, local or geographic factors could favor sensitization. Factors to be considered include greater sweating owing to the higher temperatures in the Canary Islands or more frequent use of jewelry in our setting.
It has been postulated that oral exposure to nickel can lead to immune tolerance. The use of orthodontic appliances before body piercing has been shown to be a protective factor for sensitization to nickel.18 Similarly, populations that drink water with a high nickel content are less likely to become sensitized.19 Daily nickel intake in the Canary Islands is lower than the established average intake and even lower than in most European countries studied.20 This factor might also account for the discrepancy found in the present study population.
Methylchloroisothiazolinone/methylisothiazolinone and methylisothiazolinoneMCl/MI (mix of both components, more commonly known as Kathon CG) and methylisothiazolinone are preservatives that have been used in Europe as biocides in cosmetics. They are currently authorized for use in cleaning products, paints, and other industrial products. Employment in a profession that involves contact with these products is considered a risk factor for sensitization. Since 2015, MCl/MI has been banned in leave-on cosmetic products. Methylisothiazolinone was added in 2016 and limited to a maximum content of 15ppm in rinse-off products in 2017.21 Successive changes to legislation have been accompanied by a decrease in the frequency of sensitization in the present study population (Fig. 1) and in the remaining Spanish studies.22
Two facts may partially account for the high frequency of sensitization to MCl/MI and methylisothiazolinone in the study sample. Sensitization to these allergens is more common in women12,22 and is associated with working as a cleaner, as previously assessed in the CHUIMI population.23,24 Most of the sample are engaged in seasonal work in the tourist sector, thus accounting for the high frequency of sensitization. While the Marbella study, which was performed in 2005–2010, found that only 3.7% of patients were sensitized to MCl/MI,12 this percentage may have increased in subsequent years, as occurred in Valencia, where the frequency of sensitization rose from 4.5% in 2010 to 18.9% in 2015.22 A high frequency of sensitization to methylisothiazolinone was also reported in Valencia, reaching 8.8% in 2013.25
ParaphenylenediamineParaphenylenediamine is used as an industrial dye, hair dye, and domestic dye. Despite the 2009 regulation that sets a maximum concentration of 2% for paraphenylenediamine in hair dyes and its prohibition in temporary and permanent tattoos, these continue to the be main sources of sensitization.26 A study performed in the CHUIMI population showed a correlation between age of the sensitized patients and source of the sensitization, which was mainly henna tattoos in children, occupational contact (hairdressing) in middle-aged patients, and hair dye in older (female) patients.27Fig. 1 shows that sensitization to paraphenylenediamine remained stable in the study population, as is the case in the remaining series.28
The risk factors for sensitization to paraphenylenediamine are female sex,28 age>40years,27,28 use of darker colors,26 and profession (hairdressing, driving, cleaning, and printing).28 Data on the greater prevalence of sensitization to paraphenylenediamine in the CHUIMI population have already been published.27 Given the risk factors mentioned above, this higher frequency seems to be associated with a higher percentage of women and a mean age greater than in other series (Table 4). There may also be a difference in the distribution of professions compared with the other centers,4 given that 5.5% of the patients analyzed were hairdressers-beauticians.
Potassium dichromateThe most common sources of exposure are wet cement and chrome-treated leather products. The use of cements with more than 2ppm of chrome has been banned since 201529; Fig. 1 shows a decrease in sensitization to this allergen in the present study population.
Although the percentage of patients sensitized to chrome was high in our study, those observed in other parts of Spain were higher.12 Given that sensitization to chrome has traditionally been associated with occupational dermatitis,29 the most likely explanation is that the difference in the degree of sensitization is due to the distribution of professions in each study population. In fact, we can see a clear correlation in the series analyzed: sensitization to chrome is more frequent in those with a higher percentage of occupational dermatitis than in those with a lower percentage of occupational dermatitis (Tables 3 and 4).
LimitationsFirst, this study was performed at a single center, and the relevance of the allergens was determined based on the clinical history.
Second, it is difficult to compare data between the different studies owing to the lack of studies performed during the same period in the Spanish medical literature and the absence of publicly available data on the distribution of the working population by province.
Lastly, it is important to remember that changes in the composition of the Spanish standard series in 2012 and 2016 mean that certain allergens were only assessed during specific parts of the study period.
ConclusionsFindings for the allergens analyzed in the present series are increasingly consistent with those for the allergens that most frequently lead to sensitization in Spain, especially, nickel, MCl/MI, methylisothiazolinone, and paraphenylenediamine.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We are grateful to Jesús María González-Martín, a biostatistician at the Research Unit of Complejo Hospitalario Universitario Insular Materno Infantil, for his advice on the statistical analysis.